Understanding Cardiovascular Disease
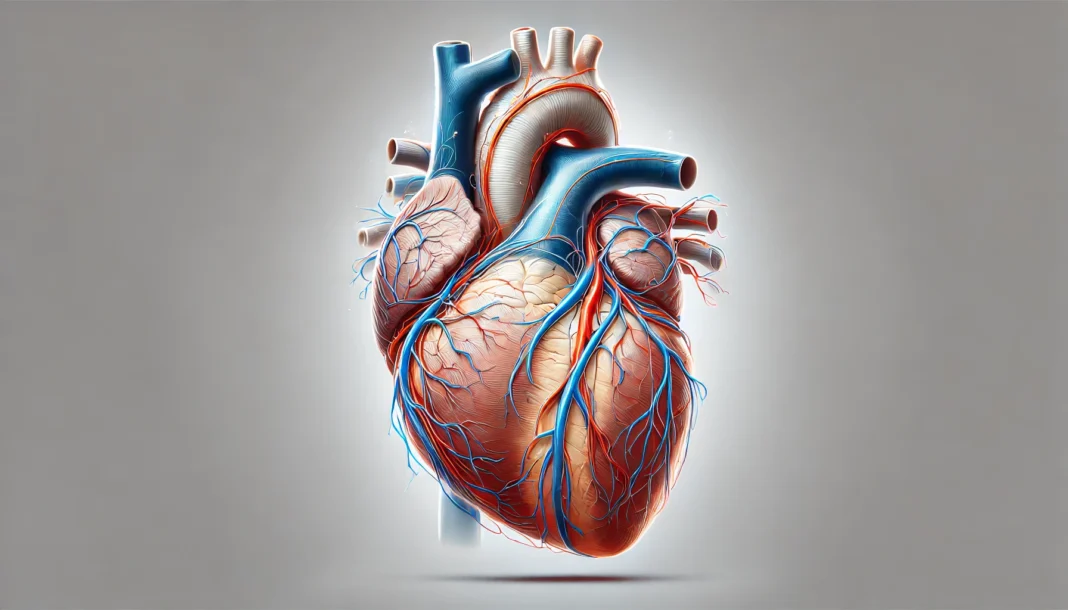
Cardiovascular diseases encompass a broad range of conditions affecting the heart and blood vessels. As the leading cause of mortality worldwide, these diseases significantly impact public health, economic stability, and quality of life. While some conditions arise due to genetic predisposition, others develop because of lifestyle factors such as diet, exercise, smoking, and stress. This comprehensive guide explores the different types of cardiovascular diseases, their causes, symptoms, risk factors, and available treatment options. By understanding the spectrum of heart conditions, individuals can take proactive steps in managing their heart health.
You may also like: 5 Modern Treatments for Heart Disease: Advancements in Cardiac Care
Is Cardiovascular Disease the Same as Heart Disease?
A common misconception is that cardiovascular disease and heart disease are interchangeable terms. While closely related, cardiovascular disease is a broader category that includes all diseases affecting the heart and blood vessels. Heart disease, on the other hand, refers specifically to conditions that impair the heart’s function, such as coronary artery disease, heart failure, and arrhythmias. Recognizing the distinction is essential for understanding the scope of cardiovascular health and the many ways it can be compromised.
Types of Cardiovascular Diseases
The list of cardiovascular diseases includes a variety of conditions that affect the heart and circulatory system. Some of the most prevalent types include coronary artery disease, heart failure, arrhythmias, cardiomyopathies, valvular heart disease, congenital heart defects, and vascular diseases. Each condition has unique characteristics, symptoms, and treatment options.
