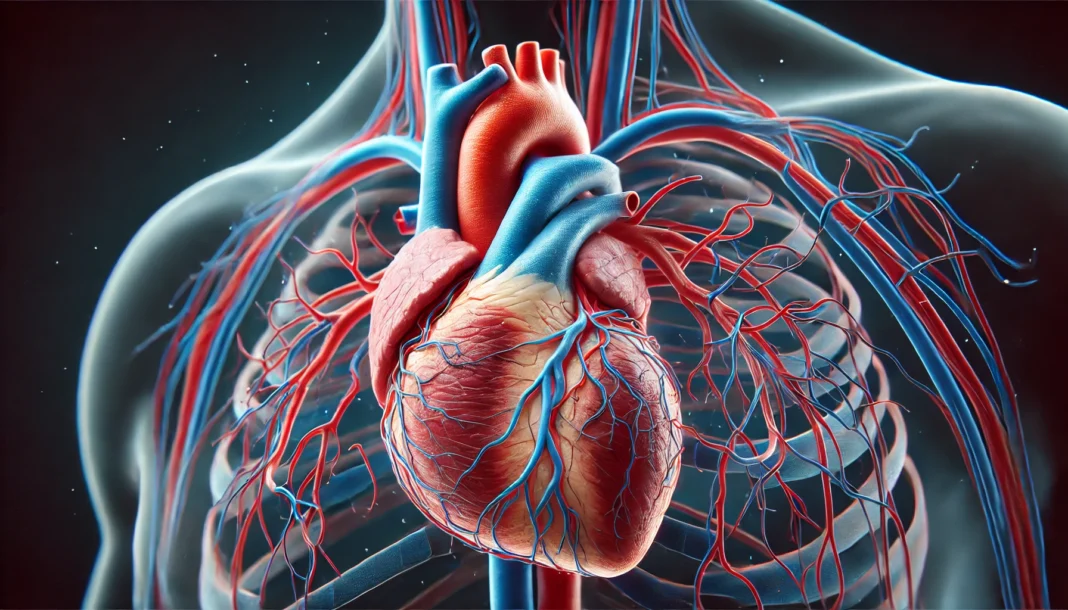
The human heart is not just a symbol of emotion; it is a biological marvel, functioning with intricate precision to sustain life. Central to this process are the vessels that nourish and cleanse the heart muscle—the arteries and veins of the coronary circulation. While much public and clinical attention has historically been directed at coronary arteries, a deeper understanding of the venous components—specifically the cardiac veins and coronary veins—reveals a rich and critical dimension of cardiovascular health. This article delves into the structure, function, clinical significance, and evolving understanding of these vital venous pathways, underscoring their indispensable role in maintaining myocardial homeostasis and overall circulatory balance.
You may also like: How to Naturally Reverse 20 Years of Arterial Plaque: Science-Backed Strategies for a Healthier Heart

Anatomy and Distinction Between Cardiac and Coronary Veins
In medical literature, the terms “cardiac veins” and “coronary veins” are often used interchangeably, though subtle distinctions exist. Cardiac veins refer broadly to the venous structures that drain the myocardium, the muscular tissue of the heart. Coronary veins, on the other hand, more specifically denote the subset of these veins that align with the coronary arteries, forming the venous complement of the coronary circulation. The primary purpose of both is to return deoxygenated blood from the myocardium to the right atrium of the heart, predominantly through the coronary sinus.
The major veins involved include the great cardiac vein, which ascends along the anterior interventricular sulcus and runs parallel to the left anterior descending artery. The middle cardiac vein courses through the posterior interventricular sulcus, while the small cardiac vein travels along the right margin of the heart. These veins converge into the coronary sinus, a broad venous channel situated in the posterior atrioventricular groove. The anterior cardiac veins bypass the coronary sinus and drain directly into the right atrium. Additionally, small veins called thebesian veins directly empty into the cardiac chambers, providing supplementary drainage.
This venous architecture is not simply structural; it reflects the heart’s functional demand for efficient waste clearance, thermoregulation, and pressure modulation. The design ensures that deoxygenated blood is swiftly removed from the myocardium, facilitating continuous, high-performance muscle contraction without toxic metabolic buildup.
