Understanding the Common Misconception About Type 2 Diabetes and Body Weight
For years, the image most often associated with type 2 diabetes has been that of someone who is overweight or obese. This link between excess weight and diabetes is so prevalent in public discourse that many people are shocked to learn that a person can indeed develop type 2 diabetes without being overweight. The reality is more nuanced, and recent scientific findings have begun to peel back the layers on this oversimplified narrative.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
The question, “can you get type 2 diabetes without being overweight?” challenges the conventional belief that body mass index (BMI) alone determines a person’s risk. While obesity is undeniably a major risk factor, thin individuals can also develop insulin resistance and eventually progress to type 2 diabetes. Genetics, fat distribution, muscle mass, ethnicity, and even chronic stress can contribute to this phenomenon. By exploring these lesser-known factors, we gain a deeper, evidence-based understanding of how type 2 diabetes operates across different body types.
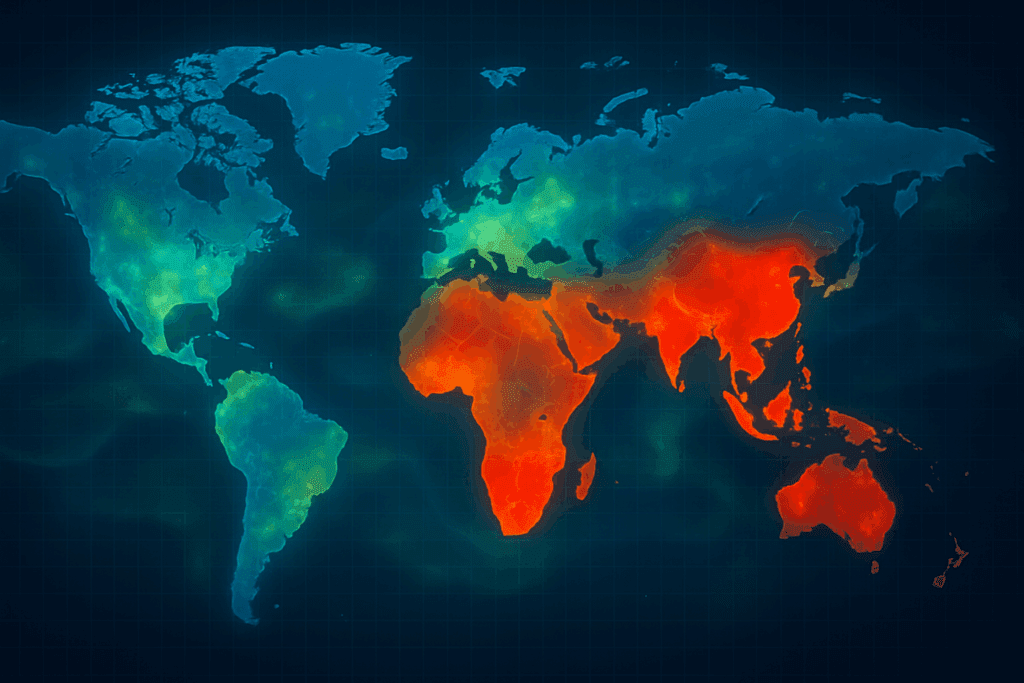
The global rise in diabetes among lean individuals, especially in parts of Asia and Africa, underscores the need to move beyond weight-centric views of this condition. In doing so, we open the door to earlier diagnosis and better outcomes for people who might otherwise be overlooked simply because they don’t fit the stereotypical profile.
What Does It Mean to Have Type 2 Diabetes Without Being Overweight?
Medically speaking, having type 2 diabetes without being overweight means developing impaired glucose regulation despite maintaining a normal or even low BMI. This may seem paradoxical at first, but it becomes clearer when we look at how insulin functions in the body. Insulin is a hormone that helps cells absorb glucose for energy. In type 2 diabetes, the body becomes resistant to insulin or fails to produce enough of it, causing blood sugar levels to rise. This dysfunction doesn’t require excess body weight to develop.
