Introduction: A New Era in Diabetes Research
Type 2 diabetes remains one of the most widespread and complex chronic diseases affecting millions of individuals worldwide. Despite decades of research and medical advances, a definitive cure has remained elusive. However, recent scientific progress has begun to challenge the status quo, offering fresh hope and transformative possibilities for both patients and practitioners. With researchers uncovering groundbreaking pathways, refining genetic therapies, and reimagining metabolic regulation, the medical community is inching closer to what many are calling a genuine diabetes cure breakthrough.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
Amid the excitement of these developments, it’s important to distinguish between temporary remission and a lasting cure. The distinction becomes especially relevant when evaluating each new type 2 diabetes cure breakthrough, which often captures headlines but requires careful scrutiny for long-term effectiveness. As we explore the latest scientific discoveries and technologies, the question arises: Are we truly on the brink of a type 2 diabetes breakthrough, or is this still a vision of the future?
This article takes a comprehensive look at where diabetes research stands today, the promising treatments under development, and what recent clinical trials are revealing. We will explore not only the science but also the human element—the individuals living with diabetes who may soon benefit from innovations that could redefine what it means to manage, reverse, or potentially cure the disease.
Understanding Type 2 Diabetes: A Metabolic Puzzle
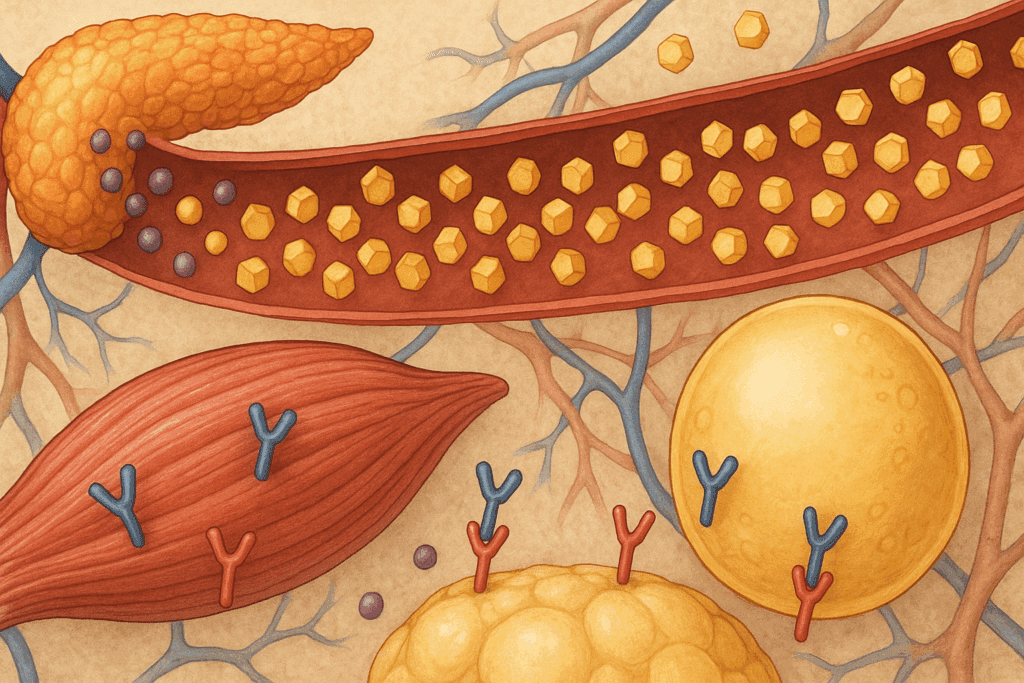
Type 2 diabetes is not a singular condition but a constellation of metabolic dysfunctions. At its core lies the body’s impaired ability to use insulin effectively, known as insulin resistance. Over time, this resistance leads to rising blood glucose levels, causing the pancreas to overproduce insulin in a desperate attempt to regulate sugar. Eventually, pancreatic beta cells can become exhausted, reducing insulin production and worsening the condition.
