High blood pressure, medically known as hypertension, is a leading cause of cardiovascular complications and early mortality worldwide. Yet, when it comes to addressing this condition, gender-specific differences are often overlooked, particularly in women. The phenomenon of female high blood pressure is not only a significant public health concern but also a subject of growing interest in the medical community due to the unique hormonal, physiological, and lifestyle factors that influence its development and progression in women. Despite advancements in cardiovascular medicine, many women remain unaware of the risks, symptoms, and management strategies specifically relevant to them. In this article, we explore what high blood pressure means for women, how it manifests differently than in men, and what steps can be taken to reduce risk and improve health outcomes.
For too long, the general conversation around high blood pressure has defaulted to male-centric research and symptomology. However, recent studies have shed light on how high BP in women follows a different trajectory across the lifespan. The hormonal shifts that occur during pregnancy, perimenopause, and menopause can significantly impact vascular health and blood pressure regulation. Moreover, societal expectations and care disparities often result in women being underdiagnosed or undertreated for hypertension. Therefore, understanding the nuances of female high blood pressure is not just important for clinicians—it is essential for women themselves to advocate for their health.
Recognizing that high blood pressure in women is often less symptomatic in its early stages, the need for preventive awareness and routine monitoring becomes even more urgent. Many women may attribute symptoms like fatigue, headaches, or chest discomfort to stress or hormonal fluctuations, overlooking their potential cardiovascular significance. Furthermore, because hypertension can lead to severe complications such as heart attack, stroke, kidney failure, and dementia, timely identification and intervention are vital. This article not only addresses the scientific underpinnings of high blood pressure in women but also offers evidence-based strategies for management and prevention tailored to the female experience.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Hormonal Influences and Lifespan Risk Factors Unique to Women
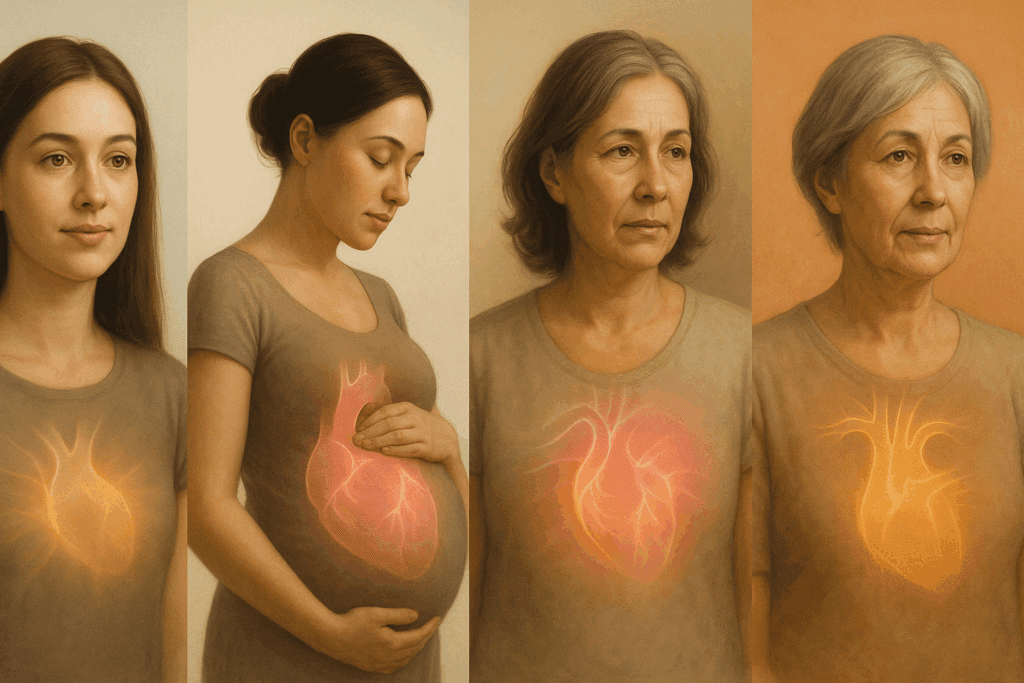
One of the most profound influences on female high blood pressure is the fluctuation of hormones throughout a woman’s life. Estrogen, which has vasodilatory properties, helps to keep blood vessels relaxed and pliable. During the reproductive years, this hormone plays a protective role in maintaining lower blood pressure. However, during menopause, estrogen levels decline sharply, leading to increased arterial stiffness and a greater propensity for hypertension. This transition, often accompanied by weight gain, sleep disturbances, and metabolic changes, creates a perfect storm for the development of high BP in women.