Physiological Role in Cardiovascular Function
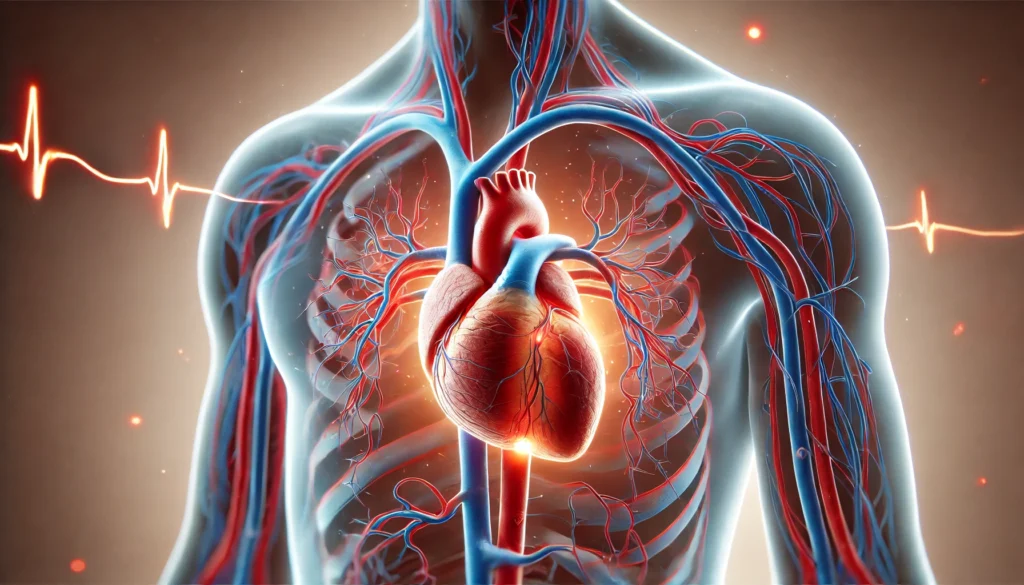
The role of cardiac veins in cardiovascular physiology is often underestimated. These veins are pivotal in maintaining the delicate balance between oxygen delivery and carbon dioxide removal within myocardial tissues. While coronary arteries are responsible for oxygen and nutrient delivery, it is the coronary veins that ensure the timely removal of metabolic byproducts, preventing ischemic injury and allowing the heart to perform consistently under varying physiological demands.
During periods of increased cardiac output, such as exercise or emotional stress, the myocardium’s metabolic activity intensifies. The cardiac veins must accommodate increased venous return without compromising the efficiency of drainage. This capacity for dynamic adaptation is achieved through intrinsic mechanisms of venous tone modulation and pressure-volume responsiveness, which are finely tuned by autonomic inputs and local metabolic factors.
Additionally, cardiac and coronary veins contribute to the heart’s thermal homeostasis. The continuous blood flow helps dissipate heat generated during high-frequency contractions, thereby preventing thermal-induced myocardial dysfunction. Moreover, these veins facilitate the transport of myocardial-derived hormones, such as atrial natriuretic peptide (ANP), which plays a role in blood volume regulation and systemic vascular resistance. Thus, cardiac veins are not passive conduits but active agents in maintaining cardiovascular equilibrium.
Clinical Relevance and Pathological Considerations
Although diseases involving coronary arteries are more commonly recognized, venous pathologies also bear significant clinical weight. One such condition is coronary sinus thrombosis, a rare but potentially fatal event often precipitated by central venous catheterization, hypercoagulable states, or cardiac infections. Symptoms may include chest pain, dyspnea, and hemodynamic instability, and if left untreated, may result in pericardial tamponade or right heart failure. Prompt diagnosis using imaging techniques such as transesophageal echocardiography or contrast-enhanced CT is critical for successful intervention.
Congenital anomalies also contribute to coronary venous disorders. Persistent left superior vena cava, coronary sinus ostial atresia, and unroofed coronary sinus syndrome can result in abnormal venous return and altered hemodynamics. These anomalies often manifest as arrhythmias, exercise intolerance, or cyanosis in children and young adults. Accurate diagnosis and anatomical delineation are essential for surgical correction or catheter-based management.
In addition, the coronary venous system plays an integral role in cardiac electrophysiology procedures. Cardiac resynchronization therapy (CRT), a cornerstone treatment for heart failure with reduced ejection fraction, relies on the placement of pacing leads within the coronary venous tributaries. These leads, advanced through the coronary sinus, stimulate the left ventricle to restore synchronized contraction. The efficacy of CRT is significantly influenced by the anatomy and patency of the coronary veins, making their understanding imperative for procedural planning and optimization.