Unlike type 1 diabetes, which involves autoimmune destruction of insulin-producing cells, type 2 diabetes is closely tied to lifestyle factors such as diet, obesity, and inactivity—though genetic predispositions and environmental influences also play significant roles. This multifactorial nature makes the disease particularly difficult to cure, requiring a multifaceted approach that addresses not only glucose control but also inflammation, hormone regulation, and even gut microbiota.
In recent years, the understanding of type 2 diabetes has deepened, revealing that the disease operates on a cellular level far beyond just insulin and glucose. Mitochondrial function, inflammatory cytokines, and even epigenetic changes are now being studied as contributing factors. This expanded view is paving the way for more targeted interventions and is central to the latest type 2 diabetes breakthrough efforts.
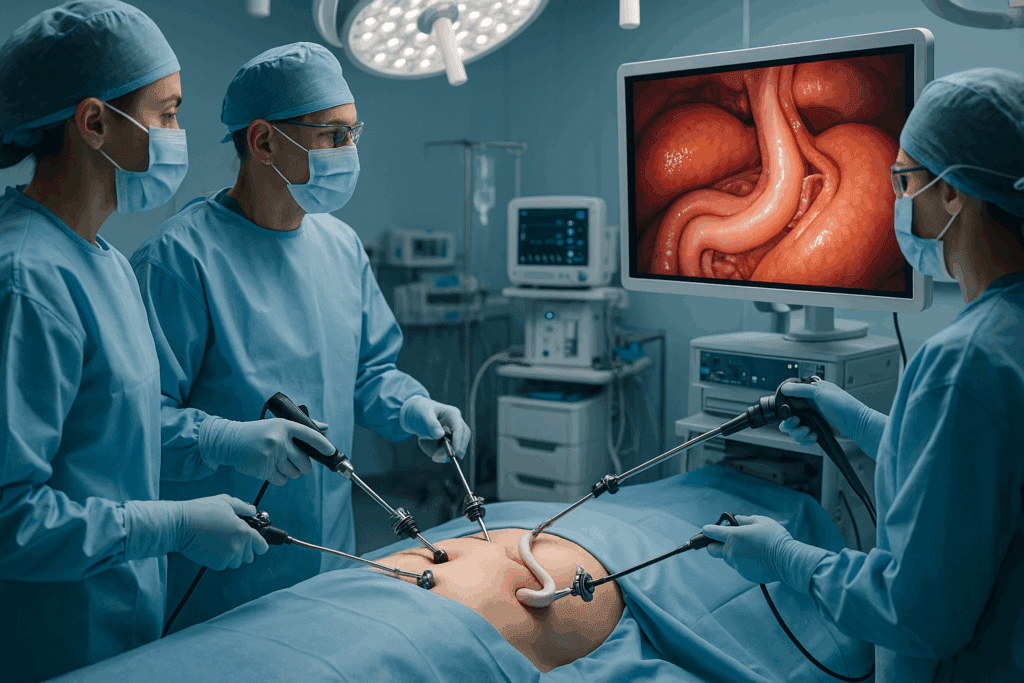
Metabolic Surgery and Diabetes Remission: A Surgical Path to Reversal
Among the most striking developments in recent years is the role of metabolic surgery in inducing long-term remission of type 2 diabetes. Procedures like gastric bypass and sleeve gastrectomy were initially developed for weight loss but have shown remarkable effectiveness in reducing blood glucose levels, sometimes even before substantial weight loss occurs. This has led many researchers to believe that these surgeries impact gut hormones, bile acids, and microbial populations in ways that enhance insulin sensitivity.
Studies have shown that patients undergoing metabolic surgery often experience dramatic improvements in blood sugar control, with many achieving remission that lasts for years. While not universally effective or suitable for every patient, these findings have sparked renewed interest in the mechanisms behind surgical interventions. Understanding how these procedures alter metabolism may provide insights into non-surgical therapies that mimic the same effects.