Pregnancy introduces another period of vulnerability. Conditions such as gestational hypertension and preeclampsia are exclusive to women and serve as early indicators of future cardiovascular issues. Women who experience high blood pressure during pregnancy are at a higher risk of developing chronic hypertension and heart disease later in life. These complications can also have lingering effects on the vascular system, contributing to sustained elevations in blood pressure long after childbirth.
The perimenopausal phase presents its own challenges. Women often report increased stress, changes in sleep patterns, and shifts in dietary habits during this time. These lifestyle changes, combined with hormonal alterations, can exacerbate the risk of developing high blood pressure. It is not uncommon for women to first be diagnosed with hypertension during their 40s or 50s, coinciding with this transitional phase. Recognizing this period as a critical window for intervention could be key to reducing long-term cardiovascular risk.
It is also important to consider how birth control pills, hormone replacement therapy, and fertility treatments may influence blood pressure. While oral contraceptives have been associated with elevated BP in some women, particularly those with a predisposition to cardiovascular conditions, the relationship between hormone therapies and blood pressure remains complex and individualized. A comprehensive understanding of a woman’s hormonal history, including any use of synthetic hormones, is vital in assessing her risk profile for hypertension.
Lastly, autoimmune diseases such as lupus and rheumatoid arthritis, which are more prevalent in women, can increase systemic inflammation and contribute to vascular damage. These conditions often coincide with higher rates of hypertension and cardiovascular complications. Therefore, female high blood pressure must be evaluated within a broader context that includes not only hormonal and reproductive factors but also immune function and chronic disease management.
Why Symptoms of High Blood Pressure May Be Missed in Women
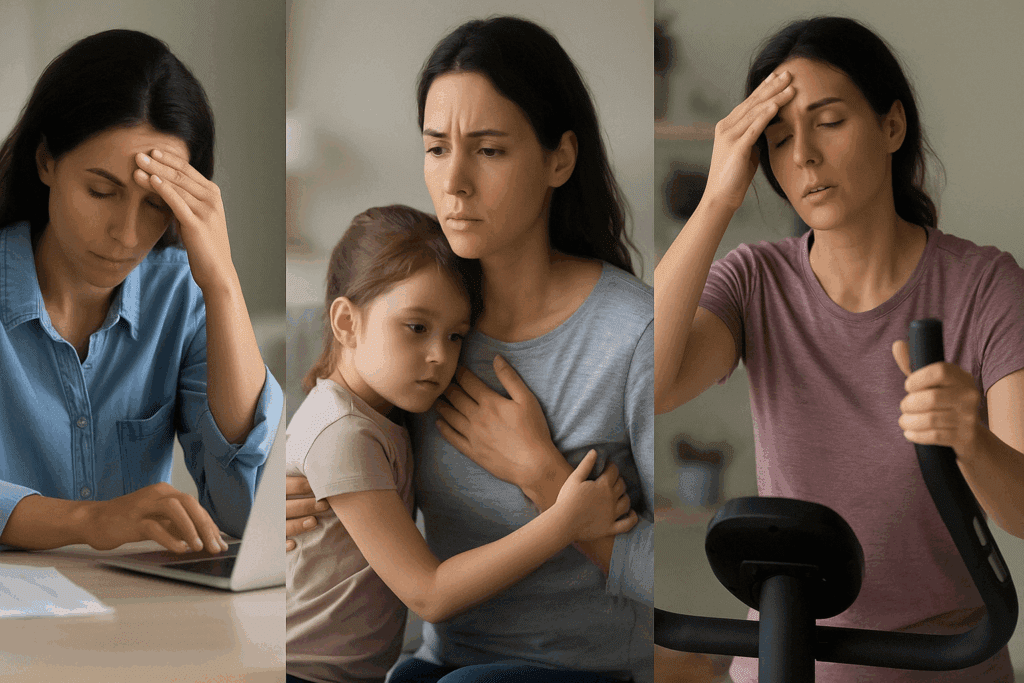
Unlike the classic textbook symptoms often described in men, high blood pressure in women frequently presents with subtler, less specific indicators. This difference in presentation can lead to delays in diagnosis and treatment, increasing the risk of serious complications. Women may experience fatigue, anxiety, dizziness, or palpitations—symptoms that are easily dismissed as hormonal or emotional in origin. This misattribution is not only perpetuated by societal norms but also by healthcare systems that historically underrepresent women in cardiovascular research.
The concept of high BP in women being a “silent killer” is particularly apt. Many women are unaware they have elevated blood pressure until they suffer a major event such as a heart attack or stroke. Even then, the presentation of these events may be atypical. For example, women are more likely to report nausea, shortness of breath, or back pain during a heart attack, rather than the crushing chest pain often experienced by men. These nontraditional symptoms further complicate timely recognition and response.