Innovations in Imaging and Diagnostic Tools
Modern cardiovascular imaging has revolutionized the visualization of coronary veins, enabling more accurate diagnosis and intervention. Technologies such as multidetector computed tomography (MDCT), cardiac magnetic resonance imaging (MRI), and three-dimensional rotational venography have significantly improved the resolution and clarity of venous structures.
MDCT is particularly valuable in mapping venous anatomy preoperatively. It offers high spatial resolution and rapid acquisition, facilitating the identification of venous anomalies and thrombi. Cardiac MRI, with its superior soft tissue contrast and absence of ionizing radiation, is ideal for functional assessments, particularly in evaluating myocardial perfusion and viability. Contrast-enhanced MR venography allows clinicians to assess the patency and architecture of the coronary sinus and its tributaries with remarkable detail.
These imaging advancements have not only enhanced the safety and efficacy of interventions such as CRT and electrophysiology ablations but have also expanded the diagnostic toolkit for congenital venous anomalies. Furthermore, the integration of real-time imaging with catheter-based interventions—guided by fluoroscopy or electroanatomical mapping—continues to improve procedural precision and outcomes.
Therapeutic Applications and Interventional Access
The accessibility of the coronary venous system has led to its increasing use as a therapeutic conduit. In addition to CRT, coronary veins serve as a delivery route for gene therapy, stem cell transplantation, and targeted pharmacologic agents. These approaches are particularly relevant in the treatment of ischemic cardiomyopathy, where localized myocardial regeneration or angiogenesis may offer substantial benefit.
Venous access allows for localized delivery with minimal systemic exposure, reducing the risk of off-target effects. For instance, gene therapy aimed at enhancing myocardial calcium handling or promoting vascular endothelial growth factor (VEGF) expression can be administered through retrograde coronary venous perfusion. This method ensures maximal therapeutic concentration at the site of injury while preserving systemic safety.
Similarly, stem cell therapies delivered via the coronary sinus aim to repopulate infarcted regions with functional cardiomyocytes or supportive stromal cells. Preliminary studies have shown promise in improving left ventricular function and reducing scar burden, although long-term data and standardized protocols are still evolving. As these therapeutic strategies mature, the coronary venous system will likely remain a critical avenue for innovation.
Pathophysiological Impact of Venous Dysfunction
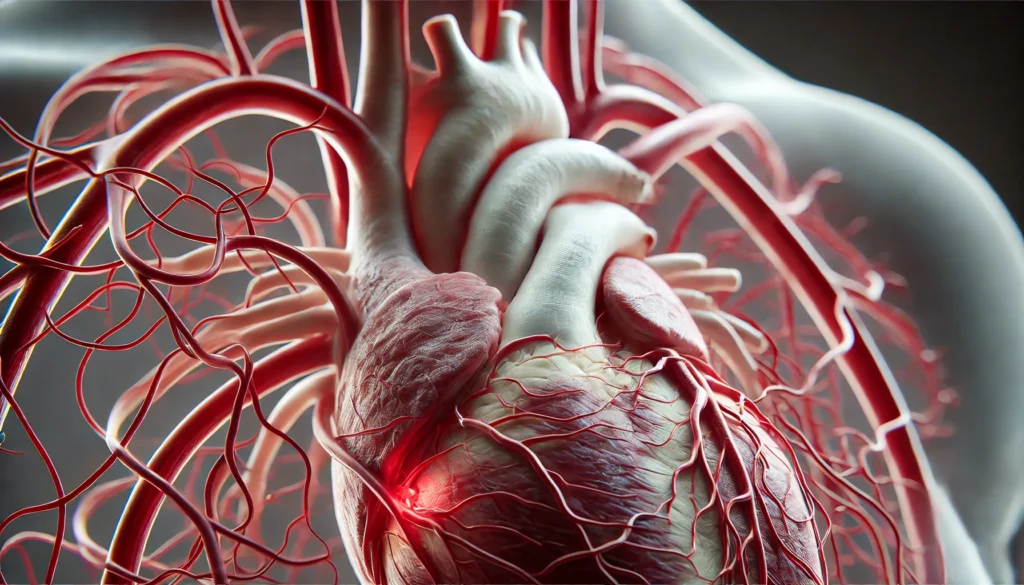
Venous dysfunction within the heart can lead to a cascade of detrimental effects. When venous return is impaired, whether due to thrombosis, external compression, or structural anomalies, the resultant congestion elevates intracardiac pressures. This pressure buildup can decrease coronary perfusion gradient, particularly during diastole, impairing myocardial oxygenation and contractility.