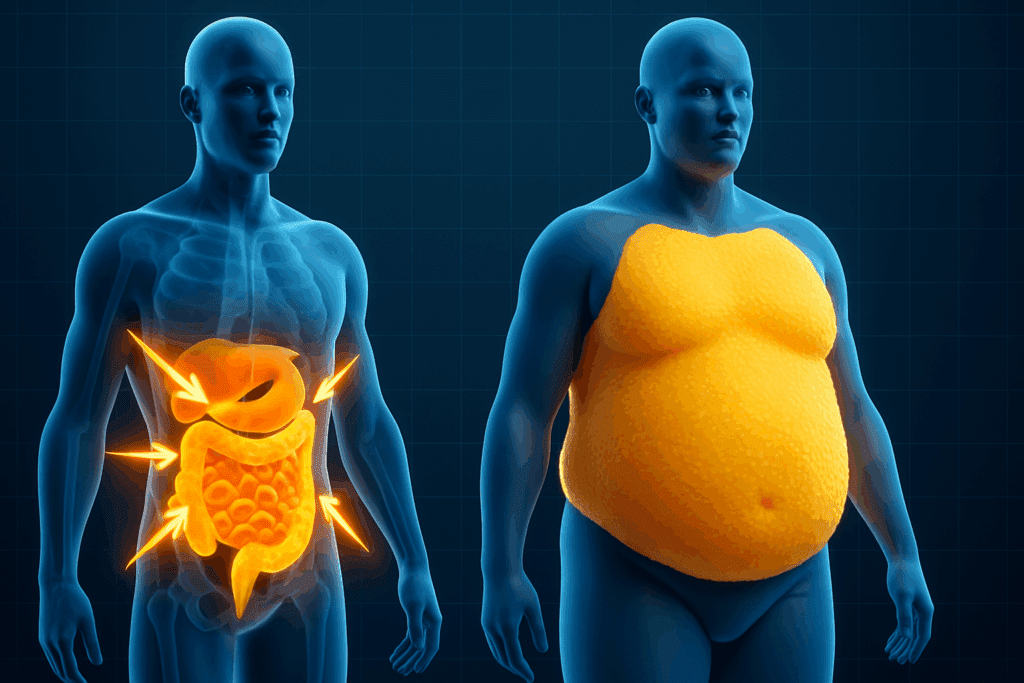
So, can you have type 2 diabetes without being overweight? Absolutely. In fact, lean individuals may sometimes face even more significant challenges because their condition is more likely to be misdiagnosed or diagnosed late. These patients might also harbor dangerous levels of visceral fat—fat stored deep in the abdomen—which is more metabolically active and harmful than subcutaneous fat. This internal fat can promote inflammation and impair insulin signaling, even in those who appear thin on the outside.
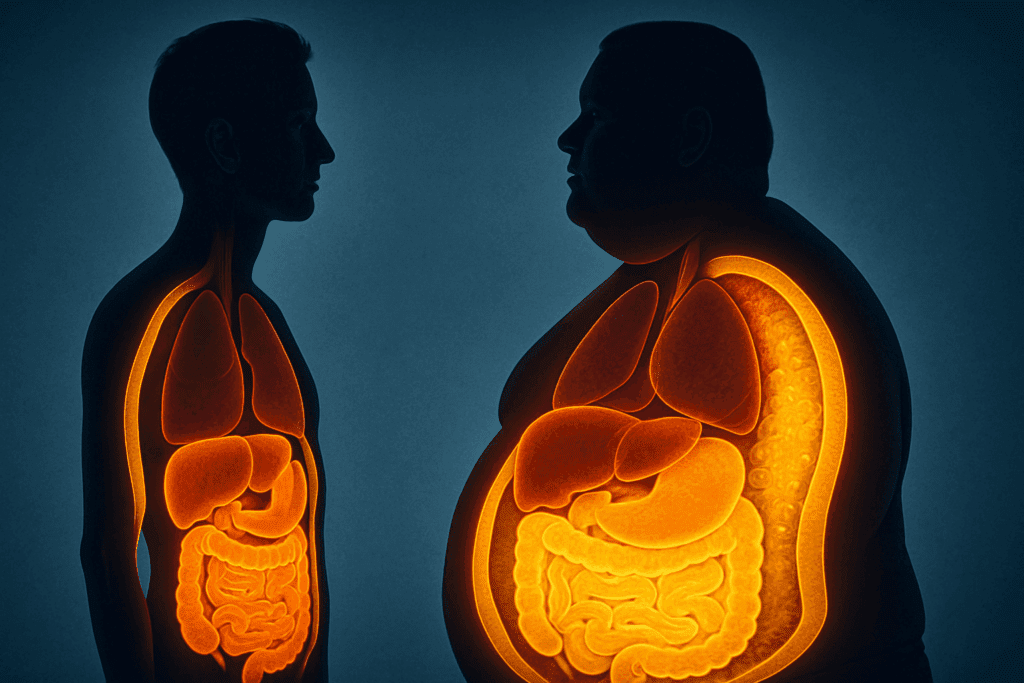
Clinicians are starting to acknowledge that BMI alone is not an adequate marker for metabolic health. Normal-weight individuals can present with what’s known as “TOFI”—thin outside, fat inside. These patients may have normal outward appearances but carry fat deposits around internal organs that increase their risk for metabolic diseases, including type 2 diabetes.
