Type 1 diabetes is a chronic condition that affects millions of children worldwide. While it is often diagnosed in early childhood or adolescence, the journey to diagnosis can be long and challenging for many families. Unlike type 2 diabetes, which is often preventable through lifestyle changes, type 1 diabetes is an autoimmune condition where the body mistakenly attacks the insulin-producing cells in the pancreas. This leads to a lack of insulin, a hormone necessary for regulating blood sugar levels. While there is no cure for type 1 diabetes, understanding the early signs, symptoms, and triggers can help parents, caregivers, and educators identify the disease early, ensuring timely intervention and management. This article delves into the early signs of diabetes in kids, the symptoms of type 1 diabetes, and what triggers the condition, with the aim of providing a thorough understanding of this serious health issue.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
What is Type 1 Diabetes?
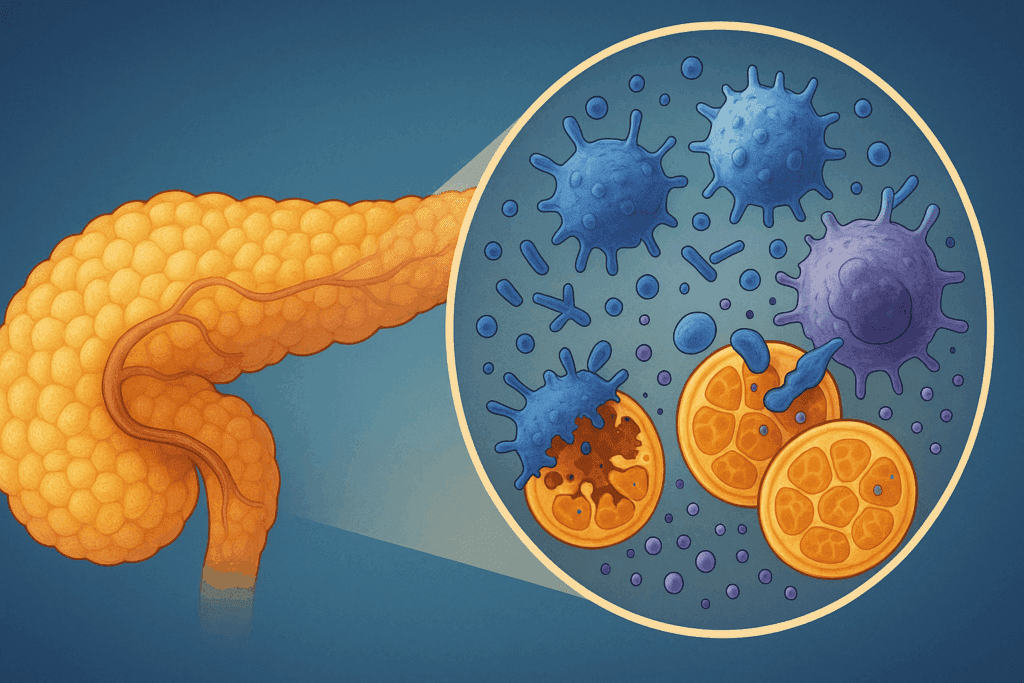
Before discussing the signs and symptoms, it’s important to understand what type 1 diabetes is. Type 1 diabetes is a condition in which the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas. This results in the inability to produce insulin, a hormone necessary to convert glucose from food into energy. While the exact cause is unknown, researchers suggest that genetic factors and environmental triggers, such as viral infections, may contribute to the development of type 1 diabetes. Unlike type 2 diabetes, which is often linked to obesity and lifestyle factors, type 1 diabetes is not preventable, and its onset can occur at any age, although it is most commonly diagnosed in children and young adults.
The severity of type 1 diabetes can vary from person to person, but all individuals with the condition require insulin therapy for survival. Insulin is typically administered through injections or an insulin pump to regulate blood sugar levels. As of today, there is no cure for type 1 diabetes, making early detection and ongoing management essential to prevent complications such as diabetic ketoacidosis, a potentially life-threatening condition that can arise when the body becomes too acidic due to high blood sugar levels.

Signs of Type 1 Diabetes in Children
Identifying type 1 diabetes in children can be difficult, especially since many of its symptoms are often mistaken for other common childhood illnesses. However, early recognition is crucial for effective management and preventing severe complications. The following are some of the most common signs of diabetes in kids that parents should be aware of:
Increased Thirst and Urination
One of the earliest signs of type 1 diabetes in children is increased thirst, also known as polydipsia. When blood sugar levels become too high, the kidneys work overtime to filter and absorb the excess sugar, which leads to dehydration. This causes children to feel excessively thirsty, often prompting them to drink large amounts of water. As a result, they may urinate more frequently, a condition known as polyuria. These symptoms can sometimes be overlooked or misattributed to a urinary tract infection or other common childhood conditions.