Coronary Artery Disease (CAD)
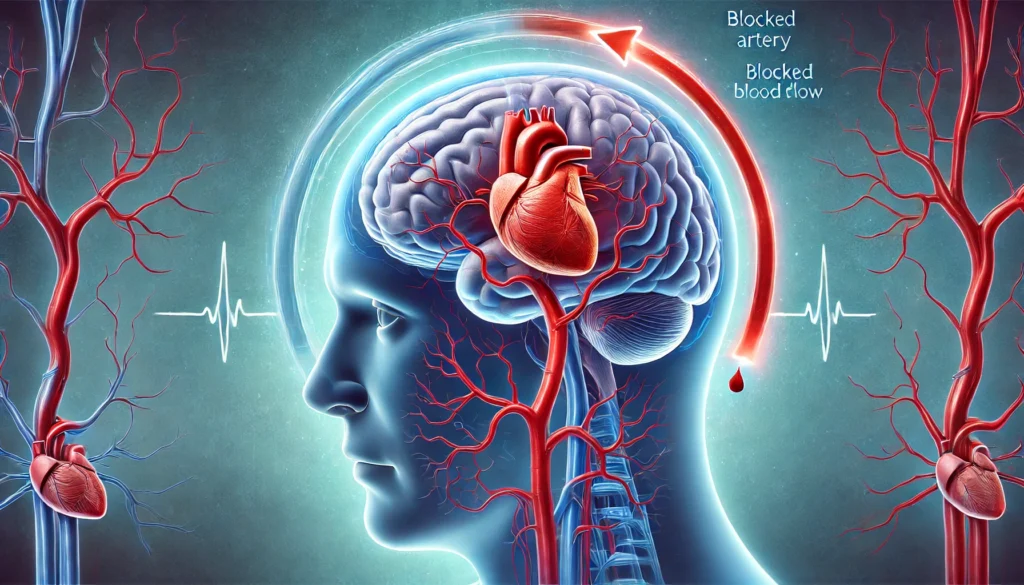
Coronary artery disease is one of the most common cardiovascular disease types and a leading cause of heart attacks. It occurs when the coronary arteries become narrowed or blocked due to plaque buildup, reducing blood flow to the heart muscle. The restricted blood flow can lead to angina, shortness of breath, or myocardial infarction. Lifestyle modifications, medications, and surgical interventions such as angioplasty or bypass surgery are commonly used to manage this condition.
Heart Failure
Heart failure is a serious condition where the heart cannot pump blood efficiently. This can result from various underlying issues, including coronary artery disease, high blood pressure, and cardiomyopathies. Symptoms include fatigue, fluid retention, and shortness of breath. Treatment focuses on improving heart function through medication, lifestyle changes, and, in severe cases, heart transplantation.
Arrhythmias
Arrhythmias refer to irregular heartbeats, which may be too fast, too slow, or erratic. These electrical disturbances can arise from structural heart abnormalities, electrolyte imbalances, or external triggers like stress and medications. While some arrhythmias are harmless, others, such as atrial fibrillation or ventricular tachycardia, can lead to severe complications like stroke or cardiac arrest. Treatment options include medication, catheter ablation, and implantable devices such as pacemakers.
Cardiomyopathies
Cardiomyopathies are diseases of the heart muscle that affect its ability to pump blood effectively. These can be classified into different types, including dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy. Causes range from genetic factors to infections and chronic conditions like diabetes. Early diagnosis is crucial, as treatment can help manage symptoms and prevent complications.
Valvular Heart Disease
Valvular heart disease occurs when one or more of the heart’s valves become damaged or dysfunctional, leading to improper blood flow. Common causes include congenital defects, infections such as rheumatic fever, and degenerative changes with age. Symptoms may include heart murmurs, fatigue, and dizziness. Depending on severity, treatment may involve medication, surgical repair, or valve replacement.
Congenital Heart Defects
Congenital heart defects are structural abnormalities present at birth. They can range from minor issues that resolve independently to severe malformations requiring surgical correction. Advances in medical technology have significantly improved survival rates and quality of life for individuals with congenital heart defects, but ongoing medical management is often necessary.
Vascular Diseases
Vascular diseases affect the blood vessels, leading to conditions such as peripheral artery disease, aneurysms, and deep vein thrombosis. These conditions can result in reduced circulation, increasing the risk of complications like stroke and limb ischemia. Management strategies include lifestyle changes, medications, and surgical interventions to restore proper blood flow.
Risk Factors for Cardiovascular Disease
Several risk factors contribute to the development of heart diseases and disorders. These include high blood pressure, high cholesterol, diabetes, obesity, smoking, sedentary lifestyle, poor diet, and genetic predisposition. Preventive measures such as regular exercise, a heart-healthy diet, smoking cessation, and routine medical check-ups can significantly reduce the risk of cardiovascular complications.
