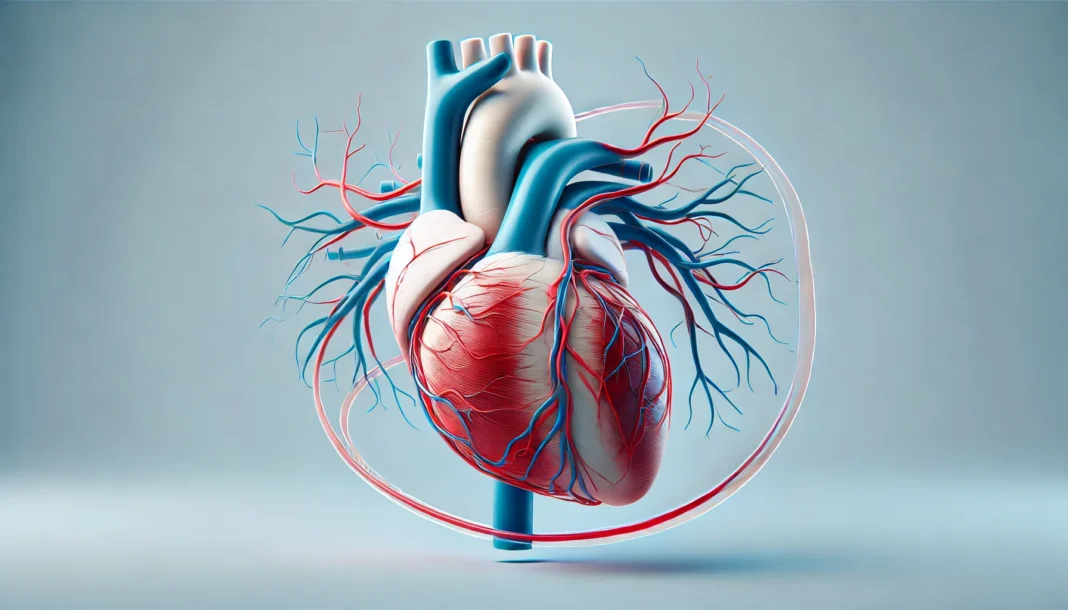
Introduction: The Vital Role of Coronary Circulation in Cardiovascular Health
The heart is an extraordinary organ—unceasing, muscular, and responsible for pumping life-sustaining blood to every part of the human body. Yet, what enables the heart itself to stay nourished and oxygenated? This vital task is carried out by a sophisticated network of coronary vessels, which supply the heart muscle (myocardium) with the blood it needs to function. Known collectively as coronary circulation, this system ensures that oxygen-rich blood is delivered to the heart’s muscular tissue while simultaneously removing metabolic waste. Understanding the intricacies of coronary artery anatomy is not just an academic exercise; it is essential for diagnosing, preventing, and managing cardiovascular disorders that can jeopardize human life.
You may also like: How to Naturally Reverse 20 Years of Arterial Plaque: Science-Backed Strategies for a Healthier Heart
In this comprehensive guide, we delve into the anatomy of cardiac arteries, explore what each artery supplies, and unravel the physiological nuances that make this system so indispensable. We also tackle common questions like “how many arteries in the heart?” and provide context for terms such as the left main coronary artery (LMCA), the LAD artery, and the RCA coronary artery. With a blend of advanced clinical insights and accessible language, this article aims to educate college-level readers and health-conscious individuals alike about coronary heart anatomy and its practical implications for lifelong cardiovascular health.
An Overview of Coronary Anatomy: Understanding the Layout of Heart Arteries
Coronary circulation refers to the movement of blood through the coronary vessels, which branch from the aorta and encircle the heart like a crown—a fitting image, as the term “coronary” is derived from the Latin word for crown. This circulation is essential for delivering oxygen and nutrients to the heart muscle itself, which paradoxically cannot be nourished by the very blood it pumps to the rest of the body. Thus, the heart relies on its own dedicated vascular system: the coronary arteries.
The principal components of coronary circulation include two primary coronary arteries: the right coronary artery and the left coronary artery. These arteries originate from the root of the aorta, just above the aortic valve, in the sinuses of Valsalva. From their origin points, they branch out into smaller arteries that distribute blood to various regions of the heart. The complexity of this vascular tree is what allows the heart to maintain functionality even under stress or partial obstruction. Each artery plays a unique and vital role in this tightly regulated system.
