Atherosclerosis of the aorta is a significant cardiovascular condition characterized by the abnormal hardening of the walls of an artery or arteries due to the buildup of plaques consisting of cholesterol, fatty substances, calcium, and other cellular debris. This disease can lead to severe complications, including heart attacks, strokes, and aneurysms, making early detection and management essential. Understanding the underlying mechanisms, risk factors, symptoms, and available treatment options can help individuals make informed decisions about their cardiovascular health and take preventive measures to reduce their risk.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery
The Pathophysiology of Atherosclerosis of the Aorta
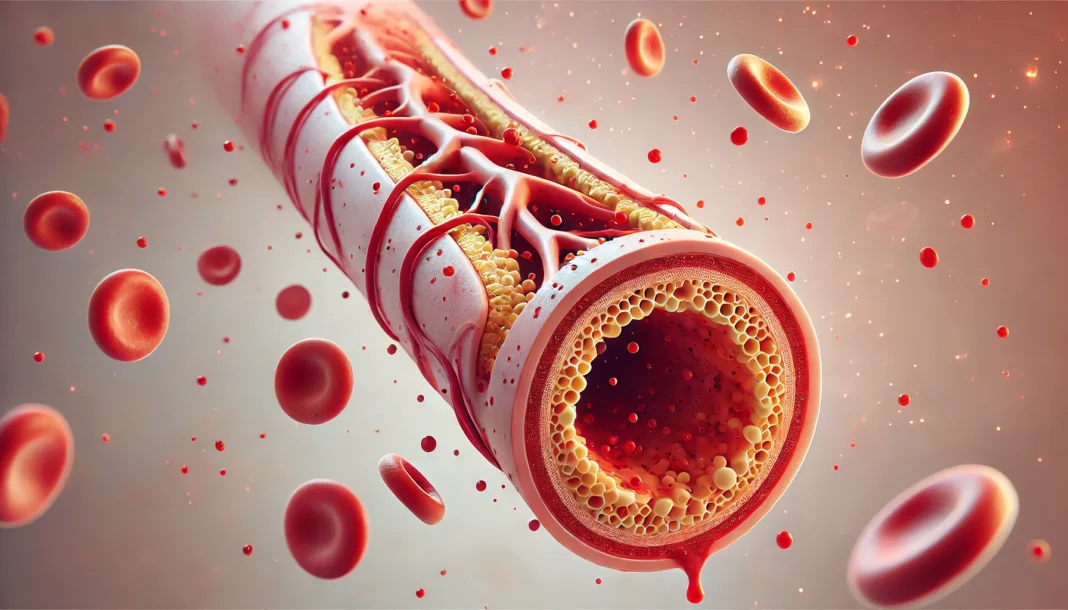
