Blood vessel disease, a broad term encompassing various disorders affecting the arteries, veins, and capillaries, can have profound implications on overall health. From mild circulation issues to life-threatening conditions such as strokes and heart attacks, vascular diseases demand attention and awareness. Recognizing vascular disease symptoms early and understanding their causes can play a crucial role in timely intervention and management. This article delves into the intricate world of blood vessel disease, exploring its symptoms, associated risks, and critical moments when medical intervention is necessary.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery

The Nature of Blood Vessel Disease
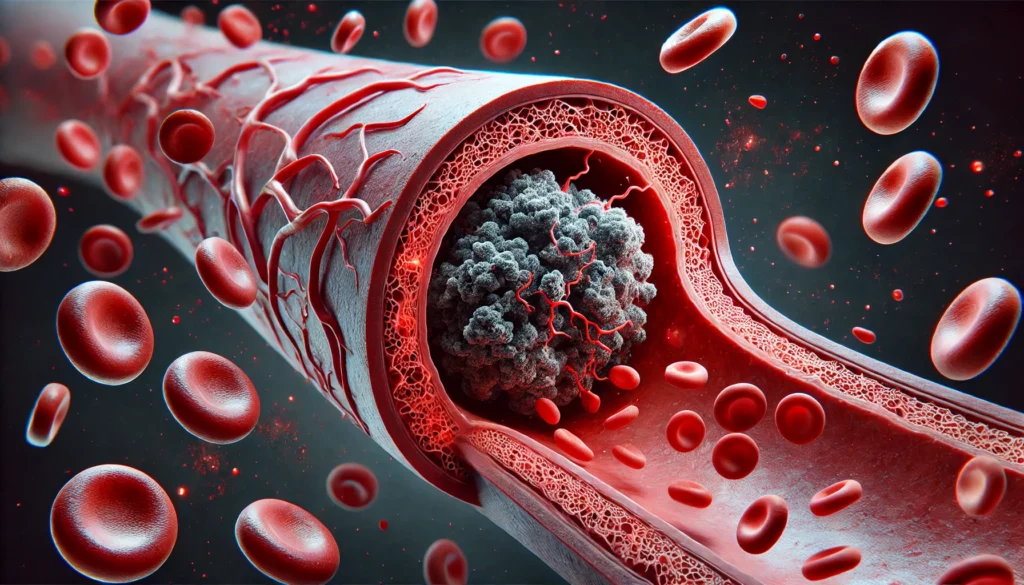
Blood vessels form an essential network within the human body, facilitating the transportation of oxygen, nutrients, and hormones to tissues and organs. Any dysfunction within this system can significantly impact circulation, leading to conditions such as atherosclerosis, aneurysms, and venous insufficiency. The disorder of arteries and arterioles, unspecified or non-specified, often refers to abnormalities within the vascular system that do not fit a precise diagnostic category. These conditions can result in narrowed or weakened arteries, reducing blood flow and increasing the risk of serious complications. Understanding what disorder of arteries and arterioles unspecified means is critical to managing vascular health.
Blood vessel diseases can develop due to genetic predisposition, lifestyle factors, or underlying health conditions. Conditions such as diabetes, high cholesterol, and hypertension frequently contribute to the deterioration of vascular health. In many cases, symptoms remain subtle until significant damage has occurred, underscoring the importance of early detection and preventive measures.
Common Symptoms of Vascular Disease
Vascular disease symptoms vary depending on the affected blood vessels and the severity of the condition. Peripheral artery disease (PAD), for instance, commonly presents as leg pain, cramping, or numbness, particularly during physical activity. This occurs due to restricted blood flow to the lower extremities. Similarly, carotid artery disease can cause dizziness, sudden weakness, or even stroke-like symptoms as a result of reduced blood supply to the brain.
A less commonly discussed symptom is the visibility of arteries in the arms. Many people wonder what disease makes arteries in the arms visible through skin. This phenomenon can be linked to conditions such as chronic venous insufficiency, where weakened vein walls result in engorged and prominent vessels. Additionally, low body fat, excessive physical exertion, or connective tissue disorders can contribute to the visibility of veins and arteries beneath the skin.
Other vascular disease symptoms include cold extremities, slow-healing wounds, discoloration of the skin, and persistent swelling. In severe cases, blood vessel disease may lead to life-threatening complications such as aneurysms, which can rupture and cause internal bleeding, or deep vein thrombosis (DVT), which poses the risk of pulmonary embolism.

Risks Associated with Blood Vessel Disease
The risks linked to blood vessel disease extend beyond circulation problems. One of the most concerning complications is an increased likelihood of heart attack and stroke. When arteries become narrowed or blocked due to plaque buildup, the risk of ischemic events rises dramatically. This is particularly relevant to those experiencing arm veins heart attack symptoms, as prominent veins combined with pain, swelling, or numbness in the arms can indicate cardiovascular distress.