Compounding the issue is the prevalence of comorbid conditions that can mask or mimic the signs of hypertension. Anxiety disorders, thyroid dysfunction, and perimenopausal changes can all present with overlapping symptoms, making it difficult to discern the underlying cause without appropriate diagnostic testing. As such, clinicians must maintain a high index of suspicion and adopt a gender-sensitive approach when evaluating women for cardiovascular risk.
Another contributing factor is the belief among some women that they are less at risk for heart disease compared to men. This misconception, rooted in outdated medical narratives, can result in lower rates of routine screening and poor adherence to treatment recommendations. Public health campaigns and educational initiatives aimed at correcting these myths are essential to improving awareness and engagement.
Moreover, socioeconomic and cultural barriers can hinder access to care for many women. Those with limited financial resources, caregiving responsibilities, or language barriers may face challenges in prioritizing their own health. Addressing these disparities requires systemic changes in healthcare delivery, as well as community-based support and culturally competent education. Only by acknowledging and addressing these multifaceted obstacles can we hope to reduce the burden of undiagnosed and untreated female high blood pressure.

Understanding the Biological and Lifestyle Drivers of High Blood Pressure in Women
A comprehensive approach to managing high blood pressure in women begins with understanding the interplay between biological and lifestyle factors. While genetics and age are non-modifiable risks, there is substantial evidence that dietary habits, physical activity, stress management, and sleep quality all play pivotal roles in the development and progression of hypertension.
One of the most significant dietary contributors to high BP in women is excessive sodium intake. Processed and packaged foods are often laden with salt, and women may be more vulnerable to its hypertensive effects due to differences in hormonal regulation and renal sodium handling. In contrast, diets rich in potassium, magnesium, and calcium—such as those found in leafy greens, legumes, nuts, and dairy—have been shown to support optimal blood pressure levels. The Dietary Approaches to Stop Hypertension (DASH) diet is particularly effective in lowering blood pressure and is often recommended for women at risk.
Weight gain, especially around the abdominal area, is another critical risk factor. Postmenopausal women often experience a redistribution of fat, leading to increased central adiposity. This type of fat is metabolically active and associated with inflammation, insulin resistance, and vascular dysfunction—all of which can drive up blood pressure. Weight management through a combination of healthy eating, portion control, and regular exercise is thus essential in preventing and treating high blood pressure in women.
