In recent years, the scientific community has watched with growing interest as China has emerged as a global leader in regenerative medicine. Nowhere is this more evident than in the latest developments surrounding stem cell therapy and its potential role in reversing chronic diseases, including autoimmune conditions such as type 1 diabetes. With new clinical trials making international headlines and major biomedical institutions in China making bold claims, many are asking: Could the latest stem cell research mark a true turning point in the search for a type 1 diabetes cure?
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
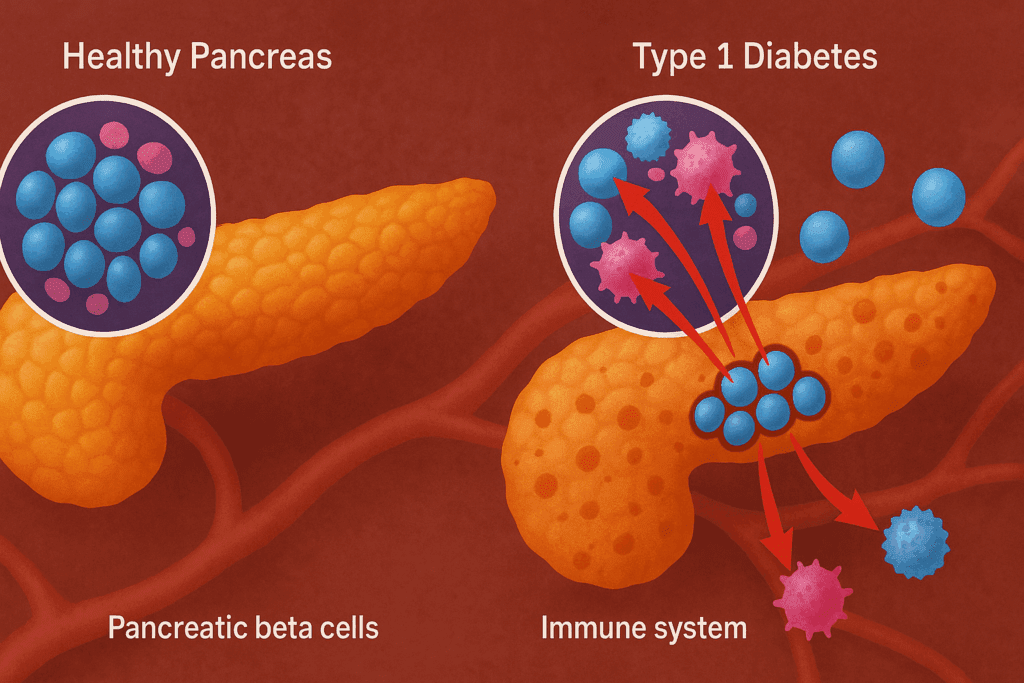
Type 1 diabetes, an autoimmune condition where the body’s immune system mistakenly attacks insulin-producing beta cells in the pancreas, affects millions worldwide. Unlike type 2 diabetes, which can often be managed or reversed with lifestyle changes, type 1 diabetes typically requires lifelong insulin therapy. But in a stunning series of recent developments, researchers in China claim they are getting closer to a functional cure through advanced stem cell technology. For many patients and families affected by this lifelong condition, the question “Can type 1 diabetes be reversed?” is no longer purely theoretical—it is now a matter of active scientific inquiry.
Understanding the Scientific Landscape of Type 1 Diabetes
To grasp the implications of this research, it’s essential to understand the biology of type 1 diabetes. In this disease, the immune system targets and destroys beta cells in the pancreas, eliminating the body’s ability to produce insulin. Insulin is critical for regulating blood glucose, and without it, individuals face life-threatening complications. While synthetic insulin and continuous glucose monitoring technologies have improved patient outcomes, these remain management strategies, not cures.