Uncontrolled vascular disease can also contribute to organ damage. The kidneys, for example, rely on healthy blood flow to filter waste and regulate blood pressure. If vascular disease compromises kidney function, patients may develop chronic kidney disease or even require dialysis. Similarly, compromised circulation to the extremities can result in ulcers, infections, and, in extreme cases, tissue necrosis, leading to amputation.
When to Seek Medical Help
Seeking medical attention for blood vessel disease is crucial when symptoms become persistent or severe. Individuals experiencing sudden weakness, loss of coordination, or difficulty speaking should seek immediate emergency care, as these may be warning signs of a stroke. Likewise, symptoms such as intense chest pain, shortness of breath, or severe limb pain warrant urgent medical evaluation to rule out heart attack or vascular blockage.
Those diagnosed with conditions like hypertension or diabetes should undergo regular vascular screenings to monitor potential complications. Identifying early warning signs, such as minor changes in skin color, unusual swelling, or persistent cramping, can lead to timely treatment and improved outcomes. If a patient is unsure about what disorder of arteries and arterioles non-specified means in their diagnosis, consulting a vascular specialist can provide clarity and a tailored treatment approach.
Preventative Measures and Lifestyle Modifications
Managing blood vessel disease involves a multifaceted approach, including lifestyle modifications and medical interventions. A heart-healthy diet rich in omega-3 fatty acids, fiber, and antioxidants can help reduce inflammation and plaque buildup in arteries. Regular physical activity enhances circulation and strengthens the cardiovascular system, lowering the risk of arterial stiffness and clot formation.
Smoking cessation is one of the most impactful steps in improving vascular health. Tobacco use accelerates arterial damage by promoting plaque accumulation and reducing blood vessel elasticity. Similarly, managing stress and maintaining a healthy weight contribute to overall vascular well-being.
In cases where lifestyle modifications are insufficient, medical interventions such as angioplasty, stenting, or bypass surgery may be necessary to restore proper blood flow. Medications such as anticoagulants, cholesterol-lowering drugs, and antihypertensives also play a crucial role in disease management.
Frequently Asked Questions (FAQ) on Blood Vessel Disease
1. What are the early warning signs of blood vessel disease?
Early signs of blood vessel disease can vary based on the specific condition but often include symptoms such as persistent numbness or tingling in the extremities, slow-healing wounds, and noticeable skin discoloration. Many people experience leg cramps during physical activity, which can indicate restricted blood flow, a hallmark of peripheral artery disease. Some individuals report unusual fatigue or shortness of breath, particularly when engaging in activities that previously did not cause discomfort. Swelling in the lower legs, feet, or hands can also suggest vascular problems, particularly if accompanied by visible veins or discoloration. Recognizing these early warning signs and seeking medical evaluation can help prevent the progression of vascular disease and reduce the risk of severe complications such as strokes or heart attacks.
2. What does disorder of arteries and arterioles unspecified mean in a medical diagnosis?
A diagnosis of disorder of arteries and arterioles unspecified means that there is an abnormality affecting these small blood vessels, but the specific cause or nature of the disorder has not been fully determined. This diagnosis is often given when a patient exhibits symptoms of vascular dysfunction, such as poor circulation or arterial narrowing, but further tests are needed to pinpoint the exact underlying condition. Possible causes may include early-stage atherosclerosis, inflammation of the arteries (vasculitis), or genetic predispositions to vascular disease. In many cases, additional diagnostic imaging or laboratory tests are required to better understand the severity and implications of the condition. Addressing this diagnosis typically involves managing underlying risk factors such as hypertension, diabetes, and cholesterol levels to prevent further arterial damage.
3. What disease makes arteries in the arms visible through skin?
There are several conditions that can cause arteries in the arms to become more visible through the skin, ranging from benign to more serious medical concerns. One common cause is low body fat, which reduces the amount of tissue covering the blood vessels, making them more prominent. However, certain vascular conditions, such as chronic venous insufficiency or arterial stenosis, can also lead to visible arteries, especially if accompanied by swelling or changes in skin texture. In some cases, connective tissue disorders such as Ehlers-Danlos syndrome can contribute to fragile blood vessels that appear more prominent. If an individual notices a sudden change in the appearance of their veins or arteries, particularly if accompanied by pain or discoloration, it is advisable to seek medical evaluation to rule out an underlying vascular disease.
4. What are the most common vascular disease symptoms?
Vascular disease symptoms vary widely depending on the affected blood vessels and the severity of the condition. Common symptoms include persistent leg pain or cramping, cold extremities, slow-healing wounds, and unexplained skin discoloration. Many individuals experience swelling in their lower limbs, particularly after prolonged periods of standing or sitting, which can indicate venous insufficiency. More severe symptoms, such as chest pain, difficulty breathing, or neurological impairments like sudden dizziness or confusion, may signal a serious vascular event such as a stroke or heart attack. Because vascular disease can progress silently for years before symptoms become noticeable, regular medical check-ups and early intervention are essential in preventing complications.