Why Lean Individuals Develop Type 2 Diabetes: The Hidden Risk Factors
There are several reasons why a person might develop type 2 diabetes not overweight. One key factor is genetic predisposition. Certain populations—such as people of South Asian, East Asian, or African descent—have a higher risk of developing diabetes at lower body weights compared to Caucasians. This is partly due to differences in fat distribution, muscle mass, and insulin sensitivity.
Another critical but often overlooked factor is low muscle mass. Muscle plays a vital role in glucose metabolism because it is one of the primary tissues that absorb glucose in response to insulin. Individuals with lower muscle mass have reduced glucose disposal capacity, making it easier for blood sugar levels to rise. Even those who appear thin may be metabolically unhealthy if they are physically inactive or have sarcopenia, a condition characterized by low muscle strength and function.
Chronic stress, sleep deprivation, and exposure to endocrine-disrupting chemicals can also elevate diabetes risk in lean individuals. These environmental and lifestyle factors disrupt the hormonal balance that regulates blood sugar and fat storage, contributing to insulin resistance. Furthermore, certain medications, including corticosteroids and antipsychotics, may impair glucose tolerance, leading to type 2 diabetes even in patients with no history of weight gain.
Thin Type 2 Diabetes Symptoms: What to Watch For If You’re Not Overweight
Recognizing thin type 2 diabetes symptoms can be particularly challenging because the signs may be subtle or misattributed to other causes. Classic symptoms such as frequent urination, excessive thirst, fatigue, and blurred vision can occur regardless of body size. However, in thinner individuals, these symptoms are sometimes overlooked by both patients and healthcare providers.
Unexplained weight loss may be one of the earliest red flags, particularly when accompanied by muscle wasting and a decrease in energy levels. Because these individuals are already lean, the loss of additional weight often goes unnoticed or is mistakenly seen as a sign of good health. In reality, it may indicate poor glucose utilization and muscle breakdown, both hallmarks of uncontrolled diabetes.
Another important symptom in lean diabetics is post-meal blood sugar spikes. These individuals might pass fasting glucose tests but fail oral glucose tolerance tests, which reveal impaired insulin responses after eating. Neuropathy—nerve damage leading to tingling or numbness in the extremities—can also develop in thin patients if diabetes remains undiagnosed and untreated.
Doctors must consider a broader diagnostic lens when evaluating patients with potential diabetes symptoms. Just because someone appears physically healthy doesn’t mean their metabolism is functioning optimally. Testing HbA1c levels, fasting insulin, and postprandial glucose can provide a more comprehensive picture of metabolic health in individuals who do not meet the conventional high-risk profile.
The Role of Visceral Fat and Fat Distribution in Non-Obese Diabetes
One of the most striking insights from recent research is the role that fat distribution plays in determining metabolic risk. Unlike subcutaneous fat—which lies just beneath the skin—visceral fat surrounds vital organs and is strongly associated with inflammation, insulin resistance, and type 2 diabetes. This type of fat is particularly dangerous because it’s not always visible or detectable through BMI alone.
In individuals with type 2 diabetes not overweight, visceral fat may be the silent culprit driving their condition. Thin individuals with central adiposity—commonly referred to as having an “apple-shaped” body—are especially at risk. These patients often have a deceptively low overall body weight but carry disproportionately high levels of intra-abdominal fat. Imaging studies using DEXA or MRI scans reveal this hidden fat in patients who might otherwise be classified as metabolically healthy based on BMI.
Research also shows that visceral fat produces inflammatory molecules called cytokines that interfere with insulin signaling and promote glucose dysregulation. This inflammatory state further exacerbates the risk of developing diabetes, even in the absence of obesity. Targeting visceral fat through lifestyle changes such as resistance training, dietary adjustments, and improved sleep hygiene may offer significant metabolic benefits for non-obese individuals.