Despite its success, surgery is not a cure per se. It is an invasive intervention with potential complications and is best reserved for those with severe obesity or poorly controlled diabetes. Still, the insights gleaned from these procedures are contributing significantly to the broader search for a diabetes cure breakthrough by informing pharmaceutical and nutritional strategies.

Targeting the Gut Microbiome: A Revolutionary Frontier
Another area gaining momentum in diabetes research is the gut microbiome—the complex community of trillions of bacteria residing in the digestive tract. These microbes influence everything from immune function to appetite regulation, and growing evidence suggests they also play a crucial role in insulin sensitivity and glucose metabolism.
Recent studies have shown that people with type 2 diabetes often have a disrupted microbial balance, known as dysbiosis. Specific strains of bacteria that promote inflammation or reduce the body’s ability to manage blood sugar appear to be more prevalent in diabetic individuals. In response, researchers are exploring ways to reshape the gut microbiome through dietary interventions, prebiotics, probiotics, and even fecal microbiota transplants.
What makes this approach particularly exciting is its potential to address root causes rather than symptoms. By fostering a healthier microbial environment, it may be possible to improve metabolic health sustainably. Several ongoing clinical trials are evaluating the efficacy of microbiome-based therapies, and some early results suggest promising pathways that could contribute to a type 2 diabetes cure breakthrough.
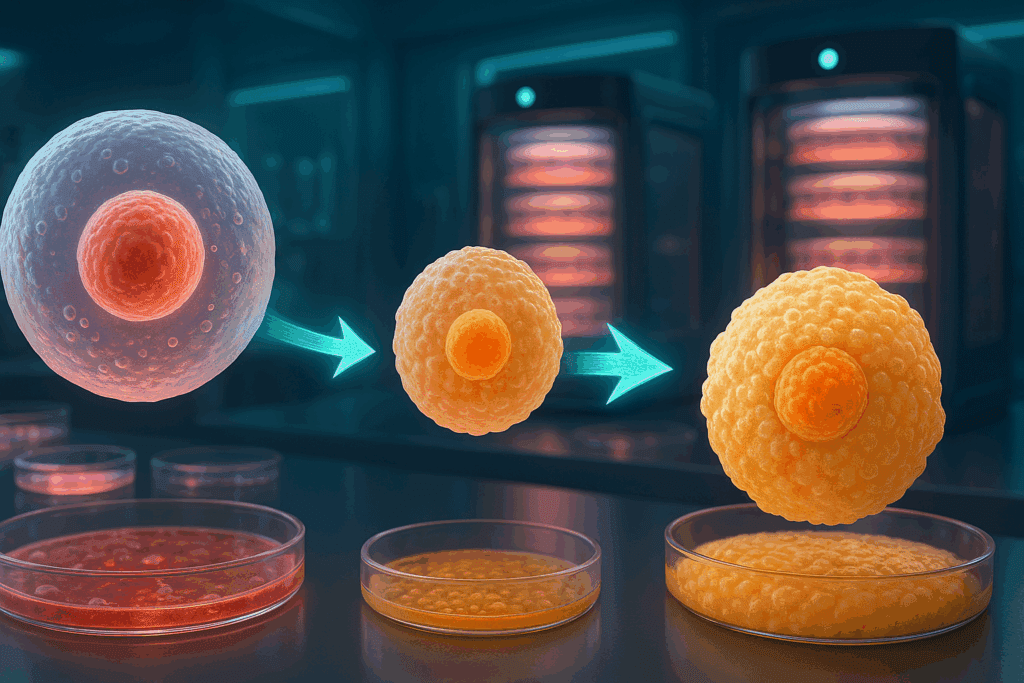
Cell-Based Therapies and Beta Cell Regeneration
One of the most transformative approaches in the search for a diabetes breakthrough involves regenerating the very cells responsible for insulin production. In both type 1 and type 2 diabetes, beta cell dysfunction is central to disease progression. Recent advances in stem cell research and cellular engineering are opening the door to therapies that could replenish these cells and restore normal glucose regulation.