The left main coronary artery, or LMCA artery, bifurcates into the left anterior descending artery and the circumflex branch of the left coronary artery. Meanwhile, the right coronary artery supplies the right side of the heart and contributes to the posterior descending artery in most individuals. This anatomy ensures that both atria and ventricles receive sufficient blood flow tailored to their metabolic demands. When examining a coronary artery diagram, one appreciates how the precise layout of these vessels supports the synchronized contractions of the cardiac cycle.
Understanding coronary vessel anatomy not only deepens our knowledge of cardiovascular physiology but also lays the foundation for recognizing pathological changes such as stenosis or atherosclerosis. By grasping the anatomical and functional distinctions among these arteries, clinicians and students alike can better appreciate the delicate balance that governs heart health.
The Left Coronary Artery: Gateway to the Left Side of the Heart
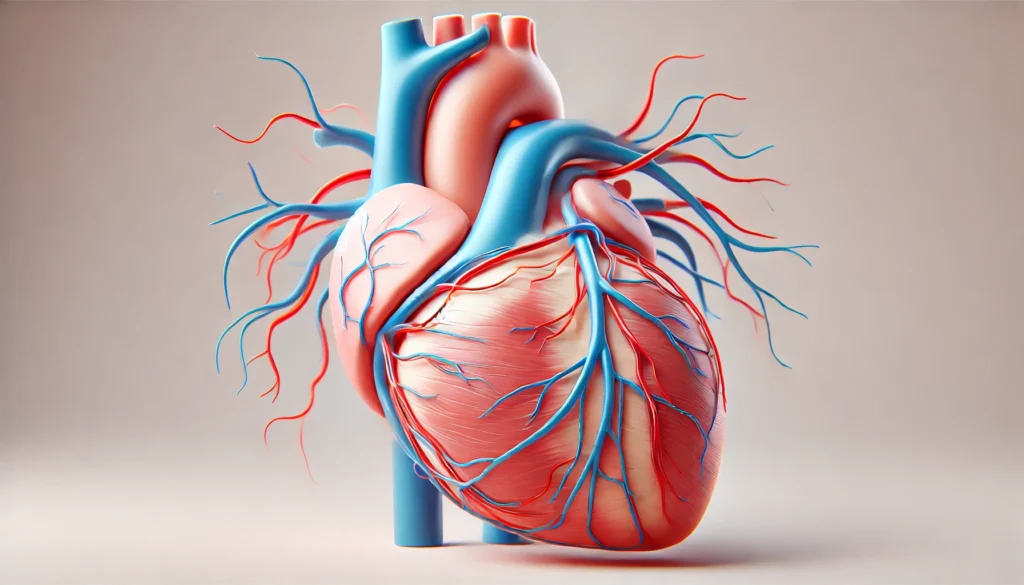
Among the most significant vessels in the coronary circulation is the left coronary artery, which is responsible for perfusing much of the left side of the heart—the side that propels oxygenated blood into systemic circulation. The left coronary artery originates from the left aortic sinus and typically has a short main trunk before dividing into two major branches: the left anterior descending artery and the circumflex branch of the left coronary artery.
The left main artery is often described as the most critical segment of coronary vasculature. Occlusion of this artery can lead to massive myocardial infarction or sudden cardiac death, underscoring its clinical importance. It gives rise to the LAD coronary artery, which travels down the anterior interventricular sulcus and supplies the anterior wall of the left ventricle, the interventricular septum, and part of the apex of the heart. Because of its central role in perfusing high-demand myocardial regions, the LAD artery is sometimes ominously nicknamed the “widowmaker.”
The circumflex branch of the left coronary artery, on the other hand, curves around the left side of the heart in the atrioventricular groove and supplies blood to the lateral and posterior walls of the left ventricle and the left atrium. In some individuals, the circumflex artery may also give rise to the posterior descending artery, a condition known as left-dominant circulation.
Understanding what each artery supplies is crucial when interpreting cardiac imaging or planning surgical interventions such as coronary artery bypass grafting (CABG). In a broader sense, knowledge of coronary heart anatomy also plays a role in assessing risk factors for ischemic heart disease and tailoring treatment plans for patients with complex cardiovascular conditions.