Can You Get Type 2 Diabetes Without Being Overweight? Global Data Says Yes
The global burden of diabetes among normal-weight individuals is rising. Data from countries like India, China, and parts of Sub-Saharan Africa show that a significant proportion of type 2 diabetes cases occur in individuals who are not overweight. This challenges the Western-centric model of diabetes risk, which has traditionally focused on obesity as the primary driver.
Epidemiological studies have identified distinct genetic markers in populations with high diabetes prevalence but lower average BMIs. These include variants in genes involved in insulin production, fat metabolism, and inflammation. Additionally, cultural and socioeconomic factors—such as diets high in refined carbohydrates and limited access to healthcare—can contribute to increased diabetes rates among lean individuals.
Understanding regional differences in diabetes risk factors helps public health authorities tailor interventions more effectively. In places where thin individuals are disproportionately affected, screening guidelines may need to shift from BMI-based thresholds to more comprehensive metabolic risk assessments. This can ensure that at-risk individuals are identified and treated early, regardless of body size.

Diagnosis and Treatment Challenges for Lean Type 2 Diabetes Patients
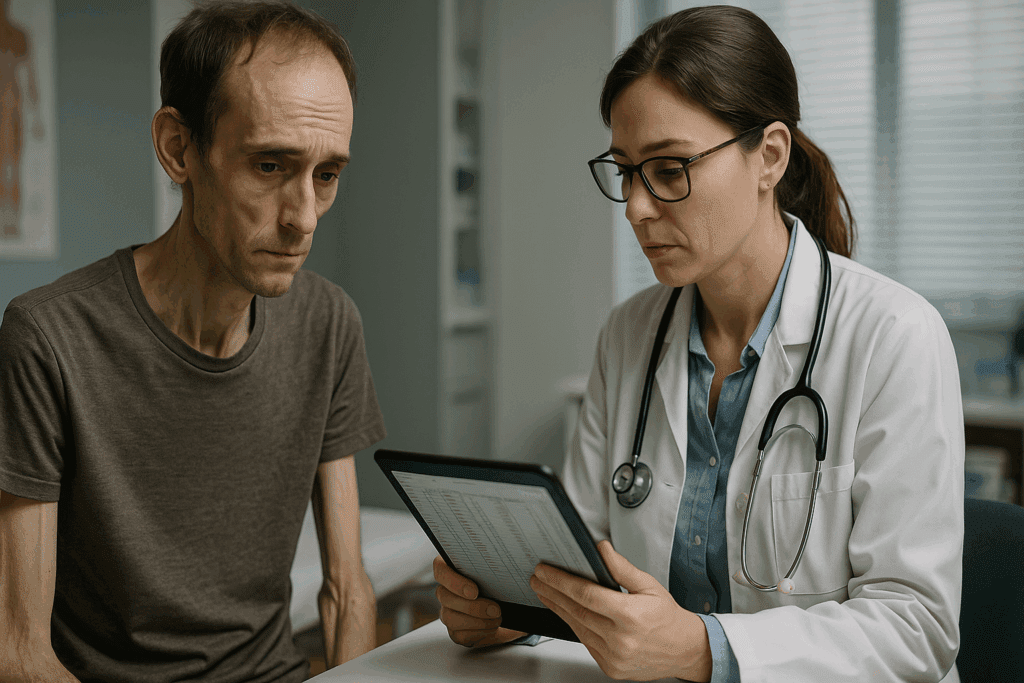
Diagnosing type 2 diabetes in thin individuals presents several challenges. Physicians often rely on BMI as an initial screening tool, which can lead to missed diagnoses in lean patients. Moreover, the assumption that normal-weight individuals are metabolically healthy may delay further testing, resulting in complications by the time the disease is identified.
Once diagnosed, treatment for thin type 2 diabetes patients must be carefully tailored. Standard interventions like weight loss are not applicable, and aggressive calorie restriction may worsen their condition. Instead, emphasis should be placed on building lean muscle mass through strength training and ensuring a nutrient-dense diet that supports metabolic health without promoting further weight loss.
Medication strategies may also need to be adjusted. Metformin, the first-line drug for type 2 diabetes, is effective in many cases but may need to be complemented with agents that improve insulin sensitivity or preserve beta-cell function. Continuous glucose monitoring can provide real-time insights into blood sugar patterns, enabling more personalized treatment plans. Nutritional counseling, physical activity, and stress reduction techniques are all essential components of a holistic management strategy.