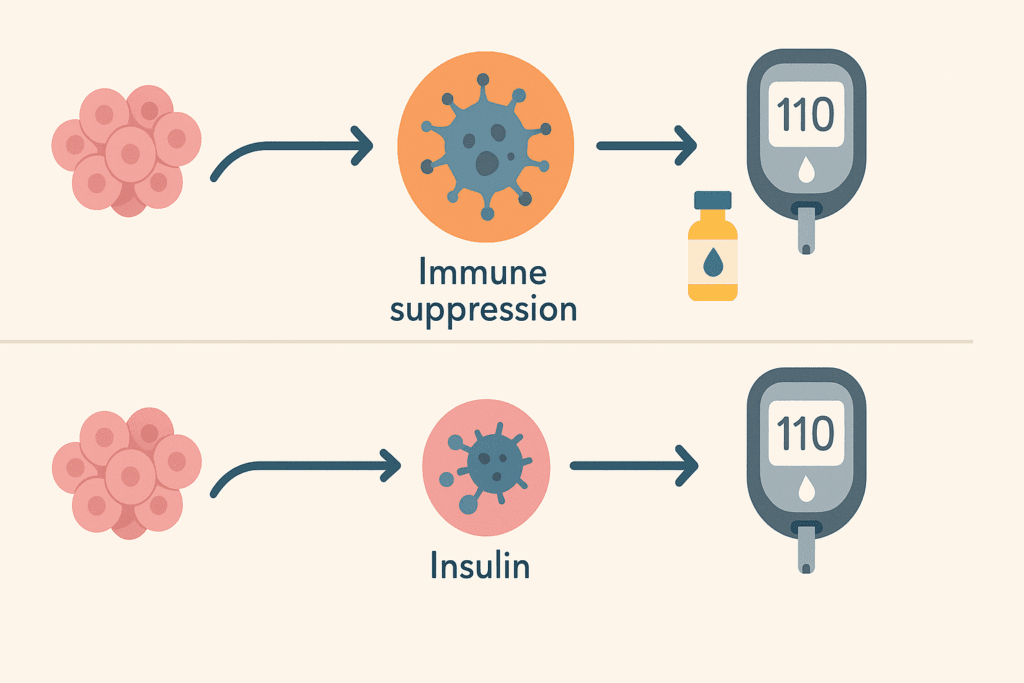
The interest in whether type 1 diabetes can be cured permanently stems from a desire to regenerate or replace these lost beta cells. Historically, pancreas transplants or islet cell transplantation were explored, but both methods come with significant limitations, including the need for immunosuppressive drugs and donor shortages. The concept of using stem cells to grow new insulin-producing cells offers a more scalable, less invasive alternative. As researchers continue to explore this field, the latest news on type 1 diabetes cure efforts is dominated by countries investing heavily in biotechnology—chief among them, China.
Why China Is Leading the Charge in Stem Cell Research
China’s rise in stem cell innovation is not accidental. Over the past decade, the country has invested billions into regenerative medicine, creating a research environment with fewer bureaucratic hurdles and more rapid clinical trial development than many Western nations. Institutions such as the Guangzhou Institutes of Biomedicine and Health and the Chinese Academy of Sciences have received global recognition for their groundbreaking work. As the world searches for a miracle cure for diabetes, eyes are turning to China’s laboratories, where early-stage results are suggesting that stem cell therapy may succeed where other approaches have faltered.
A key aspect of China’s approach has been the use of induced pluripotent stem cells (iPSCs)—cells that can be reprogrammed into any cell type, including insulin-producing beta cells. These cells can be derived from a patient’s own tissue, reducing the likelihood of immune rejection. In the most recent studies, Chinese scientists have demonstrated that these iPSCs can successfully mature into beta-like cells in lab environments and, when implanted in mice, regulate blood glucose levels over extended periods.
The headline-grabbing news that “China develops stem cell diabetes cure” is rooted in this work. But it’s important to temper excitement with rigorous scientific scrutiny. While the potential is extraordinary, clinical trials in humans are still in early phases. Nevertheless, these trials are progressing rapidly, leading many to wonder if China’s aggressive innovation pipeline may help answer the long-standing question: Is type 1 diabetes reversible?
Evaluating the Validity of Cure Claims
The phrase “type 1 diabetes cured” understandably draws both hope and skepticism. As with any groundbreaking medical claim, validation through peer-reviewed research, long-term follow-up, and transparency in trial design are essential. In China’s case, multiple trials have entered phase 2, showing promising early results. Patients receiving stem cell-derived beta cells have reportedly reduced or even eliminated their need for insulin injections over the short term. For individuals who have long asked, “Can you get rid of diabetes type 1 with regenerative therapies?”—these findings are deeply encouraging.
However, reversing diabetes 1 permanently requires more than restoring insulin production. A true cure must also address the underlying autoimmune response that caused the condition in the first place. Some research teams in China are now combining stem cell therapy with immunomodulatory treatments to reduce autoimmune activity. This dual approach aims to not only replace damaged cells but also to prevent future immune attacks. The integration of stem cells and diabetes immunotherapy may ultimately hold the key to how to cure type 1 diabetes permanently.