Chronic stress is another frequently overlooked driver of female high blood pressure. Women often juggle multiple roles—as professionals, caregivers, and household managers—which can contribute to long-term psychological strain. This persistent stress response activates the sympathetic nervous system, leading to elevated heart rate and vasoconstriction. Over time, this can result in sustained increases in blood pressure. Incorporating mindfulness practices, relaxation techniques, and supportive therapy can mitigate these effects and improve cardiovascular outcomes.
Sleep disorders, including insomnia and obstructive sleep apnea, are also emerging as important contributors to high BP in women. Hormonal fluctuations during menopause can disrupt sleep architecture, while conditions like sleep apnea are underdiagnosed in women due to differing symptom presentation. Ensuring adequate sleep hygiene and seeking treatment for sleep disturbances can significantly impact blood pressure control.
Lastly, substance use, including alcohol and tobacco, must not be overlooked. While smoking rates among women have declined, the cardiovascular risk remains significant even with minimal exposure. Alcohol consumption, particularly in excess, has a dose-dependent relationship with blood pressure. Tailored interventions that address these behaviors in a supportive, nonjudgmental manner are essential for long-term health improvement.

Evidence-Based Prevention and Treatment Strategies Tailored to Women
Given the unique risk factors and presentations of high BP in women, a one-size-fits-all approach to prevention and treatment is inadequate. Instead, interventions must be personalized and grounded in the latest evidence. This begins with regular blood pressure monitoring, ideally at home and during routine healthcare visits. Early identification of elevated readings allows for timely intervention and better outcomes.
Lifestyle modification remains the cornerstone of hypertension management. For women, this means incorporating heart-healthy dietary patterns, such as the DASH or Mediterranean diet, engaging in at least 150 minutes of moderate-intensity aerobic activity per week, and maintaining a healthy body weight. Resistance training, often underutilized by women, has also been shown to improve vascular health and reduce blood pressure.
Pharmacologic treatment should be tailored to the individual, taking into account comorbidities, reproductive status, and potential drug interactions. For example, some antihypertensive medications may not be suitable during pregnancy or may interfere with hormonal therapies. Clinicians should consider sex-specific responses to medication, as some studies suggest women may experience more side effects from certain drug classes. Shared decision-making and clear communication are key to optimizing adherence and effectiveness.
Behavioral counseling and psychological support can also enhance treatment adherence and address underlying contributors to hypertension. Women experiencing high stress, trauma, or mental health challenges may benefit from cognitive-behavioral therapy, peer support groups, or integrative approaches like yoga and meditation. These interventions can help regulate the autonomic nervous system and support blood pressure control.
Importantly, health education must be inclusive and accessible. Culturally sensitive materials, multilingual resources, and community outreach programs can help bridge knowledge gaps and empower women to take charge of their cardiovascular health. Telehealth and digital monitoring tools offer additional avenues for engagement, particularly for those with mobility or geographic constraints.

Empowering Women Through Awareness and Advocacy
One of the most powerful tools in addressing female high blood pressure is education. Women must be equipped with the knowledge and resources to understand their risk factors, recognize early warning signs, and advocate for their health. Healthcare providers, in turn, must remain vigilant, adopting a gender-specific lens in diagnosis and treatment.
National and international public health campaigns should prioritize female cardiovascular health, dispelling myths and encouraging proactive screening. Media representation also plays a critical role in shaping perceptions. When women see others like themselves speaking openly about heart health, it normalizes the conversation and promotes a culture of awareness.
Family history discussions, starting from a young age, can also be impactful. Encouraging intergenerational conversations about blood pressure, heart disease, and stroke risk can foster early prevention behaviors. School-based health programs, workplace wellness initiatives, and reproductive health visits are all strategic touchpoints for engaging women in meaningful dialogue.