Rethinking Risk: Why Thin Doesn’t Always Mean Healthy
The phrase “you can’t judge a book by its cover” is especially true when it comes to metabolic health. Thin individuals may appear healthy on the surface, but their internal metabolic profile can tell a very different story. This disconnect underscores the importance of looking beyond outward appearance when assessing diabetes risk.
Public awareness campaigns often focus on the dangers of obesity, and while this messaging is important, it can inadvertently create blind spots. Lean individuals may not see themselves as candidates for diabetes screening, nor may their doctors think to test them. Expanding public health messaging to include information about non-obese diabetes could lead to earlier diagnosis and better health outcomes for many.
From a scientific perspective, the question of “can you get type 2 diabetes without being overweight?” is no longer up for debate. The answer is a resounding yes, supported by data, clinical experience, and genetic research. As our understanding of type 2 diabetes evolves, so too must our approaches to prevention, diagnosis, and treatment. Everyone—regardless of body size—deserves access to accurate information and proactive healthcare.
Frequently Asked Questions: Thin Type 2 Diabetes Symptoms and Non-Obese Risk Factors
1. How can someone develop type 2 diabetes without being overweight?
Though it surprises many, a person can indeed develop type 2 diabetes without being overweight due to a variety of underlying factors unrelated to body fat. Genetic predisposition plays a critical role, particularly in individuals from South Asian, East Asian, or African backgrounds, who may have higher insulin resistance at lower BMIs. Additionally, chronic inflammation, sleep disturbances, and stress hormones can disrupt glucose metabolism in thin individuals. These non-obese patients may also have disproportionate amounts of visceral fat—fat stored around organs—that significantly increases risk. So, to answer the common question—can you get type 2 diabetes without being overweight? Yes, and in fact, this is a growing public health concern.
2. What are the most overlooked thin type 2 diabetes symptoms?
Subtle but significant, thin type 2 diabetes symptoms often go unnoticed because they don’t match public expectations. These may include unexplained fatigue, increased susceptibility to infections, and irritability after meals—signs of postprandial hyperglycemia. Some lean individuals report difficulty maintaining focus or experience mood swings linked to blood sugar volatility. Because these patients aren’t typically screened for diabetes, such symptoms may be attributed to stress, aging, or nutrient deficiencies. Understanding these less conventional signs is vital to improving outcomes for those with type 2 diabetes not overweight.
3. Are diagnostic guidelines adapting to account for diabetes in non-obese individuals?
Clinical guidelines are slowly evolving, but in many regions, BMI still remains the primary screening criterion—despite evidence showing that you can have type 2 diabetes without being overweight. Some healthcare systems, especially in Asia, are beginning to implement screening for metabolic syndrome and insulin resistance even among those with a normal BMI. Advanced diagnostic tools such as oral glucose tolerance testing (OGTT), C-peptide levels, and insulin sensitivity assessments are proving more effective in these populations. In the future, algorithms incorporating waist circumference, ethnicity, and metabolic biomarkers may become standard. This shift reflects an overdue recognition that thin type 2 diabetes symptoms warrant equal medical attention.
4. Is it harder to manage type 2 diabetes if you are not overweight?
Management can actually be more complex in lean individuals with diabetes, particularly because treatment protocols often assume weight loss as a central goal. For someone with type 2 diabetes not overweight, the focus must shift to maintaining or increasing lean muscle mass, optimizing insulin sensitivity, and preventing muscle catabolism. These patients often require tailored nutritional plans and exercise regimens emphasizing resistance training rather than calorie restriction. Additionally, medications that promote weight loss may be inappropriate or even harmful. In many cases, people ask, “can you get type 2 diabetes without being overweight and still need insulin?”—and the answer is yes, especially if beta-cell dysfunction is prominent.
5. How does having low muscle mass increase diabetes risk in thin individuals?
Muscle tissue is one of the most important sites for glucose uptake in response to insulin. When someone has low skeletal muscle mass—a condition sometimes seen in thin individuals—their body becomes less efficient at clearing glucose from the bloodstream. This inefficiency can contribute to insulin resistance and eventual diabetes onset. The condition is particularly prevalent in sedentary individuals or those with sarcopenia, even if they are not overweight. Therefore, when considering whether someone can have type 2 diabetes without being overweight, it’s important to look beyond fat and focus on the protective role of muscle.