Companies and academic institutions alike are investing heavily in developing lab-grown beta cells from pluripotent stem cells. These cells can then be transplanted into patients, theoretically restoring insulin production. Encapsulation technologies aim to protect these cells from immune attack, particularly relevant in type 1 diabetes, but potentially beneficial in advanced type 2 diabetes as well.
While this area has seen the most progress in t1d latest news, researchers are increasingly exploring its application to type 2 diabetes. By combining cell-based therapies with agents that reduce insulin resistance, there is growing optimism that a long-term solution may be achievable. These efforts represent a particularly hopeful avenue in the broader landscape of diabetes cure breakthroughs.
The Role of GLP-1 Agonists and Dual Hormone Therapies
Pharmaceutical advancements are also reshaping the treatment landscape. GLP-1 receptor agonists, such as semaglutide and liraglutide, have emerged as game-changing medications that not only lower blood glucose but also promote weight loss and cardiovascular health. These drugs mimic the action of a natural hormone that increases insulin secretion, slows gastric emptying, and reduces appetite.
More recently, dual and even triple hormone therapies have entered the scene, combining GLP-1 with other metabolic hormones such as GIP and glucagon. These next-generation treatments aim to replicate the body’s natural regulatory systems more closely, offering enhanced efficacy with fewer side effects. Clinical trials have shown impressive results in glycemic control, making them a centerpiece in the current type 2 diabetes breakthrough narrative.
While these therapies are not cures, they significantly improve disease management and may delay or prevent complications. By optimizing hormonal balance, they serve as both therapeutic and preventive tools, narrowing the gap between treatment and potential reversal. As new formulations and delivery mechanisms are developed, their role in the future of diabetes care is likely to expand further.
Genetic Editing and Precision Medicine: The CRISPR Revolution
Gene editing technologies, particularly CRISPR-Cas9, have introduced a new era of precision medicine in diabetes research. By enabling scientists to modify specific DNA sequences, CRISPR holds the promise of correcting genetic defects that contribute to insulin resistance or beta cell failure. Though most research to date has focused on monogenic forms of diabetes, efforts are underway to apply these techniques to more complex forms such as type 2 diabetes.