Ultimately, the empowerment of women in health extends beyond individual behavior change. It involves systemic shifts in healthcare policy, research funding, and clinical training. Ensuring equitable access to care, improving representation in clinical trials, and educating providers on sex-based differences in disease are foundational to reducing the burden of high BP in women.
Frequently Asked Questions: Female High Blood Pressure
1. How does female high blood pressure affect mental health and emotional well-being?
High blood pressure can have a profound impact on a woman’s mental health, often compounding feelings of anxiety, irritability, or depression. While stress is widely recognized as a contributor to hypertension, the reverse is also true: chronic hypertension can alter brain chemistry and increase the risk for mood disorders. High BP in women is often underdiagnosed when emotional symptoms are prioritized over cardiovascular screening. Furthermore, the hormonal shifts associated with menopause or perimenopause can make women more vulnerable to mood changes, which may be mistakenly attributed to psychological causes when vascular issues are at play. Understanding this mind-body connection is essential for developing comprehensive treatment plans that support both cardiovascular and emotional resilience.
2. Are there unique challenges for managing high BP in women with caregiving responsibilities?
Yes, caregiving roles often place women under chronic emotional and logistical strain, which can complicate blood pressure management. Many women caring for children, aging parents, or ill spouses delay their own medical care, resulting in late diagnosis or poorly controlled hypertension. Additionally, sleep disruptions and lack of self-care routines common among caregivers may aggravate female high blood pressure. Integrating stress-reduction techniques and support systems tailored to caregivers can be a critical part of effective hypertension management. It’s important for healthcare providers to recognize these social dimensions when developing care plans for high BP women.
3. What are some emerging technologies helping women monitor their blood pressure more effectively at home?
Recent advances in wearable health tech are revolutionizing how high BP women can track their readings outside clinical settings. Devices such as smartwatches equipped with optical sensors and AI-powered blood pressure monitors offer real-time feedback, making it easier to identify triggers and patterns. For women with busy schedules or caregiving duties, these tools reduce the need for frequent in-office visits while providing consistent data. Moreover, newer platforms include telehealth integration, allowing for direct uploads to physician portals. This is especially beneficial for tracking female high blood pressure, which may fluctuate in response to hormonal cycles or life-stage transitions.
4. How can nutritional interventions be customized for women dealing with hypertension?
While general dietary recommendations like the DASH diet are beneficial, specific nutrient needs and food sensitivities should be considered when tailoring plans for female high blood pressure. For instance, postmenopausal women may need additional calcium and magnesium to support vascular tone and bone health simultaneously. Some high BP women may also be more salt-sensitive, necessitating closer scrutiny of sodium intake even in natural foods like dairy or seafood. Cultural preferences and hormonal cycles should also guide meal planning; for example, cravings and fluid retention may change throughout the menstrual cycle. A registered dietitian with experience in women’s cardiovascular health can help personalize strategies effectively.
5. Is there a link between high blood pressure and menstrual health in women?
Emerging research suggests that irregular or painful menstruation may be associated with a higher risk of developing hypertension later in life. While causality has not been firmly established, inflammation and hormonal imbalances related to cycle irregularities may play a role in vascular dysfunction. High BP in women who also experience conditions like polycystic ovary syndrome (PCOS) or endometriosis may require more aggressive monitoring. Understanding menstrual patterns can offer early clues into potential cardiovascular issues. Women tracking their cycle should also monitor changes in blood pressure, particularly if symptoms like headaches or fatigue are more pronounced during certain phases.
6. How do societal norms influence awareness and treatment of high BP in women?
Societal expectations that position women as primary caregivers and emotional anchors often lead them to deprioritize their own health. Consequently, female high blood pressure may go unnoticed or be attributed to stress rather than a medical condition requiring attention. Some women may also internalize discomfort or dismiss early symptoms due to cultural norms around endurance and self-sacrifice. These dynamics contribute to a delay in seeking care and lower adherence to treatment plans. Public health efforts must work to dismantle these norms and empower women to advocate for timely screening and consistent management.