Global Response and Scientific Scrutiny
China’s progress has not gone unnoticed by the global medical community. Leading endocrinologists and immunologists have praised the technical sophistication of Chinese stem cell research while calling for greater collaboration and data transparency. Journals like Nature Biotechnology and The Lancet Diabetes & Endocrinology have published editorials encouraging more rigorous, multi-site international trials. As excitement builds around the question, “Will type 1 diabetes be cured in our lifetime?”, experts caution that any stem cell solution must meet global standards of safety, efficacy, and replicability.
One of the challenges in evaluating the claim that stem cells are curing diabetes is the variability in patient outcomes. Not all patients respond equally, and factors such as age, disease duration, and immune profile play a critical role in success rates. Furthermore, while short-term results are encouraging, longer-term studies are needed to assess the durability of beta cell function and the risk of immune rejection or tumor formation.

The Promise and Limitations of Stem Cell Therapy
To fully appreciate the impact of stem cell treatment for diabetes, it is important to distinguish between partial remission and a complete cure. For many patients, even a partial reduction in insulin dependence can dramatically improve quality of life. In recent news on type one diabetes, several Chinese trials have reported that patients were able to maintain stable glucose levels without insulin for periods ranging from several weeks to months—a significant achievement, albeit not yet a definitive cure.
For those wondering, “Where can I get stem cell treatment for diabetes?”, the answer increasingly includes clinics in China. However, patients must exercise caution. The field is still evolving, and not all facilities meet the rigorous ethical and scientific standards required for such experimental therapies. Reputable hospitals affiliated with university research centers are the most reliable sources of cutting-edge treatments, but international access is still limited.
There is also the question of whether stem cell type 1 diabetes therapies will eventually become affordable and scalable. Unlike pharmaceutical solutions, which can often be mass-produced, stem cell procedures are labor-intensive and personalized, presenting logistical challenges for widespread implementation. Nonetheless, if China continues to lead in this space, it may help drive innovation and cost reductions that make these therapies more accessible globally.
Comparing China’s Approach with Western Research Initiatives
While China is making headlines for its bold advances, researchers in the U.S., Europe, and Japan are also exploring the same frontier. Companies like Vertex Pharmaceuticals and ViaCyte in the U.S. are conducting trials involving encapsulated stem cell-derived beta cells that aim to avoid immune rejection. Yet many Western initiatives face stricter regulatory frameworks that slow down the transition from laboratory to clinic.
This contrast has led some to argue that China’s regulatory flexibility gives it a distinct advantage in the race for a T1D cure. However, it also places a greater burden on Chinese researchers to ensure safety and transparency. As global awareness of China’s work grows, so does the demand for open data sharing, peer-reviewed publications, and collaborative trials that include diverse populations.
In the end, the question is not just “Is there a cure for type 1 diabetes?” but “How can we ensure that such a cure is safe, ethical, and accessible to all who need it?” The answer will likely depend on sustained international cooperation and investment in long-term clinical validation.
Ethical Considerations in the Pursuit of a Diabetes Cure
While the scientific excitement is palpable, the ethical landscape surrounding stem cell therapy remains complex. Critics argue that some clinics may exploit the hopes of vulnerable patients by offering unproven therapies at high costs. In a field flooded with interest in a potential juvenile diabetes cure, maintaining rigorous standards is essential to protect patients from harm and misinformation.
Chinese regulatory agencies have begun to tighten oversight of clinical trials, requiring stricter approvals and compliance with international best practices. Meanwhile, international watchdogs are advocating for clearer guidelines on what constitutes legitimate research versus commercial exploitation. For patients searching phrases like “can type one diabetes be cured” or “is there any cure for type 1 diabetes,” access to medically accurate, up-to-date information is crucial.
It is also vital to ensure that any future cure does not exacerbate health inequities. Without deliberate policy planning, novel therapies may initially be available only to wealthy patients or those in major urban centers. Making the promise of a diabetes cure equitable will require attention not just to science but also to social justice and global health systems.
Looking Ahead: What This Means for Patients and Practitioners
For endocrinologists, diabetes educators, and caregivers, the pace of recent discoveries offers both hope and a challenge. Keeping up with the latest news on type 1 diabetes cure strategies requires ongoing education and adaptability. As new therapies move from trial to practice, clinicians must be prepared to evaluate emerging data, guide patient expectations, and integrate new treatment protocols into everyday care.