The Right Coronary Artery: Sustaining the Right Heart and More
The right coronary artery, or RCA coronary artery, is equally essential despite supplying a smaller volume of myocardial tissue compared to its left-sided counterpart. Emerging from the right aortic sinus, the RCA courses through the right atrioventricular groove and gives rise to several key branches that supply various components of the heart, including the sinoatrial node, right atrium, right ventricle, and inferior portion of the left ventricle.
One of the major offshoots of the RCA is the posterior descending artery, which typically supplies the posterior one-third of the interventricular septum and the inferior wall of the left ventricle. In individuals with right-dominant circulation—which accounts for approximately 85% of the population—the RCA assumes an even more pivotal role, as it becomes the source of the posterior descending artery. This dominance determines the coronary arterial contribution to the posterior heart wall, a fact with significant implications for myocardial infarction localization.
The RCA also contributes to the atrioventricular nodal artery, which supplies the AV node, and occasionally the sinoatrial nodal artery in those without left-sided dominance. These contributions are critical for the electrical conduction system of the heart, making the RCA not just a supplier of blood but a gatekeeper of rhythm and timing.
The RCA’s function and its anatomical course must be thoroughly understood when assessing cardiac catheterization images or performing percutaneous coronary interventions. The interplay between the right and left coronary arteries ensures that the heart muscle receives redundant and collateral circulation, enhancing resilience against partial occlusions or blockages. The RCA coronary artery, though sometimes overshadowed in medical discussions, deserves equal recognition for its contributions to coronary circulation.
Exploring the LAD Artery: Anatomy, Function, and Clinical Relevance
The left anterior descending artery holds a unique place in cardiology due to its anatomical reach and clinical relevance. Also referred to as the LAD heart artery or simply LAD artery, this vessel runs along the anterior interventricular groove and delivers blood to the front wall of the left ventricle, most of the interventricular septum, and the apex of the heart.
An understanding of LAD coronary artery anatomy is essential when evaluating patients for coronary artery disease. Blockages in the LAD artery can lead to extensive myocardial damage due to its supply territory. Given its path along the anterior interventricular sulcus, the LAD artery is easily visualized in imaging studies and often targeted during interventions such as angioplasty and stenting.
Functionally, the LAD artery supports a major portion of the cardiac output since it supplies regions involved in systolic contraction. The robustness of this artery correlates directly with the heart’s pumping efficiency. Hence, damage to the LAD artery can result in left ventricular dysfunction, congestive heart failure, or life-threatening arrhythmias.
Clinicians often refer to myocardial infarctions in the LAD territory as anterior wall MIs—conditions associated with higher morbidity and mortality. Knowledge of LAD heart anatomy not only aids in clinical diagnosis but also improves outcomes by enabling precise localization of ischemia.
Whether in surgical procedures, imaging interpretations, or clinical discussions, the LAD coronary artery remains central to conversations about heart artery anatomy. It serves as a striking example of how a single artery can have a profound impact on overall cardiovascular health.
Frequently Asked Questions About Coronary Circulation and Heart Artery Anatomy
What does the anterior interventricular artery contribute beyond basic blood supply?
The anterior interventricular artery, also known as the left anterior descending artery, plays a pivotal role in maintaining synchronized cardiac contractions. Beyond simply delivering oxygenated blood to the anterior interventricular septum, this artery significantly impacts the timing and coordination of left ventricular contraction, which is essential for efficient systolic function. Damage to this artery can impair the interventricular septum’s electrical conduction capabilities, making arrhythmias more likely in patients with ischemic heart disease. As modern imaging techniques improve, we are beginning to understand microvascular adaptations along the anterior interventricular artery that may modulate blood flow in response to chronic stress. These insights offer potential avenues for personalized interventions targeting the dynamics of coronary circulation in high-risk patients.
How does the right coronary artery influence cardiac rhythm regulation?
The right coronary artery does more than supply the right atrium and right ventricle—it plays an integral role in regulating cardiac rhythm. In many individuals, the right coronary artery provides the sinoatrial nodal branch and atrioventricular nodal artery, supplying the heart’s primary pacemakers. This unique anatomical positioning makes the RCA a critical structure in rhythm disorders such as bradycardia or heart block, particularly when ischemia or atherosclerosis develops in these nodal branches. Intriguingly, variability in coronary vessel anatomy can affect how arrhythmias present clinically, making a detailed understanding of the RCA coronary artery crucial for electrophysiologists. Advances in electro-anatomical mapping have shown that subtle anatomical deviations within RCA pathways can influence therapeutic outcomes for catheter ablation procedures.