Recent experiments in animal models have successfully used CRISPR to improve insulin sensitivity and glucose metabolism by targeting genes involved in fat storage, inflammation, and mitochondrial function. These studies highlight the potential of genetic approaches to provide personalized and durable solutions. However, ethical considerations and long-term safety remain significant hurdles.
Still, the pace of innovation is accelerating. As our understanding of diabetes genetics deepens, and as gene editing tools become more refined, the potential for a true type 2 diabetes cure breakthrough becomes increasingly plausible. Though it may take years before these therapies become widely available, their implications for the future of diabetes treatment are profound.
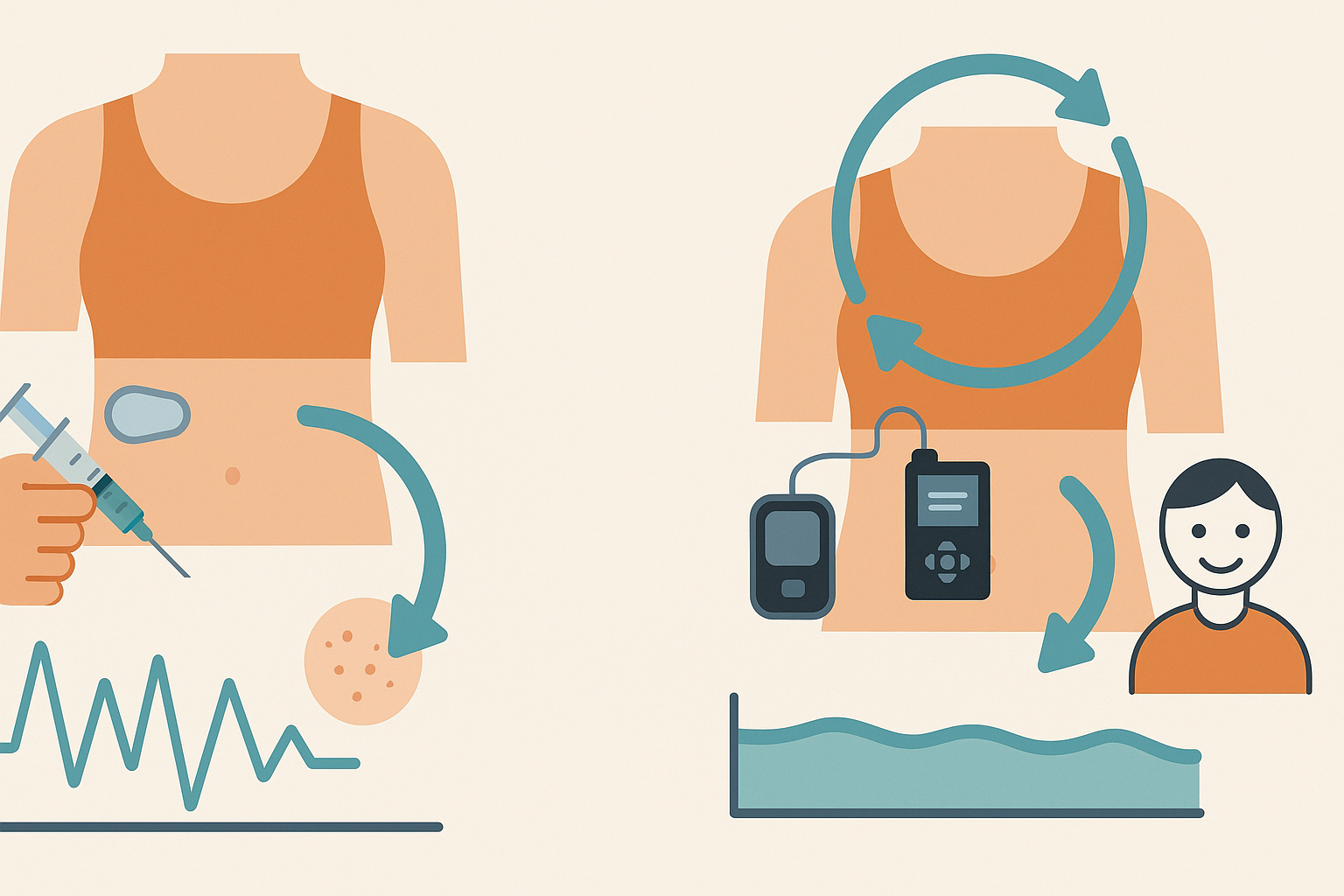
Artificial Pancreas Systems and Insulin Innovation
Technological innovations have also played a critical role in improving life with diabetes. Artificial pancreas systems—which integrate continuous glucose monitoring with insulin pumps and advanced algorithms—have revolutionized insulin delivery for people with type 1 diabetes and are increasingly being adapted for type 2 diabetes management.
These closed-loop systems provide real-time glucose readings and adjust insulin doses automatically, significantly reducing the burden of disease management. While not a cure, they offer near-physiological glucose control, reducing the risk of complications and improving quality of life. The expansion of these systems into type 2 diabetes care marks an important milestone in the pursuit of personalized, technology-driven solutions.
Parallel to these developments are innovations in insulin itself. Researchers are working on glucose-responsive insulins that activate only when blood sugar rises, minimizing the risk of hypoglycemia. Other formulations aim for once-weekly injections, offering greater convenience and adherence. Each insulin breakthrough brings us closer to an era where diabetes management is seamless and intuitive.
Environmental and Epigenetic Influences: Beyond Lifestyle
Emerging evidence suggests that environmental exposures and epigenetic modifications may contribute to the development and progression of type 2 diabetes. Factors such as endocrine-disrupting chemicals, chronic stress, and early-life nutritional status can alter gene expression in ways that predispose individuals to metabolic dysfunction.
Understanding these influences opens new avenues for prevention and intervention. Epigenetic therapies—which seek to modify gene expression without altering DNA sequences—are being explored in preclinical models. These therapies could complement existing treatments by targeting underlying biological mechanisms rather than surface-level symptoms.