Patients, too, are empowered by access to better information and a more hopeful outlook. When someone searches, “Can you reverse type 1 diabetes?” or “Can diabetes 1 be reversed with stem cells?”—they’re now encountering a growing body of research that suggests reversal may not be just a dream. However, distinguishing between early-stage breakthroughs and clinically proven therapies remains essential.
Above all, the evolving narrative about stem cells curing diabetes underscores a larger truth: medical innovation is often nonlinear. Success is usually incremental, built on decades of foundational work, failed trials, and scientific debate. But sometimes, the pace accelerates, and breakthroughs that once seemed decades away begin to materialize. Many now believe we are entering such a moment.
Frequently Asked Questions: Stem Cells and the Future of Type 1 Diabetes Treatment
1. How does China’s approach to stem cell therapy differ from Western methods in the search for a type 1 diabetes cure?
China’s approach to regenerative medicine is notably more agile due to its expedited regulatory processes and state-supported infrastructure, giving researchers a competitive edge in translating lab findings to clinical trials. While Western institutions often encounter prolonged approval timelines, China can rapidly implement stem cell therapies in pilot studies, which may partly explain the surge in type 1 diabetes news coming from Chinese labs. In particular, the way China develops stem cell diabetes treatments reflects an integrated approach combining biotechnology, artificial intelligence, and genetic engineering. This comprehensive strategy positions the country as a major innovator in what some call the emerging frontier of a diabetes cure. Although caution is warranted, especially regarding oversight, China’s ecosystem for medical innovation is contributing significantly to the latest news on type 1 diabetes cure efforts worldwide.
2. Can you reverse type 1 diabetes through lifestyle changes alone?
Unlike type 2 diabetes, which can often be controlled or even reversed with significant lifestyle modifications, reversing type 1 diabetes requires more than diet and exercise. Because this autoimmune condition results in the destruction of insulin-producing beta cells, external interventions such as immunotherapy or stem cell transplantation are typically necessary. While improved lifestyle habits can enhance glucose control and reduce complications, they do not regenerate lost beta cell function. For those wondering whether type 1 diabetes is reversible without medical intervention, the answer remains firmly grounded in science: a holistic strategy may help manage the disease but cannot replace the need for targeted therapeutic approaches like those being developed in China. Therefore, discussions around how to cure type 1 diabetes permanently increasingly center on biomedical innovation, not solely behavioral change.
3. What practical challenges exist for implementing stem cell therapy in everyday diabetes care?
Despite promising headlines like “China develops stem cell diabetes breakthrough,” several practical barriers must be overcome before stem cell therapy becomes part of routine care. Manufacturing stem cell products at scale while ensuring purity, safety, and functionality remains technically demanding. Additionally, the question of where can I get stem cell treatment for diabetes brings up issues of access, affordability, and regulatory approval, especially across different healthcare systems. Even if stem cell-derived beta cells prove safe and effective, long-term monitoring, potential immune rejection, and the risk of cellular overgrowth require meticulous management. These real-world considerations mean that while the science advances, healthcare infrastructure must evolve in tandem to support broader use.
4. What distinguishes a functional cure from a complete cure in the context of type 1 diabetes?
When discussing whether type 1 diabetes is cured, it’s essential to distinguish between a functional and a complete cure. A functional cure means that individuals no longer require insulin injections and maintain stable glucose levels, but their immune system may still harbor autoimmune tendencies. A complete cure, on the other hand, would not only restore insulin production but also eliminate the underlying immune dysfunction. Currently, the most advanced stem cell type 1 diabetes trials aim to achieve functional remission, with some patients showing reduced insulin dependency for months. As the search continues for how to reverse diabetes 1 completely, researchers are increasingly focused on combining beta cell replacement with immune system modulation to prevent relapse.
5. Are there ethical concerns surrounding the development of a juvenile diabetes cure using stem cells?
Yes, ethical considerations are central to the pursuit of a juvenile diabetes cure via stem cell technologies. These concerns include the sourcing of stem cells, the oversight of clinical trials involving children, and the equitable distribution of future treatments. The promise of a miracle cure for diabetes should not overshadow the importance of informed consent and long-term safety monitoring, especially in vulnerable populations. Furthermore, disparities in healthcare access may limit the availability of advanced treatments to wealthier regions or patients, raising global equity questions. As China develops stem cell diabetes strategies, ensuring ethical transparency and regulatory consistency remains a critical priority for both national and international stakeholders.