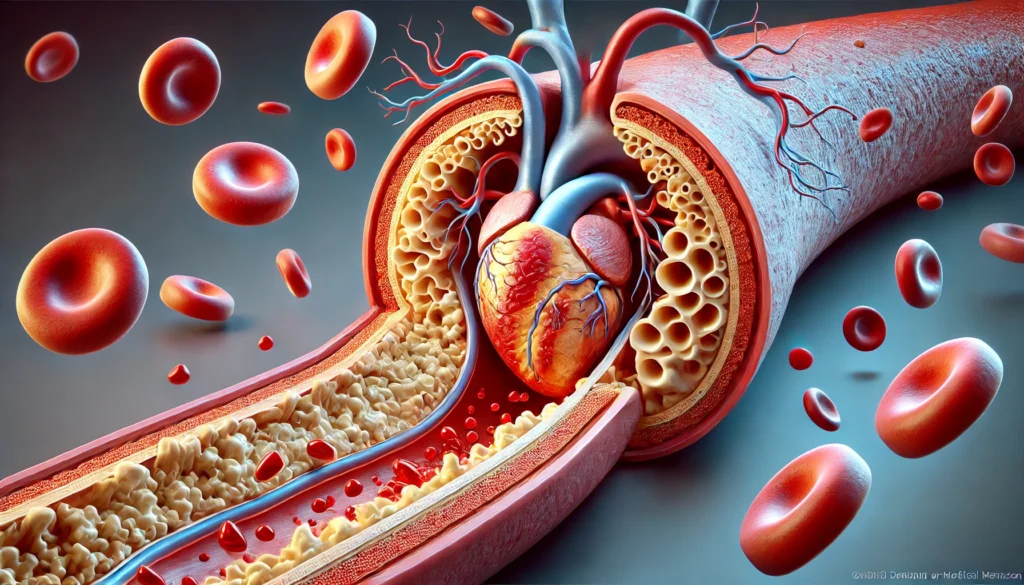
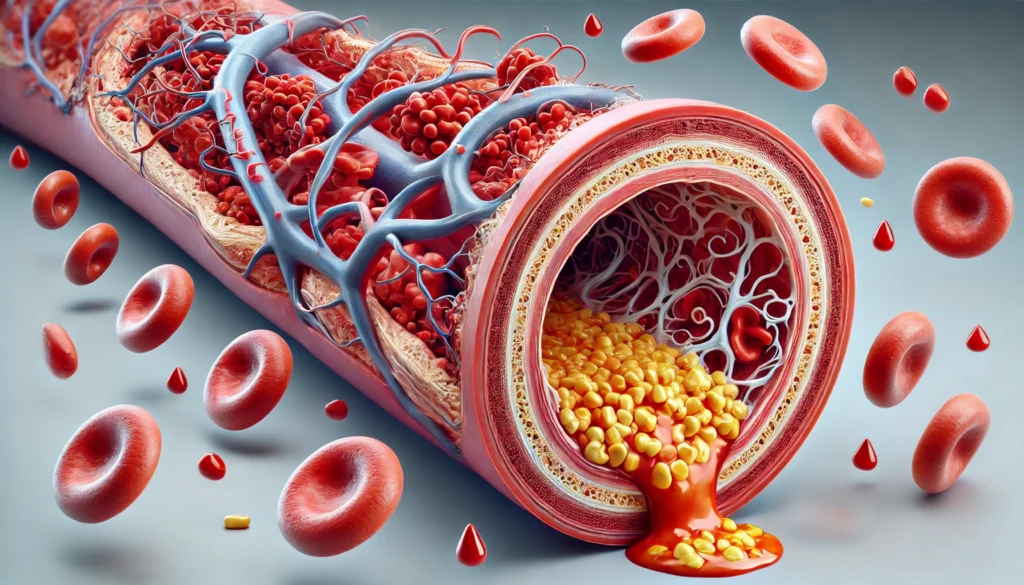
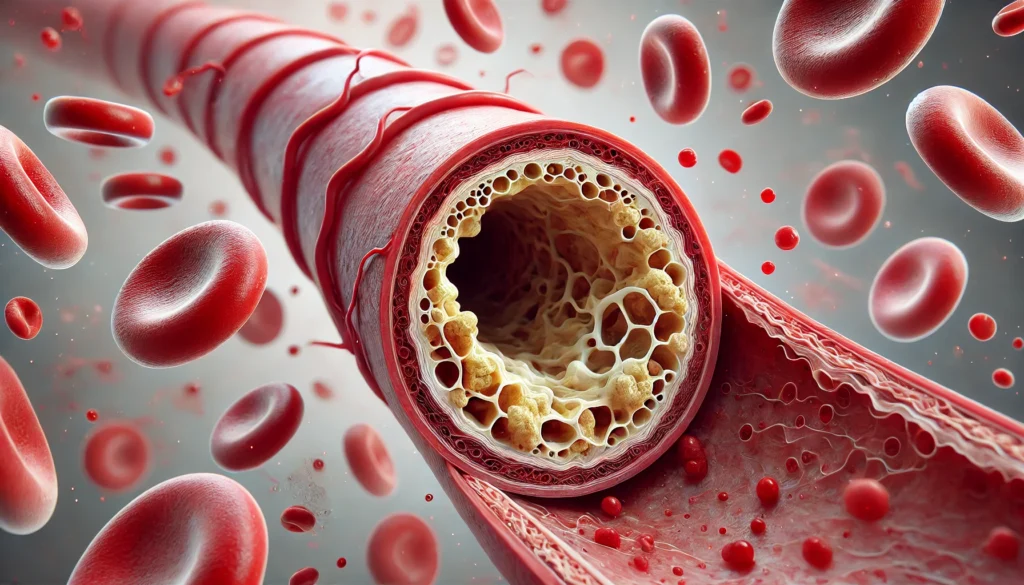
Atherosclerosis of the aorta is a progressive disease that begins with damage to the endothelium, the delicate inner lining of blood vessels. This damage can be caused by various factors, including hypertension, high cholesterol levels, smoking, diabetes, and inflammation. Once the endothelium is compromised, low-density lipoprotein (LDL) cholesterol infiltrates the arterial wall, triggering an immune response that results in chronic inflammation. Over time, white blood cells such as macrophages attempt to clear the cholesterol but instead become foam cells, leading to the formation of fatty streaks within the artery.