Extreme Hunger
Another sign of type 1 diabetes in children is extreme hunger, or polyphagia. Despite eating regular meals, children with type 1 diabetes often feel hungry all the time. This is because the body cannot properly process glucose without enough insulin. Since the cells are unable to receive the energy they need from glucose, the body signals an increase in hunger in an attempt to compensate.
Fatigue and Weakness
Children with type 1 diabetes may experience significant fatigue or weakness. This occurs because their bodies are unable to use glucose for energy, which leaves them feeling tired and drained. Fatigue can manifest as an unwillingness to engage in regular activities, difficulty staying awake during the day, or trouble concentrating at school. If this fatigue persists despite rest, it could be a sign of an underlying health issue such as diabetes.
Weight Loss
While weight loss is often associated with type 2 diabetes, it can also be a prominent symptom in children with type 1 diabetes. This happens because the body, unable to use glucose due to insufficient insulin, starts to break down muscle and fat for energy. As a result, children may experience unintentional weight loss, even if their appetite has increased.
Blurred Vision
High blood sugar levels can lead to fluid being drawn from the lenses of the eyes, which affects the ability to focus. This may cause blurry vision, a symptom that can go unnoticed at first but can eventually lead to difficulty seeing clearly. If a child experiences persistent blurred vision, it is important to consult a healthcare provider to determine the underlying cause.
Mood Changes and Irritability
Children with type 1 diabetes may experience mood swings and irritability, which can be linked to fluctuating blood sugar levels. Both high and low blood sugar levels can affect a child’s behavior, causing them to become more easily upset, anxious, or lethargic. This is often compounded by the frustration of managing the disease, as children struggle with the restrictions and changes it imposes on their daily lives.

Symptoms of Type 1 Diabetes: A Closer Look
The symptoms of type 1 diabetes in children typically develop over a short period, often just days or weeks. In some cases, the symptoms can escalate quickly, leading to a medical emergency. This makes it all the more important to recognize the symptoms early. Apart from the aforementioned signs, there are several other symptoms that may indicate type 1 diabetes:
Breath That Smells Fruity or Sweet
A fruity or sweet-smelling breath is a classic sign of diabetic ketoacidosis (DKA), a dangerous complication of type 1 diabetes. DKA occurs when the body starts breaking down fat for energy due to the lack of insulin, leading to the accumulation of ketones in the blood. These ketones cause the breath to take on a fruity or acetone-like odor. If a child’s breath smells this way, immediate medical attention is necessary.
Nausea and Vomiting
When blood sugar levels rise significantly, the body tries to flush out excess glucose by increasing urine production. This can lead to dehydration, which in turn causes nausea and vomiting. These symptoms are more commonly associated with DKA, which can be life-threatening if not treated promptly. If left untreated, dehydration can worsen, causing a child to become confused, lethargic, or even unconscious.
Dry Mouth and Skin
Dry mouth and skin are common symptoms of dehydration, which is a result of the body’s inability to retain water due to high blood sugar levels. Children with type 1 diabetes may also have dry, cracked lips and skin that feels tight or rough. Dehydration can further contribute to the other symptoms of type 1 diabetes, such as fatigue and weakness.
What Triggers Type 1 Diabetes?