Over time, chronic venous hypertension can induce myocardial edema, disrupt extracellular matrix architecture, and impair electrophysiological conduction. These changes may manifest clinically as arrhythmias, reduced ejection fraction, and exercise intolerance. In right-sided heart failure, increased venous pressure often results in systemic venous congestion, hepatomegaly, ascites, and peripheral edema.
Early recognition and management of venous congestion are thus critical. Strategies may include optimizing preload with diuretics, reducing afterload through vasodilators, and, in select cases, mechanical decompression via pericardial drainage or surgical intervention. The goal is to restore venous patency, relieve myocardial stress, and preserve cardiac function.
Evolutionary and Comparative Perspectives
The development of a robust coronary venous system is a testament to evolutionary pressures favoring efficient cardiac performance. In mammals and birds, which exhibit high metabolic rates and sustained cardiac output, the venous system has evolved to maximize drainage and thermal regulation. The coronary sinus, nearly universal among vertebrates with a four-chambered heart, serves as a central channel integrating multiple venous pathways.
Comparative studies reveal that in lower vertebrates such as amphibians and reptiles, the absence of a coronary sinus is offset by alternative venous routes, reflecting diverse evolutionary adaptations. The presence of extensive thebesian veins in some species illustrates an evolutionary redundancy that ensures venous return even in the face of structural variations.
These insights not only enhance our understanding of human anatomy but also provide a foundation for modeling cardiovascular diseases and testing therapeutic interventions in animal systems. The study of evolutionary biology thus remains an important complement to clinical and translational cardiology.
Molecular and Cellular Characteristics of Venous Endothelium
At the cellular level, the endothelium of cardiac and coronary veins exhibits unique properties that influence vascular tone, permeability, and inflammatory responses. Unlike arterial endothelium, venous endothelial cells express different profiles of nitric oxide synthase, adhesion molecules, and growth factor receptors. These molecular distinctions play a role in regulating venous capacitance and leukocyte trafficking.
In pathological states, such as myocardial infarction or myocarditis, venous endothelial cells participate in the local immune response. They release cytokines, present antigens, and interact with circulating immune cells. This interaction can be either protective—facilitating tissue repair—or harmful, promoting fibrosis and scarring.
Recent research has also identified the role of venous endothelium in angiogenesis. Under hypoxic conditions, these cells upregulate pro-angiogenic signals, contributing to collateral vessel formation and tissue regeneration. Understanding these pathways may yield novel therapies for ischemic heart disease, including modulation of endothelial behavior through pharmacological or genetic means.
Preventive and Public Health Implications
While much emphasis is placed on preventing arterial disease, maintaining venous health is equally critical. Lifestyle factors such as regular exercise, adequate hydration, and avoidance of prolonged immobility support venous return and reduce the risk of thrombotic events. Managing comorbidities like hypertension, diabetes, and obesity further alleviates stress on the venous system.
Public health initiatives should incorporate education on venous risk factors and encourage early screening for individuals with familial or occupational predispositions. Healthcare providers can use non-invasive tools like Doppler ultrasonography or impedance cardiography to monitor venous flow in at-risk populations.
In hospital settings, particularly among critically ill or immobilized patients, vigilance against venous thromboembolism (VTE) includes prophylactic anticoagulation, mechanical compression devices, and early mobilization. These strategies not only prevent deep vein thrombosis but also protect against secondary cardiac complications stemming from impaired venous return.
Educational Priorities in Medical Training
Medical curricula must emphasize a balanced understanding of both arterial and venous systems. Enhanced focus on the anatomy, physiology, and pathology of cardiac veins prepares future clinicians to recognize and manage complex cardiovascular conditions holistically.
Interactive tools such as 3D models, virtual dissection, and simulation-based training can augment traditional lectures, fostering a deeper appreciation for venous anatomy. Case-based learning, incorporating real-world scenarios of CRT, congenital anomalies, or venous thrombosis, reinforces clinical relevance and decision-making skills.