As the disease advances, these fatty streaks evolve into larger plaques that can restrict blood flow. The presence of calcium deposits further contributes to the hardening of the aorta, reducing its elasticity and increasing the risk of rupture. Severe atherosclerosis of the abdominal aorta and iliac arteries can lead to significant blockages, impairing circulation to lower extremities and potentially causing critical limb ischemia. This condition underscores the importance of early intervention and lifestyle modifications to slow disease progression.
Risk Factors Contributing to Aortic Atherosclerosis
Several risk factors predispose individuals to the development of atherosclerotic disease of the aorta. Some of these are modifiable, meaning they can be addressed through lifestyle changes, while others are non-modifiable and require medical surveillance. Among the modifiable risk factors, high blood pressure plays a critical role, as persistent hypertension exerts excessive force on arterial walls, accelerating endothelial damage and plaque formation. Similarly, elevated cholesterol levels, particularly LDL cholesterol, contribute to plaque buildup, making dietary modifications and lipid-lowering therapies essential components of prevention.
Smoking is another significant risk factor, as it not only damages the endothelium but also promotes oxidative stress and inflammation. Diabetic individuals are also at increased risk due to the harmful effects of chronic hyperglycemia on blood vessels. In contrast, non-modifiable risk factors include age, with older individuals being more susceptible to atherosclerosis, and genetic predisposition, which can increase vulnerability to cardiovascular disease. Understanding these risk factors allows for the implementation of targeted prevention strategies tailored to an individual’s health profile.
Recognizing the Symptoms of Atherosclerosis
The manifestations of atherosclerosis vary depending on the severity and location of arterial blockages. In the early stages, mild atherosclerosis may not produce noticeable symptoms, making routine health screenings essential for early detection. As the disease progresses, symptoms of arteriosclerosis may include chest pain (angina), shortness of breath, and fatigue, particularly during physical exertion. These symptoms often indicate that atherosclerosis has already begun to impair blood flow to the heart.
Atherosclerosis of the abdominal aorta can present with abdominal pain, particularly after meals, as reduced blood supply affects digestive organs. In more advanced cases, severe atherosclerosis of the abdominal aorta and iliac arteries can lead to leg pain, cramping, or numbness due to restricted circulation to the lower extremities. In cases where plaque rupture occurs, leading to the formation of blood clots, individuals may experience sudden, life-threatening events such as heart attacks or strokes. Therefore, being vigilant about early warning signs and seeking medical attention promptly is crucial.
Diagnosing Atherosclerosis of the Aorta
Accurate diagnosis of atherosclerosis requires a combination of clinical assessment and imaging studies. Physicians typically begin with a thorough medical history and physical examination to evaluate risk factors and symptoms. Blood tests measuring cholesterol levels, inflammatory markers, and blood glucose provide further insights into an individual’s cardiovascular risk profile. Non-invasive imaging techniques such as ultrasound, computed tomography (CT) angiography, and magnetic resonance angiography (MRA) are commonly used to visualize the extent of plaque buildup and assess blood flow.
For cases where more detailed examination is required, an angiogram may be performed, in which a contrast dye is injected into the arteries to provide a clearer view of blockages. Identifying the severity of atherosclerosis through these diagnostic tools enables healthcare providers to recommend appropriate treatment strategies tailored to the patient’s specific condition and risk factors.
Treatment Options for Aortic Atherosclerosis
The treatment of atherosclerosis involves a multifaceted approach that includes lifestyle modifications, medications, and, in severe cases, surgical interventions. Lifestyle changes play a foundational role in managing atherosclerosis disease treatment. Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce cholesterol levels and inflammation. Regular physical activity is equally essential, as it improves circulation, enhances cardiovascular function, and aids in weight management.
Medications are frequently prescribed to manage risk factors and prevent disease progression. Atherosclerosis medication may include statins to lower cholesterol, antihypertensive drugs to control blood pressure, and antiplatelet agents such as aspirin to reduce the risk of clot formation. In cases of advanced atherosclerosis where blood flow is significantly compromised, surgical procedures such as angioplasty, stent placement, or bypass surgery may be necessary to restore circulation and prevent complications.