6. How realistic is the goal of curing type 1 diabetes with stem cells in the next decade?
While the pace of research is accelerating, particularly with diabetes cure China headlines making waves, a definitive cure within the next decade remains an ambitious goal. Current evidence supports the potential for partial reversal, or at least a dramatic reduction in insulin dependency. For those asking, “Can type one diabetes be cured soon?”, the answer lies in bridging promising lab data with long-term, peer-reviewed clinical trials. The translation from experimental to mainstream medicine typically spans many years due to safety protocols and regulatory checkpoints. Nevertheless, the rapid evolution of stem cells and diabetes research suggests that significant therapeutic progress could indeed be realized within the next ten years, even if full reversal remains a longer-term aspiration.
7. What are the long-term risks associated with stem cell-based therapies for type 1 diabetes?
Long-term safety remains a paramount concern in stem cell-based interventions, particularly when dealing with autoimmune conditions. Potential risks include immune rejection, unintended cell differentiation, and in rare cases, the formation of tumors. While China’s leading institutions are working to mitigate these risks by refining cell purification techniques and using autologous (self-derived) stem cells, the clinical landscape is still evolving. It is too early to definitively say whether stem cells curing diabetes will avoid these long-term complications altogether. As the body of type 1 diabetes news grows, so too does the need for continuous monitoring and outcome transparency in every patient cohort.
8. What role does genetic profiling play in the success of stem cell therapy for diabetes?
Genetic profiling is increasingly recognized as a critical factor in determining which patients might benefit most from emerging therapies. By analyzing a person’s immune profile, beta cell function, and genetic predisposition to autoimmunity, clinicians can better predict how a patient will respond to treatments like stem cell transplantation. This is particularly relevant in efforts to reverse diabetes 1, where individual variability significantly affects outcomes. With precision medicine gaining momentum, the integration of genomics into diabetes treatment may enhance the safety and efficacy of next-generation therapies. As China develops stem cell diabetes protocols, personalized medicine is likely to become a core component of their clinical trial design.
9. How are global collaborations shaping the future of type 1 diabetes treatment?
The international nature of stem cell research means that progress is rarely confined within borders. Collaborations between Chinese institutions and Western universities are beginning to bridge gaps in data sharing, patient recruitment, and regulatory harmonization. This cross-pollination of ideas is driving a more unified strategy to answer persistent questions like “Can you reverse type 1 diabetes effectively?” and “Is type one diabetes reversible with immune protection?” Multinational clinical trials and co-authored scientific papers are accelerating the credibility and reach of new treatment options. By combining China’s rapid trial infrastructure with Western oversight rigor, the global medical community may get closer to a consensus answer for whether type 1 diabetes can be cured.
10. What lifestyle considerations remain important even with emerging T1D cures on the horizon?
Even as research advances toward a potential T1D cure, lifestyle factors remain foundational to overall health. Exercise, a nutrient-rich diet, and stress management will continue to support metabolic balance and cardiovascular health, especially for patients in partial remission. Those exploring whether type 1 diabetes is reversible often benefit from lifestyle measures that enhance the body’s resilience and may even improve the effectiveness of regenerative therapies. Moreover, sustained health-conscious behaviors can reduce comorbid risks like kidney disease, neuropathy, and eye complications, which are not necessarily resolved even if beta cell function is restored. In the evolving conversation around stem cell type 1 diabetes therapies, personal health practices remain an indispensable part of the equation.
A New Era in Diabetes Care: Is a Functional Cure Finally Within Reach?
As we reflect on the rapid advancements in regenerative medicine, it becomes clear that the answer to questions like “Can type I diabetes be cured?” or “Is type one diabetes reversible?” may soon shift from theoretical to practical. With China at the forefront of this research renaissance, we are witnessing a global reimagining of what is possible in diabetes care.
The integration of stem cells and diabetes treatment is not just a scientific curiosity—it represents a potential paradigm shift. Patients who once had no hope of regaining pancreatic function are now participating in trials that may restore insulin independence. While the journey is far from over, the evidence is mounting that stem cell technology could one day deliver a lasting solution.
For now, we must proceed with cautious optimism. Stem cell breakthroughs in China have injected new energy into a field that had long been defined by management, not cure. If these efforts continue to bear fruit, the dream of a T1D cure could soon become reality—not just a medical headline, but a new chapter in the lives of millions who have waited too long for a permanent answer.
Further Reading:
Stem-cell therapy reverses type 1 diabetes in groundbreaking case study
Groundbreaking Stem Cell Therapy Offers New Hope for Type 1 Diabetes: A Medical Breakthrough
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