5. How does blood vessel disease increase the risk of a heart attack?
Blood vessel disease significantly elevates the risk of a heart attack by causing narrowing, blockages, or reduced elasticity in the arteries that supply the heart with oxygen-rich blood. When plaque accumulates inside the arteries, a condition known as atherosclerosis, it restricts blood flow and increases the likelihood of clot formation. If a clot completely obstructs a coronary artery, it can trigger a heart attack. In some cases, individuals experiencing arm veins heart attack symptoms—such as swelling, pain, or prominent veins in the upper extremities—may have an underlying vascular condition contributing to their cardiac risk. Managing blood vessel disease through lifestyle modifications, medication, and medical procedures can help prevent heart attacks and improve overall cardiovascular health.
6. What lifestyle changes can help prevent vascular disease?
Preventing vascular disease involves making lifestyle modifications that promote healthy circulation and reduce the risk of arterial damage. One of the most effective steps is adopting a heart-healthy diet rich in whole grains, lean proteins, and healthy fats while minimizing processed foods, trans fats, and excessive sugar intake. Regular physical activity, such as walking, swimming, or cycling, strengthens the cardiovascular system and improves blood flow. Smoking cessation is crucial, as tobacco use damages blood vessel walls and accelerates plaque buildup. Managing stress through mindfulness techniques, adequate sleep, and relaxation exercises can also reduce vascular strain. For individuals at higher risk, routine medical check-ups and vascular screenings can detect potential problems early, allowing for timely intervention.
7. What does disorder of arteries and arterioles non specified mean?
A disorder of arteries and arterioles non specified means that a patient has been diagnosed with an issue affecting small blood vessels, but the exact cause has not yet been determined. This diagnosis is often used when symptoms such as poor circulation, abnormal blood pressure fluctuations, or unexplained swelling suggest vascular dysfunction without a clear underlying pathology. Additional tests, such as Doppler ultrasounds, angiography, or laboratory assessments, may be required to pinpoint the cause. Conditions such as vasculitis, arterial blockages, or undiagnosed metabolic disorders can all contribute to this type of vascular dysfunction. Seeking specialist care can help clarify the diagnosis and guide treatment options to prevent disease progression.
8. Can blood vessel disease cause neurological symptoms?
Yes, blood vessel disease can lead to neurological symptoms when it affects the arteries supplying blood to the brain. Carotid artery disease, for instance, occurs when plaque buildup narrows the carotid arteries, reducing blood flow and increasing the risk of transient ischemic attacks (TIAs) or full-blown strokes. Symptoms such as sudden dizziness, confusion, vision disturbances, or difficulty speaking can indicate compromised blood flow to the brain. In cases of small vessel disease, which affects the tiny arteries within the brain, patients may experience cognitive decline, memory problems, or difficulties with motor function over time. Early detection and management of vascular disease can help reduce the risk of serious neurological complications.
9. Are visible veins always a sign of vascular disease?
Visible veins are not always an indicator of vascular disease, as they can be influenced by factors such as genetics, low body fat, or physical activity levels. However, in some cases, veins that become increasingly prominent over time, particularly if accompanied by swelling, pain, or skin changes, may indicate underlying vascular issues. Chronic venous insufficiency, for example, can cause veins to enlarge and become more noticeable due to poor circulation. Conditions such as deep vein thrombosis (DVT) can also lead to visible veins and swelling, requiring immediate medical evaluation. Individuals concerned about new or worsening vascular changes should seek medical advice to rule out potential circulatory problems.
10. How is blood vessel disease diagnosed?
Diagnosing blood vessel disease typically involves a combination of medical history assessment, physical examination, and specialized tests. Physicians may use imaging techniques such as Doppler ultrasound, CT angiography, or MRI scans to evaluate blood flow and detect blockages or abnormalities in the vessels. Blood tests may also be conducted to assess cholesterol levels, inflammation markers, and blood clotting tendencies. In some cases, stress tests or electrocardiograms (ECGs) are used to assess cardiovascular function. Early detection through regular screenings is crucial for managing vascular disease effectively and preventing serious complications such as strokes, heart attacks, or limb ischemia.
Conclusion: Taking Charge of Vascular Health
Blood vessel disease, though potentially life-threatening, is manageable with proper awareness, lifestyle adjustments, and timely medical intervention. Understanding vascular disease symptoms and recognizing when to seek help can significantly improve patient outcomes. Whether dealing with peripheral artery disease, carotid artery disease, or an unspecified disorder of arteries and arterioles, taking proactive steps in vascular health maintenance is essential. By prioritizing regular check-ups, leading a heart-conscious lifestyle, and seeking medical advice when necessary, individuals can significantly reduce their risk of severe vascular complications and enhance their overall well-being.
vascular health, circulatory system disorders, artery disease symptoms, venous insufficiency, cardiovascular risk factors, poor circulation remedies, peripheral artery health, heart disease prevention, chronic vein conditions, early signs of stroke, deep vein thrombosis awareness, high blood pressure effects, blood clot prevention, atherosclerosis management, arterial blockages, leg pain and circulation, improving blood flow, signs of poor vascular health, managing heart attack risks, blood vessel function
Further Reading:
Vascular Disease (Vasculopathy)
What to know about coronary artery disease
Cardiovascular diseases (CVDs)
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