Why do some patients develop symptoms even if the major coronary vessels are clear?
It’s increasingly recognized that coronary microvascular dysfunction can lead to anginal symptoms even when angiography reveals no significant obstruction in major coronary vessels. While the large heart arteries like the left coronary artery and right coronary artery are commonly assessed, the microvasculature embedded in the myocardial tissue also plays a vital role. In conditions such as microvascular angina or coronary vasospasm, these smaller vessels fail to dilate properly, leading to impaired coronary circulation despite a structurally normal coronary artery diagram. This phenomenon underscores the importance of evaluating not only coronary artery anatomy but also coronary function using advanced tools like coronary flow reserve (CFR) or stress perfusion MRI. In clinical practice, addressing these cases requires nuanced management strategies that differ from traditional atherosclerotic treatments.
How many arteries in the heart are considered clinically significant?
While there are technically multiple arteries branching off the left and right coronary systems, the number of clinically significant coronary arteries typically revolves around three: the left anterior descending, the circumflex branch of the left coronary artery, and the right coronary artery. However, this standard view simplifies the complexity of coronary heart anatomy, which can vary widely among individuals. For instance, the posterior descending artery may arise from either the right or the circumflex artery depending on coronary dominance, influencing perfusion patterns. Therefore, the answer to how many coronary arteries are there extends beyond a numeric count to include anatomical dominance, collateral circulation, and variation in branching. Understanding these nuances is especially important in procedures such as coronary artery bypass grafting, where surgical strategy depends on precise coronary vessel anatomy.
What emerging imaging techniques enhance our understanding of coronary anatomy?
Innovations in cardiac imaging have revolutionized our understanding of coronary artery anatomy and function. Coronary computed tomography angiography (CCTA) now offers high-resolution, non-invasive visualization of both the lumen and the wall of coronary arteries, allowing for earlier detection of atherosclerosis. Additionally, techniques such as 3D reconstruction of coronary artery diagrams provide detailed views of the left main coronary artery and its bifurcations, enabling more accurate procedural planning. Functional imaging, such as fractional flow reserve derived from CT (FFR-CT), assesses how narrowed vessels like the LAD artery affect blood flow dynamically. Moreover, intravascular ultrasound (IVUS) and optical coherence tomography (OCT) are now standard in interventional cardiology for assessing stent placement and identifying vulnerable plaques. These technologies are helping redefine what we know about coronary anatomy and its clinical applications.
Why is the LAD artery considered particularly vulnerable in cardiac events?
The LAD coronary artery supplies a substantial portion of the left ventricle, including critical regions such as the anterior wall, apex, and most of the interventricular septum. Because of this extensive coverage, occlusion in the LAD heart territory often results in large, anterior myocardial infarctions associated with high mortality. Compounding this vulnerability is the fact that the left anterior descending is often the site of early atherosclerotic plaque formation due to shear stress at its origin from the left main artery. Emerging research suggests that local endothelial dysfunction in the LAD artery contributes to early calcification and impaired vasodilation, compounding risk. Consequently, ongoing monitoring of LAD coronary artery health is essential in patients with metabolic syndrome or elevated inflammatory markers.
How does anatomical variation affect surgical interventions in coronary artery disease?
Anatomical variation in coronary vessel anatomy can significantly influence surgical planning and outcomes. For instance, in patients with a short LMCA artery or trifurcation (involving a ramus intermedius artery), decisions about graft placement during bypass surgery must be carefully tailored. Similarly, the presence of a left-dominant circulation—where the circumflex branch of the left coronary artery gives rise to the posterior descending artery—alters the ischemic risk profile and requires a different surgical approach. Understanding coronary anatomy in three dimensions through preoperative imaging has become an essential part of modern cardiac surgery protocols. These anatomical insights can also guide minimally invasive or robotic procedures that depend on precise mapping of coronary artery anatomy. Individualized surgical strategies rooted in anatomic detail often result in better outcomes and fewer complications.
Is the coronary artery the largest human artery, and what does its size imply?