This area of research also reinforces the importance of public health measures aimed at reducing exposure to harmful substances and promoting early-life nutrition. By addressing the roots of metabolic disease, scientists hope to shift the focus from treatment to true prevention, creating space for a future where the risk of type 2 diabetes can be meaningfully reduced or even eliminated.
Frequently Asked Questions: Exploring the Latest Breakthroughs in Diabetes Treatment
What makes a diabetes cure breakthrough different from traditional treatment approaches?
A true diabetes cure breakthrough goes beyond merely managing blood sugar levels; it targets the root causes of the disease. Traditional treatments like metformin or insulin therapy aim to control symptoms, but they do not address the underlying dysfunctions such as insulin resistance or beta cell failure. In contrast, a type 2 diabetes cure breakthrough often involves regenerative strategies like beta cell regeneration, microbiome modulation, or metabolic reprogramming. These methods strive for long-term remission or even reversal, shifting the paradigm from reactive care to proactive healing. As the field evolves, distinguishing between therapeutic management and curative breakthroughs becomes essential for patients seeking meaningful, sustainable outcomes.
How is microbiome research contributing to diabetes breakthroughs?
The gut microbiome has emerged as a novel frontier in understanding and addressing metabolic disorders, particularly type 2 diabetes. Recent research shows that certain bacterial strains can influence insulin sensitivity, inflammatory responses, and even appetite regulation. Manipulating the microbiome through personalized diets, targeted probiotics, or even microbiota transplants is now being explored as a potential type 2 diabetes breakthrough. Unlike medications that act on isolated biochemical pathways, microbiome-based strategies offer a holistic intervention that may affect multiple systems at once. This area of study is also intersecting with t1d latest news, suggesting its relevance in both major forms of diabetes.
Are there any diabetes cure breakthroughs involving wearable technology or smart devices?
Yes, wearable technology is playing an increasingly prominent role in what could be considered a behavioral diabetes breakthrough. Devices like continuous glucose monitors (CGMs) and smart insulin pens do more than track blood sugar—they empower users to understand the nuances of their metabolism in real time. Some systems now integrate artificial intelligence to predict glucose trends and recommend personalized interventions, essentially acting as a virtual endocrinologist. While these innovations may not constitute a cure, they are revolutionizing diabetes management in ways that may ultimately complement other curative efforts. The development of these tools underscores the integration of digital health in the broader quest for a type 2 diabetes cure breakthrough.
What ethical concerns surround genetic interventions in diabetes treatment?
As genetic editing tools like CRISPR become more viable, they open the door to potentially correcting the genetic predispositions linked to type 2 diabetes. However, these advances are not without ethical complexities. Questions about long-term safety, gene patenting, and access to treatment are surfacing alongside the promise of a genetic diabetes cure breakthrough. There’s also the concern of unintended consequences, such as off-target gene effects or unforeseen interactions with other biological systems. Still, as public and scientific dialogue continues, regulatory frameworks and ethical guidelines are being developed to ensure these breakthroughs are used responsibly and equitably.
How are lifestyle-based interventions evolving in the era of scientific diabetes breakthroughs?
Though lifestyle changes have long been a staple in diabetes care, recent research is refining how these interventions are applied. Scientists are now using biometric data and AI-driven analysis to tailor diet and exercise plans to an individual’s genetic and metabolic profile. This precision approach is transforming lifestyle modification into a more data-driven, effective tool in achieving a type 2 diabetes cure breakthrough. Furthermore, behavioral psychology is being integrated into these programs to enhance adherence and long-term success. By blending old wisdom with new science, lifestyle intervention is becoming a more powerful and personalized weapon in the battle against diabetes.
Can diabetes breakthroughs help prevent the disease in high-risk individuals?
Prevention is increasingly seen as the most effective cure, and emerging science is making this idea more tangible. Biomarker profiling and genetic risk scoring can now identify prediabetic individuals long before symptoms appear. Early intervention strategies inspired by diabetes breakthrough research are being tested to reprogram metabolism before full-blown disease develops. For instance, short-term fasting protocols and gut microbiome modulation are being explored as preventive therapies. This shift from reactive treatment to proactive prevention could redefine how both patients and clinicians approach the disease.