Frequently Asked Questions About Cardiovascular Diseases
1. What Are the Lesser-Known Risk Factors for Cardiovascular Diseases?
While common risk factors like high cholesterol, hypertension, and smoking are well known, several lesser-known contributors also increase the likelihood of developing cardiovascular diseases. Chronic inflammation, which can result from autoimmune disorders, poor dental hygiene, or persistent infections, may contribute to arterial damage and plaque buildup. Environmental factors such as prolonged exposure to air pollution and toxins have been linked to an increased risk of heart conditions. Additionally, sleep disorders like obstructive sleep apnea can strain the heart by causing intermittent oxygen deprivation and spikes in blood pressure. Socioeconomic status also plays a role, as limited access to healthcare and healthy food options can contribute to a higher prevalence of cardiovascular conditions. Addressing these overlooked factors through lifestyle modifications and medical interventions may help reduce the burden of heart disease.
2. How Does Mental Health Influence the Development of Cardiovascular Disease?
There is growing evidence linking mental health conditions to heart disease categories, yet the connection remains underappreciated. Chronic stress, anxiety, and depression can trigger physiological responses such as increased blood pressure, elevated cortisol levels, and inflammation, all of which contribute to heart disease. Individuals experiencing prolonged psychological distress may also be more likely to engage in unhealthy coping mechanisms like smoking, excessive alcohol consumption, or poor dietary choices, further exacerbating cardiovascular risk. Studies suggest that managing stress through mindfulness techniques, cognitive behavioral therapy, or regular physical activity can help mitigate these risks. Healthcare professionals now emphasize an integrative approach to treating heart illnesses that includes mental health care as a crucial component. Recognizing the role of psychological well-being in cardiovascular health can lead to more comprehensive prevention strategies.
3. Can Cardiovascular Diseases Be Reversed Through Lifestyle Changes?
While some damage from cardiovascular disease types may be irreversible, lifestyle modifications can significantly slow progression and even partially reverse certain conditions. A plant-based diet rich in antioxidants and anti-inflammatory properties has been shown to improve endothelial function and reduce arterial plaque buildup. Regular physical activity enhances circulation, reduces blood pressure, and strengthens the heart muscle, mitigating the effects of existing conditions. Smoking cessation and reducing alcohol intake play crucial roles in improving heart function and preventing further deterioration. Emerging research on intermittent fasting and calorie restriction suggests potential benefits in reducing cardiovascular risk by improving metabolic health. While medical interventions may still be necessary, proactive lifestyle changes remain one of the most effective tools in managing and improving cardiovascular health.
4. What Are Some Rare or Overlooked Cardiovascular Diseases?
Beyond well-known heart disease names like coronary artery disease and heart failure, several rare and often overlooked conditions can affect cardiovascular health. Takotsubo cardiomyopathy, commonly known as “broken heart syndrome,” is a stress-induced condition that mimics a heart attack but is typically reversible. Pericarditis, an inflammation of the heart’s outer lining, can cause chest pain and fluid accumulation, leading to complications if untreated. Buerger’s disease, which primarily affects smokers, causes blood vessel inflammation and can lead to tissue damage and amputations. Marfan syndrome, a genetic disorder, can result in aortic enlargement and a higher risk of life-threatening ruptures. While these conditions may not be as prevalent as other heart diseases and disorders, recognizing their symptoms and risk factors is vital for early intervention and treatment.
5. How Does Cardiovascular Disease Differ Between Men and Women?
Men and women experience different types of CVD with variations in symptoms, risk factors, and responses to treatment. Women are more likely to experience atypical symptoms such as fatigue, nausea, and shortness of breath rather than the classic chest pain associated with heart attacks. Hormonal fluctuations, particularly post-menopause, can increase the risk of cardiovascular disease due to decreased estrogen levels, which previously offered some protective effects. Women are also more susceptible to conditions such as microvascular disease, which affects the smaller arteries of the heart rather than the major coronary arteries. Despite these differences, women are often underdiagnosed and undertreated, leading to worse health outcomes. Greater awareness of gender-specific cardiovascular risks can lead to improved diagnostic approaches and tailored treatment strategies.