6. What is the psychological impact of being diagnosed with type 2 diabetes as a thin person?
The diagnosis can be particularly jarring for lean individuals, who often perceive themselves as healthy and immune to metabolic diseases. This disconnect may lead to denial, emotional distress, or even stigma—especially if others assume they must be overweight to have diabetes. Patients may feel isolated in support groups or medical environments tailored toward those with obesity-related diabetes. These emotional barriers can complicate self-management and delay treatment adherence. When thin type 2 diabetes symptoms appear, healthcare providers must acknowledge these psychological dimensions to ensure holistic care.
7. Are there different dietary considerations for lean people with type 2 diabetes?
Yes, nutrition strategies must be adapted carefully. While reducing simple carbohydrates and processed sugars remains important, underweight or lean individuals need sufficient calories to avoid further weight loss and muscle wasting. Nutrient-dense foods, balanced macronutrients, and protein timing are crucial in preserving metabolic function. For example, including healthy fats and slow-digesting carbohydrates can help stabilize glucose levels without compromising energy intake. In this context, managing type 2 diabetes not overweight involves a delicate nutritional balance, not the restrictive diets often associated with diabetes management.
8. Are thin individuals with type 2 diabetes more likely to be misdiagnosed with type 1 or LADA?
Absolutely—misdiagnosis is a significant risk. Because thinness is more closely associated with autoimmune diabetes in the medical community, many lean patients are initially diagnosed with type 1 diabetes or latent autoimmune diabetes in adults (LADA). However, unlike autoimmune forms, type 2 diabetes not overweight typically involves insulin resistance rather than immune-mediated beta-cell destruction. Diagnostic clarity requires testing for autoantibodies and C-peptide levels to distinguish between types. Early misclassification can lead to unnecessary insulin use and hinder proper disease management.
9. How does ethnicity influence diabetes risk among non-obese individuals?
Ethnic background has a profound effect on diabetes risk, even at lower BMIs. People of South Asian, East Asian, Hispanic, and African descent have a higher prevalence of visceral fat and reduced insulin sensitivity, making them more susceptible to type 2 diabetes not overweight. In these groups, the pancreas may struggle to compensate for even minor insulin resistance. Standard BMI cutoffs used in Western populations may fail to reflect true metabolic risk in these demographics. A more ethnically inclusive understanding of risk factors can improve early detection and personalized prevention strategies.
10. What does the future hold for detecting and preventing diabetes in lean individuals?
Emerging technologies and precision medicine are beginning to reshape how we view diabetes risk. Artificial intelligence tools are being trained to detect patterns in blood markers and genetics that predict whether someone can get type 2 diabetes without being overweight. Researchers are also exploring the role of the gut microbiome, sleep quality, and circadian rhythms in lean diabetes risk. Wearable devices capable of continuous glucose and stress monitoring may offer earlier insights into metabolic decline. As awareness of thin type 2 diabetes symptoms grows, future screening models are likely to move away from BMI-centric thresholds and toward personalized, risk-based prevention models.
Conclusion: Embracing a Broader Understanding of Type 2 Diabetes Beyond Weight
The evidence is clear: you can have type 2 diabetes without being overweight, and ignoring this fact puts countless individuals at risk of delayed diagnosis and preventable complications. Thin type 2 diabetes symptoms may be subtle, but they are real and often linked to underlying metabolic dysfunction that demands attention. The notion of type 2 diabetes not overweight is not an anomaly—it is a growing reality that challenges long-held assumptions in both medicine and public perception.
By shedding light on the complex interplay of genetics, fat distribution, muscle mass, and lifestyle factors, we move toward a more inclusive, accurate, and effective approach to diabetes care. Clinicians, researchers, and public health leaders must all play a role in expanding awareness and updating screening protocols to reflect the full spectrum of diabetes risk.
Ultimately, the path to better outcomes begins with asking the right questions—such as “can you have type 2 diabetes without being overweight?”—and seeking answers grounded in science, empathy, and a deep commitment to individual well-being.
Further Reading:
Type 2 diabetes – Symptoms and causes
The Role of Obesity in Type 2 Diabetes Mellitus—An Overview
Type 2 Diabetes: What It Is, Causes, Symptoms & Treatment
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.