High blood pressure, often associated with adults, is increasingly being recognized as a significant concern in children and adolescents. While it might not always receive the same attention as adult hypertension, elevated blood pressure in young individuals can lead to serious health complications if left unaddressed. For parents, caregivers, and healthcare providers, understanding the signs, causes, and management of high blood pressure in kids is crucial for supporting lifelong cardiovascular health.
In recent decades, growing awareness and improvements in pediatric screening practices have led to more frequent diagnoses of childhood hypertension. This condition, once thought to be rare in young populations, is now acknowledged as both a standalone health issue and a marker of potential underlying problems such as obesity, kidney disease, or congenital heart defects. Early intervention can be pivotal in preventing complications later in life, such as stroke, heart attack, or chronic kidney disease. As such, gaining clarity around what constitutes normal blood pressure for children of various ages and identifying risk factors early on can empower parents and health professionals to take proactive steps toward prevention and treatment.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Understanding Normal Blood Pressure in Children
Blood pressure norms vary significantly based on age, height, and gender. For young children, such as those around the age of four or five, what constitutes a “normal” reading may differ from what would be expected in teens or adults. It is essential to interpret pediatric blood pressure values using percentile charts, which take into account a child’s growth metrics. A normal blood pressure for a 5-year-old, for instance, typically ranges around 95/55 to 110/70 mmHg, depending on their size and overall health. For a 4-year-old, blood pressure values often fall within a similar range, though slightly lower values may still be considered healthy.
When discussing 4 year old blood pressure and normal blood pressure for 4 year old readings, one must remember that fluctuations can occur due to stress, physical activity, or even the environment in which the measurement is taken. This means a single elevated reading doesn’t necessarily indicate a problem. Repeated measurements and a consistent pattern of elevated values are needed before a diagnosis of hypertension can be confirmed. Pediatricians use detailed percentile curves to determine whether a child’s blood pressure falls into the normal, elevated, or hypertensive category, thereby tailoring their assessment to each individual child.
Similarly, in evaluating normal blood pressure for a 5 year old, healthcare professionals often look at both the systolic (top number) and diastolic (bottom number) pressures in relation to standardized age-specific norms. A reading consistently above the 90th percentile may indicate elevated blood pressure, while those above the 95th percentile may be classified as hypertensive. These distinctions are not just academic—they guide treatment decisions and inform whether lifestyle changes or further testing is required.
Risk Factors and Causes of High Blood Pressure in Kids
Childhood hypertension can be categorized as either primary (essential) or secondary. Primary hypertension is more common in older children and teens and is often linked to lifestyle factors such as obesity, physical inactivity, poor diet, or a family history of high blood pressure. In contrast, secondary hypertension is more frequently seen in younger children and is usually the result of an underlying medical condition, such as kidney disease, congenital heart defects, or hormonal disorders.
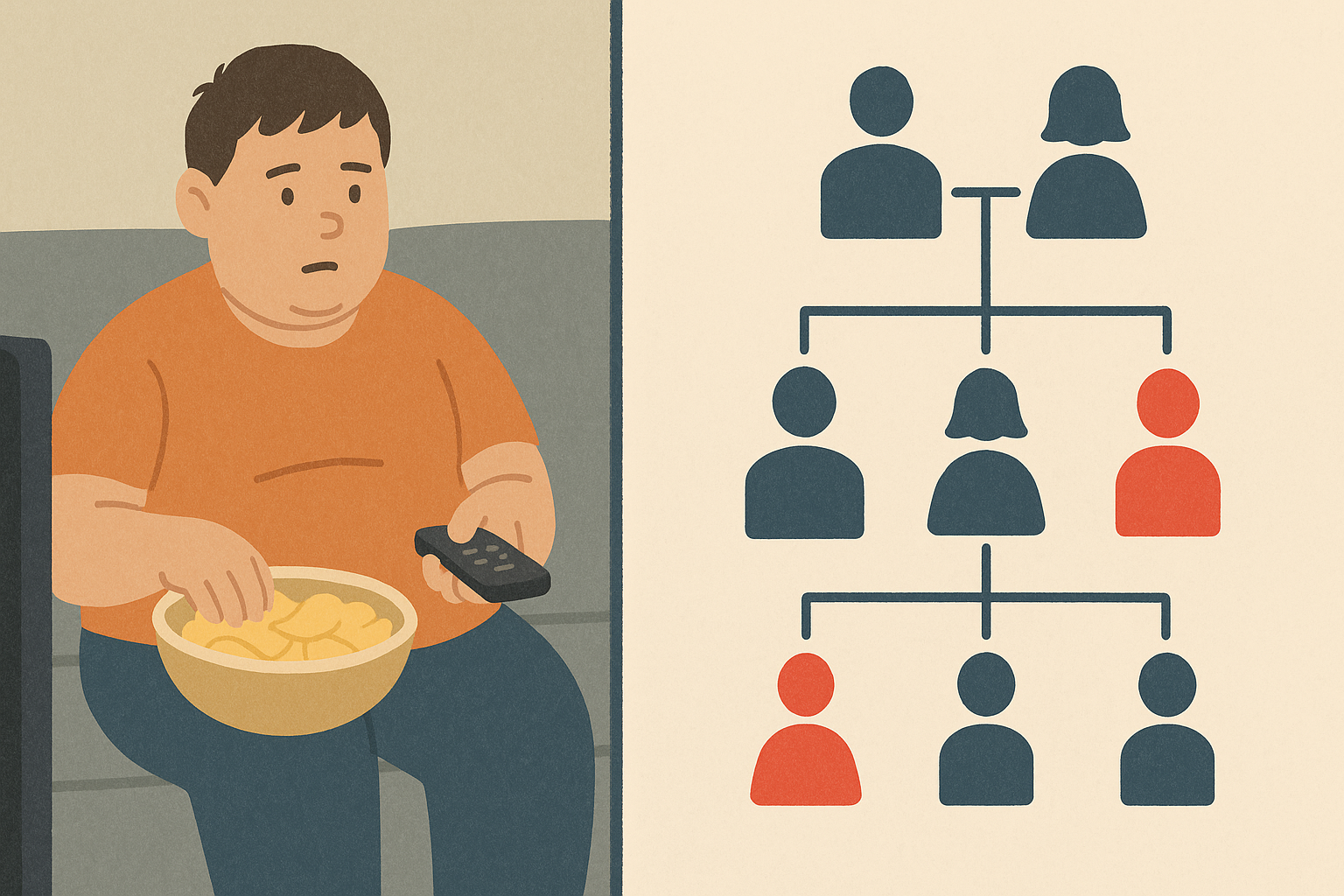
One of the most prevalent contributors to high blood pressure in kids is excess body weight. As rates of childhood obesity continue to climb, so does the incidence of high blood pressure. Fat tissue contributes to increased vascular resistance and alters the balance of hormones that regulate blood pressure. When these physiological changes are coupled with sedentary behavior and high sodium intake, the result can be persistently elevated blood pressure.