6. Are There Specific Dietary Habits That Increase the Risk of Cardiovascular Diseases?
A poor diet plays a critical role in the development of various cardiovascular disease types by contributing to obesity, inflammation, and arterial plaque buildup. Diets high in processed foods, trans fats, and excessive sugar can lead to insulin resistance, which is closely linked to heart disease. Excessive sodium intake can increase blood pressure, placing additional strain on the cardiovascular system and increasing the likelihood of stroke or heart failure. Conversely, diets rich in omega-3 fatty acids, fiber, and plant-based foods have been shown to reduce inflammation and support overall heart health. While moderation is key, consistently making heart-friendly food choices can significantly impact long-term cardiovascular outcomes.
7. How Does Exercise Benefit Cardiovascular Health Beyond Weight Management?
While exercise is commonly associated with weight loss, its benefits for cardiovascular health extend far beyond weight management. Regular physical activity strengthens the heart muscle, enhances circulation, and improves oxygen utilization, reducing the burden on the heart. Exercise also promotes the production of nitric oxide, a molecule that helps keep blood vessels flexible and reduces the risk of hypertension. Additionally, it plays a crucial role in balancing cholesterol levels by increasing high-density lipoprotein (HDL) and reducing low-density lipoprotein (LDL). Resistance training and aerobic exercises have distinct cardiovascular benefits, making a combination of both ideal for overall heart health. Incorporating movement into daily life, even in small ways, can yield significant improvements in cardiovascular function.
8. What Role Does Genetics Play in Cardiovascular Disease Development?
Genetics play a substantial role in determining an individual’s risk of developing heart illnesses, but lifestyle choices still have significant influence. Some genetic mutations predispose individuals to conditions such as familial hypercholesterolemia, which leads to dangerously high cholesterol levels from an early age. Certain forms of cardiomyopathy, arrhythmias, and aortic disorders also have strong hereditary components. However, genetic predisposition does not guarantee disease development; environmental factors and lifestyle choices play a crucial role in disease manifestation. Genetic testing and family history assessments can help individuals take preemptive measures to manage their risk and make informed healthcare decisions.
9. How Do Emerging Technologies Impact Cardiovascular Disease Treatment?
Advancements in medical technology are revolutionizing the diagnosis and treatment of different types of heart conditions. Wearable devices equipped with electrocardiogram (ECG) capabilities allow for real-time heart monitoring, enabling early detection of arrhythmias and other abnormalities. Artificial intelligence (AI) is improving diagnostic accuracy by analyzing medical imaging and identifying potential cardiovascular issues before they become severe. Minimally invasive procedures, such as transcatheter aortic valve replacement (TAVR), are providing safer alternatives to traditional open-heart surgeries. Stem cell research and gene therapy hold promise for regenerating damaged heart tissue and addressing genetic heart diseases at the molecular level. These innovations are shaping the future of cardiovascular care, improving survival rates and patient outcomes.
10. How Can Cardiovascular Disease Prevention Strategies Be Personalized?
While general heart health recommendations apply to most individuals, personalized prevention strategies are gaining traction as a more effective approach. Advances in precision medicine allow for genetic profiling to determine an individual’s specific risks and tailor interventions accordingly. Personalized dietary plans consider metabolic differences, food sensitivities, and genetic predispositions to optimize heart health. Wearable technology and remote monitoring provide real-time insights into cardiovascular function, allowing for more responsive and individualized healthcare. Stress management techniques can also be customized based on personality traits and psychological predispositions to enhance long-term adherence. By embracing a more personalized approach, individuals can take more targeted actions to protect their heart health and mitigate their specific risk factors.
Conclusion: Protecting Heart Health
Understanding the different types of heart diseases and disorders is crucial for prevention, early detection, and effective management. By recognizing risk factors and adopting heart-healthy habits, individuals can reduce their susceptibility to these conditions. Advances in medical research continue to improve treatment options, offering hope for better outcomes and longevity. Maintaining cardiovascular health requires a commitment to informed lifestyle choices and proactive medical care, ensuring a healthier future for individuals and communities alike.
cardiovascular health risks, heart attack prevention, blood circulation disorders, chronic heart conditions, heart muscle diseases, arterial blockage symptoms, managing high blood pressure, stroke prevention strategies, cardiac rehabilitation programs, lifestyle changes for heart health, early signs of heart disease, reducing cholesterol naturally, genetic heart conditions, advanced heart failure treatment, heart disease prevention tips, improving heart function, hypertension management techniques, impact of diet on heart health, exercise benefits for the heart, understanding heart inflammation
Further Reading:
What is Cardiovascular Disease?
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.