Preventing Atherosclerosis: Strategies for Long-Term Cardiovascular Health
Prevention remains the most effective strategy for reducing the burden of atherosclerotic disease of the aorta. Adopting a proactive approach that focuses on minimizing risk factors can significantly lower the likelihood of developing severe complications. Dietary choices play a crucial role, with emphasis placed on consuming nutrient-dense foods that support vascular health. Omega-3 fatty acids found in fish, nuts, and seeds have been shown to reduce inflammation and improve lipid profiles, making them valuable additions to a heart-protective diet.
Regular physical activity, such as brisk walking, swimming, or cycling, promotes cardiovascular fitness and enhances endothelial function. Smoking cessation is one of the most impactful changes an individual can make, as it not only reduces the risk of atherosclerosis but also improves overall respiratory and vascular health. Managing underlying conditions such as diabetes and hypertension through medical supervision and lifestyle adjustments is also essential in mitigating cardiovascular risks.
Frequently Asked Questions (FAQ) About Atherosclerosis of the Aorta
What are the early signs of atherosclerosis of the aorta?
In its early stages, atherosclerosis of the aorta may not present noticeable symptoms, making it a silent but progressive disease. However, as plaques develop and begin to obstruct blood flow, subtle warning signs can emerge. These may include fatigue, mild chest discomfort, and decreased tolerance for physical activity, particularly in older adults. Some individuals may experience transient dizziness or episodes of lightheadedness, often mistaken for unrelated conditions. The early stages of hardening of the arteries require close monitoring, as preventive measures at this stage can significantly reduce the risk of severe cardiovascular complications.
How does abdominal aortic atherosclerosis affect overall health?
Abdominal aortic atherosclerosis can have widespread effects beyond the aorta itself, impairing circulation to vital organs such as the kidneys, intestines, and lower extremities. Poor blood flow to the digestive system can lead to abdominal pain after meals, known as intestinal angina, while reduced perfusion to the kidneys may contribute to hypertension and kidney dysfunction. In severe cases, atherosclerosis of the abdominal aorta and iliac arteries can lead to peripheral artery disease, increasing the risk of limb ischemia and ulcers. Over time, progressive plaque accumulation may result in aneurysm formation, posing a life-threatening rupture risk. Understanding these systemic effects highlights the need for early intervention to prevent irreversible damage.
What are super narrow arteries called, and how do they impact circulation?
Super narrow arteries, commonly referred to as stenotic arteries, are significantly restricted due to the buildup of atherosclerotic plaques. These narrowed vessels reduce the amount of oxygenated blood that reaches vital tissues, leading to ischemia and potential organ dysfunction. Aortic atherosclerosis can cause severe narrowing within the body’s largest artery, affecting blood supply to multiple regions, while stenosis in smaller arteries can increase the risk of localized complications. When stenosis occurs in the coronary arteries, it can lead to angina or myocardial infarction. In contrast, narrowing in cerebral arteries may contribute to stroke or transient ischemic attacks, underscoring the dangers of progressive vascular obstruction.
How can atherosclerosis lead to symptoms of arteriosclerosis in the brain?
Atherosclerosis contributes to the hardening of the arteries in the brain by causing reduced elasticity and narrowing of cerebral vessels, impairing blood flow to critical areas. This condition is associated with vascular dementia, a form of cognitive decline caused by chronic ischemia and microvascular damage. Common symptoms include memory loss, confusion, difficulty concentrating, and, in some cases, sudden neurological deficits resembling strokes. When left untreated, advanced atherosclerosis can significantly increase the likelihood of major cerebrovascular events. Recognizing the connection between aortic atherosclerosis and brain health emphasizes the importance of maintaining optimal cardiovascular function to preserve cognitive abilities.
What treatment options are available for an atherosclerotic aorta?
Atherosclerosis disease treatment involves a combination of lifestyle modifications, medication, and, in some cases, surgical intervention. Lifestyle changes such as a heart-healthy diet, regular exercise, and smoking cessation are essential in slowing disease progression. Atherosclerosis medication may include statins to lower cholesterol, antihypertensive drugs to control blood pressure, and antiplatelet agents to reduce clot formation risk. In severe cases, procedures like angioplasty with stent placement or bypass surgery may be required to restore adequate blood flow. A personalized treatment approach is critical in addressing the unique factors contributing to each patient’s condition.
Can mild atherosclerosis progress to a more severe form?