7. Can yoga and mind-body practices significantly impact blood pressure in women?
Yes, yoga and other mind-body modalities such as tai chi and meditation have shown measurable benefits in reducing systolic and diastolic pressure, particularly in high BP women experiencing chronic stress. These practices engage the parasympathetic nervous system, encouraging relaxation and improved heart rate variability. For female high blood pressure, which is often linked to stress and hormonal fluctuations, such interventions offer a low-cost, accessible adjunct to medical therapy. Studies also suggest that consistency is key—women who practice these methods regularly over months experience more pronounced improvements. Beyond physical benefits, these practices enhance emotional well-being and improve adherence to lifestyle changes.
8. How does menopause uniquely alter hypertension risk and management in women?
Menopause marks a pivotal shift in cardiovascular health, as the decline in estrogen is directly linked to increased arterial stiffness and reduced endothelial function. Female high blood pressure often emerges or worsens during this period due to both physiological changes and lifestyle adjustments, such as weight gain or altered sleep patterns. Hormone replacement therapy (HRT) remains a controversial but potentially useful tool for some women, although it must be carefully weighed against cardiovascular risks. Some antihypertensive drugs may also interact differently in postmenopausal women, necessitating dosage adjustments. An integrative approach that includes dietary, pharmaceutical, and hormonal considerations is often the most effective strategy.
9. What role does sleep architecture play in high blood pressure among women?
Sleep disturbances, including insomnia and obstructive sleep apnea, are disproportionately underdiagnosed in women, even though they can significantly elevate blood pressure over time. Hormonal changes, especially during perimenopause, often contribute to sleep fragmentation and reduced restorative sleep. Female high blood pressure is more likely to persist when sleep quality is compromised, regardless of other lifestyle factors. Screening for sleep disorders should be a routine part of hypertension evaluation in women, especially those who report fatigue, snoring, or mood changes. Behavioral sleep therapy and, where necessary, CPAP therapy can offer significant improvements in both sleep and cardiovascular metrics.
10. How can women approach conversations with their doctors about hypertension more effectively?
Many women feel dismissed or misunderstood when discussing symptoms that could indicate high blood pressure. Preparing a log of home blood pressure readings, noting associated symptoms and lifestyle triggers, can help structure a more productive dialogue. It’s also valuable for high BP women to ask specific questions about how hormonal status, reproductive history, and current medications may influence their condition. Seeking out clinicians with experience in women’s cardiovascular health or requesting referrals to specialists can further enhance care quality. Ultimately, assertiveness and preparation empower women to become proactive partners in managing female high blood pressure.
Confronting Female High Blood Pressure: A Call to Action for Prevention and Lifelong Wellness
High blood pressure in women is a complex and multifaceted condition that demands our urgent attention. It is shaped by a constellation of hormonal, lifestyle, genetic, and social factors that interact in ways unique to the female body and experience. Yet, too often, the signs are missed, the risks underestimated, and the treatments generalized. By acknowledging the specific dynamics of high BP in women and embracing a tailored, evidence-based approach to care, we can transform outcomes and reduce the toll of cardiovascular disease.
From adolescence through menopause and beyond, every stage of a woman’s life presents both challenges and opportunities for prevention. By raising awareness, encouraging proactive health monitoring, and promoting gender-sensitive medical practices, we empower women to take control of their cardiovascular destiny. The road to better heart health begins with knowledge—and it is through this lens of understanding and advocacy that meaningful change can occur.
As research continues to evolve, so too must our approach to healthcare. Integrating insights from endocrinology, behavioral science, public health, and cardiology will enable us to provide comprehensive, compassionate, and effective care for women at every life stage. In doing so, we not only improve individual lives but also elevate the health of entire communities. The time to act is now, and the future of women’s cardiovascular health depends on it.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
High Blood Pressure and Heart Disease in Women
Hypertension in women: latest findings and clinical implications
Hypertension in Females: Understanding Its Impact on Women’s Health