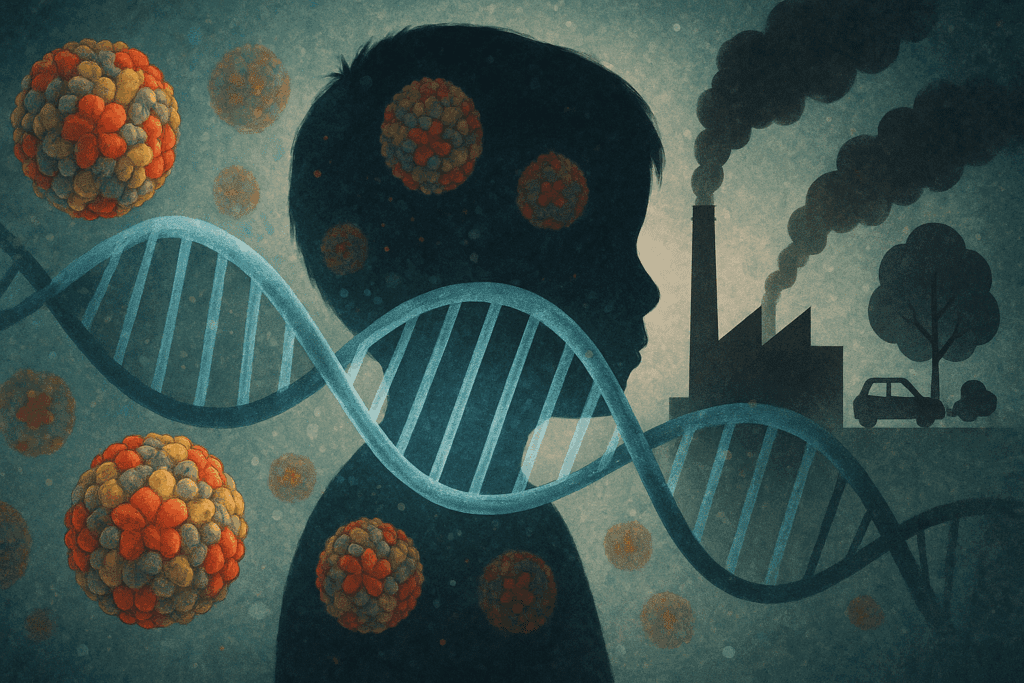
The exact cause of type 1 diabetes remains unclear, but experts believe it is triggered by a combination of genetic and environmental factors. These triggers lead to an autoimmune response in which the body attacks its own insulin-producing beta cells. Understanding the potential triggers can help provide insight into why type 1 diabetes develops in some children and not others.
Genetics and Family History
One of the most significant factors in developing type 1 diabetes is genetics. Research has shown that children who have a first-degree relative with type 1 diabetes (such as a parent or sibling) are at a higher risk of developing the condition. Specific genes, particularly those related to the immune system, have been identified as playing a role in the development of type 1 diabetes. However, genetics alone does not account for the entire risk; environmental factors must also be considered.
Viral Infections
Certain viral infections have been linked to the onset of type 1 diabetes. Viruses such as enteroviruses, mumps, and rubella may trigger an autoimmune response in genetically predisposed individuals. These infections may damage the insulin-producing cells in the pancreas, ultimately leading to type 1 diabetes. While viral infections do not directly cause the disease, they can act as triggers for its development.
Environmental Factors
Environmental factors, such as exposure to certain chemicals or toxins, may also play a role in triggering type 1 diabetes. Some studies have suggested that early childhood exposure to environmental toxins or an imbalance in gut bacteria may increase the risk of developing the disease. Additionally, diet and lifestyle factors, although less directly linked to type 1 diabetes than type 2, may contribute to the disease’s onset in genetically predisposed children.

How Type 1 Diabetes Is Diagnosed
Diagnosing type 1 diabetes in children involves a combination of medical history, physical exams, and blood tests. Healthcare providers typically look for the classic signs and symptoms of the condition, such as increased thirst, urination, and fatigue. A blood test is then performed to measure blood glucose levels. If blood sugar levels are significantly elevated, additional tests may be conducted to confirm the diagnosis, including tests for ketones, which are often present in cases of DKA.
Doctors may also perform an autoantibody test to check for antibodies that attack the pancreas’s insulin-producing cells. This test helps confirm that the body’s immune system is responsible for the destruction of the pancreas cells. In some cases, genetic testing may also be used to assess a child’s risk of developing type 1 diabetes, particularly if there is a family history of the condition.
Frequently Asked Questions (FAQ) About Type 1 Diabetes in Children
Can Type 1 Diabetes Be Cured?
Currently, there is no cure for type 1 diabetes. It is a lifelong condition that requires consistent management through insulin therapy, blood sugar monitoring, and lifestyle adjustments. While there are ongoing research efforts exploring potential cures, including advances in immunotherapy and stem cell research, the focus remains on improving treatment options and managing the condition effectively. Families with children diagnosed with type 1 diabetes can manage the disease well with proper care, ensuring that their child lives a healthy, active life despite the diagnosis.
What Are the Early Signs of Diabetes in Kids?
The early signs of diabetes in kids can be subtle but often include symptoms such as excessive thirst, frequent urination, extreme hunger, fatigue, and unintentional weight loss. If your child is constantly thirsty, drinking large amounts of water, and frequently needing to urinate, it might be a sign that their blood sugar levels are elevated. These symptoms arise because the body is trying to flush out excess glucose through urine. Other signs of diabetes in toddlers or children may include blurred vision and irritability. Identifying these signs early can help get the child diagnosed and treated sooner, reducing the risk of complications like diabetic ketoacidosis.
Can You Get Type 1 Diabetes Later in Life?