Yes, mild atherosclerosis can gradually progress into advanced atherosclerosis if left unmanaged. While early atherosclerosis may only involve small fatty deposits, these plaques can grow over time, hardening the aorta artery and leading to significant blood flow restriction. Factors such as uncontrolled hypertension, poor diet, and smoking accelerate this progression, increasing the risk of cardiovascular complications. Regular monitoring through medical imaging and blood tests helps track disease progression and allows for timely interventions. Preventative strategies, including dietary adjustments and exercise, play a pivotal role in halting the advancement of plaque buildup.
How can you prevent atherosclerosis from developing?
Preventing atherosclerosis requires a multifaceted approach that includes dietary improvements, regular physical activity, and risk factor management. A diet rich in fiber, healthy fats, and antioxidants helps reduce inflammation and cholesterol levels, slowing the hardening of arteries symptoms before they become severe. Engaging in at least 150 minutes of moderate-intensity exercise per week strengthens the cardiovascular system and improves circulation. Regular health screenings for blood pressure, cholesterol levels, and blood sugar help detect early warning signs and allow for proactive treatment. Avoiding smoking and excessive alcohol consumption also significantly lowers the likelihood of developing atherosclerotic disease of the aorta.
What are the complications of severe atherosclerosis of the abdominal aorta and iliac arteries?
Severe atherosclerosis of the abdominal aorta and iliac arteries can lead to life-threatening complications such as aneurysm formation, arterial blockages, and critical limb ischemia. Aneurysms pose a significant rupture risk, resulting in internal bleeding that requires emergency medical intervention. Blockages in the iliac arteries can restrict blood flow to the lower extremities, causing pain, numbness, and impaired wound healing, increasing the risk of gangrene and amputation. In cases where circulation is severely compromised, endovascular or surgical procedures may be required to restore blood flow. Understanding these potential complications underscores the importance of early detection and aggressive risk factor management.
What role do genetics play in the development of atherosclerosis?
While lifestyle choices are major contributors to atherosclerosis, genetics also play a significant role in determining an individual’s susceptibility to the disease. A family history of cardiovascular conditions increases the likelihood of developing an atherosclerotic abdominal aorta or other vascular abnormalities. Genetic predisposition can influence cholesterol metabolism, inflammation levels, and blood vessel integrity, all of which contribute to plaque formation. Individuals with a strong family history should undergo regular cardiovascular screenings and adopt preventive measures early in life. Advances in genetic research are providing deeper insights into hereditary risk factors, potentially paving the way for more personalized atherosclerosis treatments.
How does stress contribute to the progression of atherosclerosis?
Chronic stress has been linked to an increased risk of developing atherosclerosis by promoting inflammation, hypertension, and unhealthy coping mechanisms such as poor dietary choices and smoking. Elevated stress hormones like cortisol can contribute to endothelial dysfunction, making arteries more susceptible to plaque formation. The inflammatory response triggered by prolonged stress may accelerate the manifestations of atherosclerosis, increasing the likelihood of cardiovascular events. Practicing stress management techniques, including mindfulness, meditation, and regular physical activity, can help mitigate these effects. Recognizing the impact of psychological health on cardiovascular disease highlights the importance of a holistic approach to atherosclerosis of aorta treatment and prevention.
Conclusion: Taking Charge of Aortic Health
Atherosclerosis of the aorta is a complex yet largely preventable condition that demands attention to cardiovascular health and proactive disease management. By understanding the underlying causes, recognizing early symptoms, and implementing effective treatment strategies, individuals can significantly reduce their risk of complications associated with this condition. Lifestyle modifications, combined with appropriate medical interventions, form the cornerstone of effective prevention and treatment. Through ongoing research, advancements in diagnostic techniques, and the development of innovative therapies, the future holds promise for improved cardiovascular outcomes. Taking charge of one’s heart health today ensures a healthier, more resilient cardiovascular system in the years to come.
arterial plaque buildup, cardiovascular disease prevention, endothelial dysfunction, vascular inflammation, cholesterol and heart health, coronary artery disease risk, blood vessel elasticity, lifestyle changes for heart health, circulatory system disorders, heart attack prevention, stroke risk factors, vascular calcification, high blood pressure effects, peripheral artery disease symptoms, aneurysm formation risks, chronic hypertension impact, arterial blockage symptoms, healthy blood flow maintenance, metabolic syndrome and heart disease, medical imaging for atherosclerosis
Further Reading:
What to know about atherosclerosis
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.