How does the t1d latest news influence type 2 diabetes research and treatment?
The crossover between type 1 and type 2 diabetes research is more significant than it might appear at first glance. Innovations in immune modulation, beta cell replacement, and closed-loop insulin delivery systems often originate in the type 1 diabetes space but find applications in type 2 management. For example, encapsulated islet cell transplants, initially developed for type 1, are now being studied in advanced type 2 diabetes cases with beta cell failure. Following the t1d latest news can provide early insights into technologies and therapies that may shape the future of type 2 diabetes care. This cross-pollination enriches the entire diabetes research ecosystem.
What role do socioeconomic factors play in accessing the benefits of a diabetes breakthrough?
Even the most promising diabetes cure breakthrough can fall short if it’s inaccessible to the people who need it most. Socioeconomic disparities often determine who benefits from cutting-edge therapies, particularly those involving gene editing, advanced biologics, or integrated tech platforms. Policy changes, insurance reform, and global health initiatives will be essential to ensure equitable access to these medical advances. This challenge highlights the need for systemic support alongside scientific progress. A true type 2 diabetes breakthrough must also be a breakthrough in affordability and accessibility.
How is the pharmaceutical industry responding to the possibility of a cure?
Historically, the pharmaceutical industry has focused on long-term management drugs rather than curative therapies, which offer limited ongoing revenue. However, shifts in public demand, regulatory frameworks, and technological feasibility are forcing a reevaluation. Companies are now investing in diabetes cure breakthrough research, particularly in areas like beta cell regeneration, insulin breakthrough compounds, and multi-hormone therapies. Strategic partnerships between biotech firms, universities, and pharmaceutical giants are driving a new era of innovation. These changes suggest a growing recognition that the market is ready for transformative solutions, not just incremental improvements.
What is the long-term vision for diabetes care if a cure is found?
If a reliable and safe cure for type 2 diabetes is realized, the healthcare system will undergo significant transformation. Resources currently devoted to chronic management could be redirected toward early detection, precision treatment, and population-wide prevention. Long-term, a diabetes cure breakthrough would not only reduce the personal burden of disease but also yield massive public health and economic benefits. Additionally, lessons learned from curing diabetes could inform treatments for other complex chronic diseases, setting a precedent in medical innovation. The vision extends beyond disease elimination—it offers a template for holistic, proactive healthcare.
Conclusion: Charting the Course Toward a Diabetes Cure Breakthrough
As science continues to unravel the intricate web of factors driving type 2 diabetes, a growing consensus is forming: a cure may not be a singular discovery but a mosaic of therapeutic innovations. From cell-based regeneration and hormone modulation to microbiome manipulation and gene editing, each advancement contributes a vital piece to the puzzle. Together, they are shaping a future where the term “cure” may finally become a reality for millions.
While no single therapy has yet emerged as the definitive type 2 diabetes cure breakthrough, the cumulative momentum is undeniable. The integration of cutting-edge science, patient-centered technology, and precision medicine holds the potential to transform not only how diabetes is treated but how it is understood. Moreover, lessons from type 1 diabetes research—as seen in recent t1d latest news and insulin breakthrough studies—are enriching the strategies applied to type 2 diabetes, further accelerating progress.
Ultimately, the path forward requires collaboration, rigorous clinical testing, and a continued commitment to ethical, evidence-based innovation. For patients and healthcare providers alike, the message is one of cautious optimism: while the horizon is still unfolding, the future of diabetes treatment has never looked more promising. With continued investment in research and a holistic view of metabolic health, the long-sought goal of a cure may be closer than ever imagined.
Further Reading:
Trailblazing Discoveries: The Top 5 Diabetes Research Breakthroughs of 2023
A Brighter Future for Diabetes: New Advances on the Horizon
Type 1 Diabetes Cure: Current Research (2024)
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.