Continued education through journals, conferences, and online platforms ensures that clinicians remain abreast of emerging research and evolving standards of care. As therapeutic options expand, particularly in interventional cardiology and regenerative medicine, a thorough grounding in coronary venous systems becomes indispensable.
Frequently Asked Questions: Cardiac and Coronary Veins
1. Can poor posture or sedentary behavior affect cardiac vein function over time?
Yes, prolonged sedentary behavior and poor posture can indirectly impact the efficiency of cardiac vein function. When a person remains seated or reclined for extended periods, venous return from the periphery to the heart can slow down, particularly through lower extremity veins. While the cardiac veins themselves are not directly compressed, chronic under-circulation can contribute to systemic venous hypertension. Over time, this can alter intracardiac pressure gradients, influencing how efficiently the coronary veins drain deoxygenated blood from the myocardium. Regular movement and posture correction may help maintain optimal hemodynamic conditions that support healthy cardiac and coronary vein flow.
2. Are there any nutritional strategies that support the health of coronary veins?
Nutritional strategies aimed at reducing inflammation and improving endothelial health may support the optimal function of coronary veins. Diets rich in omega-3 fatty acids, flavonoids, and antioxidants can promote vascular flexibility and reduce oxidative stress, which benefits both arterial and venous structures. While most nutritional advice focuses on arterial health, maintaining the endothelium of the coronary veins is equally critical for efficient venous return and pressure regulation. Nutrients like magnesium, potassium, and vitamin K2 have shown promise in modulating vascular tone and preventing calcification, which could extend benefits to the venous system. Thus, a heart-healthy diet indirectly contributes to sustaining the long-term function of cardiac veins.
3. How do cardiac and coronary veins change with aging, and what are the implications?
As we age, the elasticity and compliance of vascular structures, including cardiac and coronary veins, decline. This stiffening can lead to delayed or impaired venous drainage from the myocardium, resulting in inefficient removal of metabolic waste. Age-related endothelial dysfunction also affects the coronary veins, increasing the risk of thrombosis and venous congestion. Reduced venous compliance may exacerbate symptoms of heart failure in older adults by compromising preload management. Understanding these age-related changes emphasizes the importance of early lifestyle interventions and monitoring to preserve cardiac vein health well into advanced age.
4. Can lifestyle interventions like yoga or deep breathing affect coronary vein drainage?
Yes, activities that influence autonomic tone—such as yoga, meditation, and deep breathing—can positively affect coronary vein drainage. These practices stimulate the parasympathetic nervous system, which can lead to vasodilation and improved venous return. While evidence specifically targeting cardiac veins is still emerging, broader research on venous tone regulation suggests that mindful breathing techniques may optimize pressure gradients that facilitate venous drainage. By lowering systemic blood pressure and improving heart rate variability, these interventions help balance arterial inflow and venous outflow, supporting the role of coronary veins in maintaining circulatory homeostasis. Thus, integrating stress-reduction techniques can complement cardiovascular care in a non-invasive manner.
5. How might cardiac and coronary veins be affected in patients with chronic lung conditions?
Chronic lung diseases such as COPD or pulmonary hypertension can significantly affect the function of cardiac and coronary veins. Elevated pulmonary pressures increase right ventricular afterload, which in turn can cause backpressure on the venous system, including the coronary sinus and cardiac veins. In severe cases, this may result in impaired drainage of the coronary veins, potentially contributing to myocardial hypoxia despite adequate arterial inflow. Furthermore, oxygen desaturation associated with chronic respiratory disease exacerbates venous endothelial dysfunction, making the system more vulnerable to congestion and thrombosis. Comprehensive cardiopulmonary management is therefore essential to protect the integrity of cardiac venous return in these patients.
6. Are there early signs that might suggest dysfunction of the cardiac venous system?
Unlike arterial diseases, which often present with chest pain or claudication, dysfunction in cardiac veins can manifest more subtly. Patients might experience unexplained fatigue, reduced exercise tolerance, or palpitations without clear arterial blockages. In electrophysiology, abnormal lead resistance during CRT device implantation may indicate anatomical obstruction or narrowing within the coronary veins. Additionally, subtle ECG changes or imaging anomalies in venous flow patterns can be early clues. Clinical suspicion combined with targeted imaging such as venography or cardiac MRI can help detect venous system issues before they evolve into more significant complications.