Although critical in function, the coronary artery is not the largest human artery—that distinction belongs to the aorta. However, despite their smaller diameter, the coronary arteries wield an outsized influence on cardiovascular health due to their role in perfusing the myocardium. Because they are narrow and embedded within a constantly contracting organ, coronary arteries are more prone to dynamic changes in pressure and flow. This makes them susceptible to endothelial injury and plaque formation even when systemic arterial health appears stable. Their smaller size also implies that even minor stenoses can have significant physiological consequences, particularly in arteries such as the LAD artery or the LMCA artery, where perfusion demand is greatest.
What new therapeutic approaches target specific coronary vessels?
Advancements in cardiology have led to therapies that specifically address different segments of coronary circulation. Drug-eluting stents have become standard for treating lesions in the left anterior descending artery, especially near bifurcation points. In patients with disease in the left main coronary artery, techniques such as the double kissing crush or culotte stenting are used to ensure patency across branches. Moreover, therapies targeting microvascular function—like ranolazine or endothelial nitric oxide modulators—are being explored in patients with non-obstructive coronary artery disease. Hybrid revascularization procedures that combine minimally invasive surgical grafting with stenting are also emerging, especially for anatomically complex cases involving multiple heart arteries. These evolving strategies highlight how coronary artery anatomy directly informs tailored therapeutic decisions.
How does understanding coronary circulation improve long-term cardiovascular outcomes?
Deep knowledge of coronary circulation enhances not only acute care but also long-term disease management. For instance, recognizing early signs of reduced perfusion in coronary vessels can lead to preventive strategies such as aggressive lipid control or coronary calcium scoring. Patient-specific insights—like whether their posterior descending artery is supplied by the RCA coronary artery or the circumflex—allow clinicians to predict risk more accurately and adjust surveillance protocols. Furthermore, understanding how coronary anatomy changes over time, such as with aging or diabetes, enables dynamic treatment models rather than static algorithms. Longitudinal monitoring through imaging and biomarkers provides a window into evolving coronary vessel anatomy and facilitates timely interventions. Ultimately, familiarity with the intricacies of heart artery anatomy translates to more personalized, proactive care and improved quality of life for patients.
Conclusion: The Clinical and Anatomical Importance of Coronary Circulation
In conclusion, the heart’s intricate vascular system—the coronary circulation—is fundamental to sustaining life. Understanding the anatomy of cardiac arteries is not merely a scientific pursuit but a practical necessity for diagnosing and treating cardiovascular disease. The coronary vessels—including the left main artery, left anterior descending, right coronary artery, and circumflex branch—each contribute uniquely to myocardial function and overall cardiovascular health.
A deeper appreciation for coronary artery anatomy allows clinicians to anticipate complications, strategize interventions, and personalize treatment for patients with coronary artery disease. It also empowers patients to comprehend the implications of diagnostic imaging, surgical decisions, and lifestyle changes in the context of coronary anatomy. Whether exploring a coronary artery diagram or examining a cross-sectional view of the LAD heart artery, knowledge becomes the bridge between clinical theory and real-world application.
Questions like “how many coronary arteries are there” or “what is the function of the coronary circulation” are no longer abstract once placed within the lived experience of patient care and the physiological demands of the heart. The answer to “is coronary artery the largest human artery” may be no—since that title belongs to the aorta—but few arteries wield the clinical impact and complexity of those within the coronary network.
As cardiovascular disease remains a leading cause of death globally, the value of understanding coronary vessel anatomy cannot be overstated. It is not only a matter of scientific accuracy but a commitment to preserving life through insight, precision, and ongoing education. With this knowledge in hand, healthcare professionals and informed readers alike can better navigate the challenges and opportunities of heart health, guided by the roadmap of coronary anatomy.
cardiac blood flow, myocardial perfusion, heart muscle oxygenation, coronary artery disease risk factors, arterial plaque formation, cardiac catheterization, heart imaging techniques, blood supply to the myocardium, myocardial infarction pathophysiology, heart valve and artery interaction, cardiac ischemia mechanisms, myocardial energy demands, atherosclerotic heart disease, cardiac anatomy education, heart surgery planning, cardiac rhythm disorders, ventricular wall blood supply, cardiovascular diagnostics, coronary stent placement, angiographic interpretation
Further Reading:
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.