While type 1 diabetes is typically diagnosed in children and young adults, it is possible to be diagnosed with it as an adult, though it is less common. In some cases, adults may not show the classic symptoms of type 1 diabetes and could be misdiagnosed as having type 2 diabetes. However, both types of diabetes share some symptoms, and a proper diagnosis is essential. Type 1 diabetes in adults can present itself suddenly, and just like in children, the individual will need to manage it with insulin. A healthcare provider may conduct tests such as checking for antibodies or performing an oral glucose tolerance test to confirm the diagnosis.
Are You Born with Type 1 Diabetes?
Type 1 diabetes is not typically something that a person is born with. However, genetics can play a role in increasing the likelihood of developing it. Children who have a parent or sibling with type 1 diabetes have a higher chance of being diagnosed with the condition, but this does not guarantee it will happen. Environmental factors, such as viral infections, may trigger the autoimmune response that leads to type 1 diabetes. Therefore, while one might have a genetic predisposition, it is not accurate to say that a child is born with type 1 diabetes.
How Long Can a Child Have Diabetes Without Knowing?
It’s possible for a child to have type 1 diabetes for a while without showing any obvious signs or being diagnosed. In some cases, children may experience mild symptoms, which could be mistaken for other illnesses. Parents may not recognize the signs of diabetes in toddlers or children until the condition worsens. Without treatment, diabetes can cause long-term complications. If you suspect that your child might be at risk, it’s important to seek a medical evaluation to determine whether type 1 diabetes is the cause of their symptoms.
What Triggers Type 1 Diabetes?
The exact cause of type 1 diabetes is not fully understood, but it is believed to result from a combination of genetic and environmental factors. Certain viral infections, such as enteroviruses, have been linked to triggering the autoimmune response that leads to type 1 diabetes. Other potential triggers may include environmental factors, like early childhood exposure to toxins or imbalances in gut bacteria. While it is difficult to predict exactly what triggers type 1 diabetes in any given individual, understanding these potential factors can help guide future research into prevention and treatment options.
How Is Type 1 Diabetes Diagnosed?
Diagnosing type 1 diabetes involves a combination of clinical examination, medical history, and lab tests. A pediatrician may suspect type 1 diabetes if a child presents with symptoms like excessive thirst, urination, and unexplained weight loss. The most common diagnostic tests include a fasting blood glucose test or an oral glucose tolerance test. If blood sugar levels are abnormally high, further tests, including an antibody test, may be conducted to confirm that the body’s immune system is attacking the insulin-producing cells in the pancreas, which is characteristic of type 1 diabetes.
Can Type 1 Diabetes Be Prevented?
Unfortunately, there is no known way to prevent type 1 diabetes. The condition is largely driven by genetic factors and autoimmune responses that occur beyond an individual’s control. However, lifestyle factors such as maintaining a healthy diet and managing stress can play a role in managing overall health, though they cannot prevent the onset of type 1 diabetes. For families with a history of diabetes, staying alert to the early signs of diabetes in children and seeking medical advice promptly can help manage the condition if it develops.
What Are the Complications of Type 1 Diabetes?
Diabetes mellitus type 1 complications can affect various parts of the body, especially when blood sugar is not well managed. Long-term high blood sugar levels can lead to complications such as kidney disease, nerve damage, and eye problems, including diabetic retinopathy. Additionally, children and adults with type 1 diabetes are at higher risk of developing heart disease and experiencing stroke. One of the most immediate complications, especially if diabetes is not diagnosed early, is diabetic ketoacidosis, a life-threatening condition that requires urgent medical attention.
Does Type 1 Diabetes Go Away?
No, type 1 diabetes does not go away. Once diagnosed, it is a lifelong condition that requires ongoing management. However, with proper insulin therapy, diet, exercise, and regular monitoring, children and adults with type 1 diabetes can lead full and active lives. While there are no cures for type 1 diabetes, advancements in treatment, such as the development of continuous glucose monitoring systems and insulin pumps, have greatly improved the quality of life for those with the disease. Research continues to explore potential cures, but for now, managing type 1 diabetes is the key to living well with the condition.
Conclusion: Living with Type 1 Diabetes
Type 1 diabetes is a lifelong condition that requires constant management, but with early detection and proper treatment, children with the disease can lead healthy, active lives. While there is currently no cure for type 1 diabetes, advancements in research continue to provide new hope for better treatments and potential breakthroughs. By understanding the early signs and symptoms of diabetes, parents and caregivers can act quickly to get the appropriate medical care for their children. Early diagnosis and intervention are crucial in preventing complications such as diabetic ketoacidosis and ensuring that children with type 1 diabetes can live full and fulfilling lives.
Further Reading:
Type 1 diabetes – Symptoms and causes
How does diabetes affect children and teenagers?
Understanding Type 1 Diabetes: What Parents Should Know
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.