7. Can coronary veins be genetically predisposed to anomalies or dysfunction?
Yes, some individuals have congenital anomalies of the coronary veins that can affect drainage and cardiac performance. These may include persistent left superior vena cava, unroofed coronary sinus, or coronary sinus atresia, all of which can disrupt the normal flow of blood through the cardiac venous system. While these conditions are rare, they can be inherited and may go undetected until cardiac imaging is performed for unrelated symptoms. Advances in genetic mapping and imaging techniques are helping to identify these predispositions earlier. Understanding family history and considering genetic screening can be important, especially in patients with otherwise unexplained arrhythmias or exercise intolerance.
8. How do the coronary veins interact with mechanical support devices like LVADs?
In patients who require left ventricular assist devices (LVADs), the dynamics of the coronary venous system can be significantly altered. These devices unload the left ventricle, potentially changing the pressure gradients that drive venous return via the coronary veins. In some cases, the altered hemodynamics can impair coronary sinus drainage or affect CRT lead placement if resynchronization is also being employed. Moreover, the interaction between continuous-flow devices and the pulsatile nature of venous return introduces unique challenges in maintaining adequate myocardial perfusion and clearance. A multidisciplinary approach that includes venous anatomy in procedural planning helps ensure optimal outcomes for LVAD patients.
9. What role do coronary veins play in cardiac arrhythmias and their management?
The coronary venous system plays an important yet underappreciated role in the genesis and treatment of arrhythmias. Veins such as the coronary sinus are common access points for electrophysiological studies and ablation procedures. Abnormal anatomy or flow within the cardiac veins can influence the substrate for arrhythmogenesis, particularly in cases of atrial fibrillation or ventricular tachycardia. Venous congestion can alter the electrical properties of the myocardium by promoting fibrosis or disrupting cellular communication. Understanding the venous component in arrhythmic circuits allows clinicians to tailor interventions with greater precision, improving the efficacy of catheter-based therapies.
10. How might future technologies enhance our understanding of cardiac vein function?
Emerging technologies like 4D flow MRI and molecular imaging are poised to revolutionize how we study the function of cardiac and coronary veins. These tools allow for real-time assessment of blood flow patterns and wall shear stress within the coronary venous system, offering a dynamic perspective on physiological changes. Additionally, machine learning algorithms can analyze venous flow data to predict complications or optimize lead placement in CRT procedures. Nanotechnology may also enable targeted drug delivery via coronary veins, opening doors to highly localized therapies for heart failure or ischemia. As innovation accelerates, our appreciation of the cardiac venous system will deepen, further bridging the gap between anatomy and clinical application.
Conclusion: Embracing the Clinical Significance of Cardiac and Coronary Veins in Heart Health
The cardiac veins and coronary veins, once viewed as passive conduits, are now recognized as dynamic players in cardiovascular function and disease. Their roles in waste removal, thermal regulation, hormone transport, and therapeutic access position them as critical components of the circulatory system. With growing clinical applications—from cardiac resynchronization to gene therapy—their significance continues to expand.
Understanding these venous structures not only enhances our grasp of cardiac physiology but also informs a more comprehensive approach to cardiovascular care. By embracing the complexity and utility of cardiac and coronary veins, clinicians, researchers, and educators can drive forward innovations in diagnosis, treatment, and prevention.
As we refine imaging techniques, develop targeted therapies, and deepen our molecular understanding, the cardiac venous system promises to play an even more prominent role in the future of medicine. Heart health depends not only on robust arterial supply but also on efficient venous return—a truth that reinforces the importance of holistic cardiovascular care.
myocardial circulation, heart muscle drainage, venous return to the heart, coronary sinus function, cardiovascular anatomy, heart failure management, cardiac imaging techniques, electrophysiology procedures, heart rhythm disorders, cardiac resynchronization therapy, myocardial perfusion imaging, endothelial function in veins, heart disease diagnostics, vascular health and aging, cardiac catheter interventions, chronic venous insufficiency, cardiovascular therapeutic innovations, cardiac gene therapy delivery, venous anomalies in the heart, heart-lung circulation disorders
Further Reading:
Cardiac veins, an anatomical review
Heart Anatomy, Function, and Blood Circulation
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.