Additionally, genetic predisposition plays a notable role in the development of childhood hypertension. If a child has one or both parents with high blood pressure, they are significantly more likely to develop the condition themselves. This hereditary factor, combined with shared environmental and dietary habits, can amplify risk. Other potential contributors include sleep apnea, exposure to tobacco smoke, stress, and certain medications, such as corticosteroids or stimulants used to treat ADHD.
Recognizing High Blood Pressure in Teens
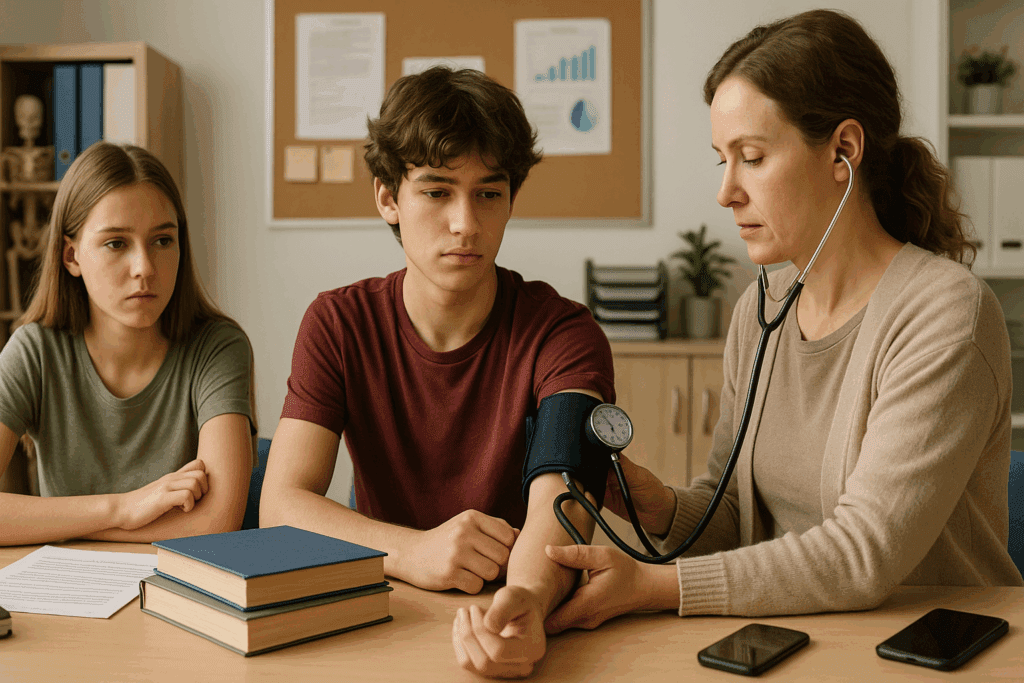
High blood pressure in teens is becoming increasingly prevalent, often paralleling the rise in adolescent obesity and sedentary lifestyles. It is crucial for parents and guardians to understand what constitutes normal bp for a teenager, which generally hovers around 110/70 to 120/80 mmHg, though, again, individual factors like height and weight must be taken into account. Blood pressure for teens that consistently exceeds the 90th percentile based on age, sex, and height should prompt further evaluation.
Hypertension in teens may go unnoticed because it often lacks obvious symptoms. Unlike adults, who might experience headaches, dizziness, or chest pain, many teenagers with elevated blood pressure are asymptomatic. This makes regular health check-ups all the more important, especially during adolescence when hormonal changes and lifestyle habits can significantly impact cardiovascular health. Annual physicals should include routine blood pressure measurements to detect changes early.
High blood pressure as a teenager may also be a reflection of poor dietary habits, such as excessive consumption of processed foods, sugary drinks, and high-sodium snacks. Additionally, academic pressures, mental health challenges, and inadequate sleep can all contribute to the condition. Because adolescence is a critical period for developing long-term health behaviors, identifying and addressing elevated blood pressure during these years can have profound implications for future well-being.
Diagnosing and Monitoring Childhood Hypertension
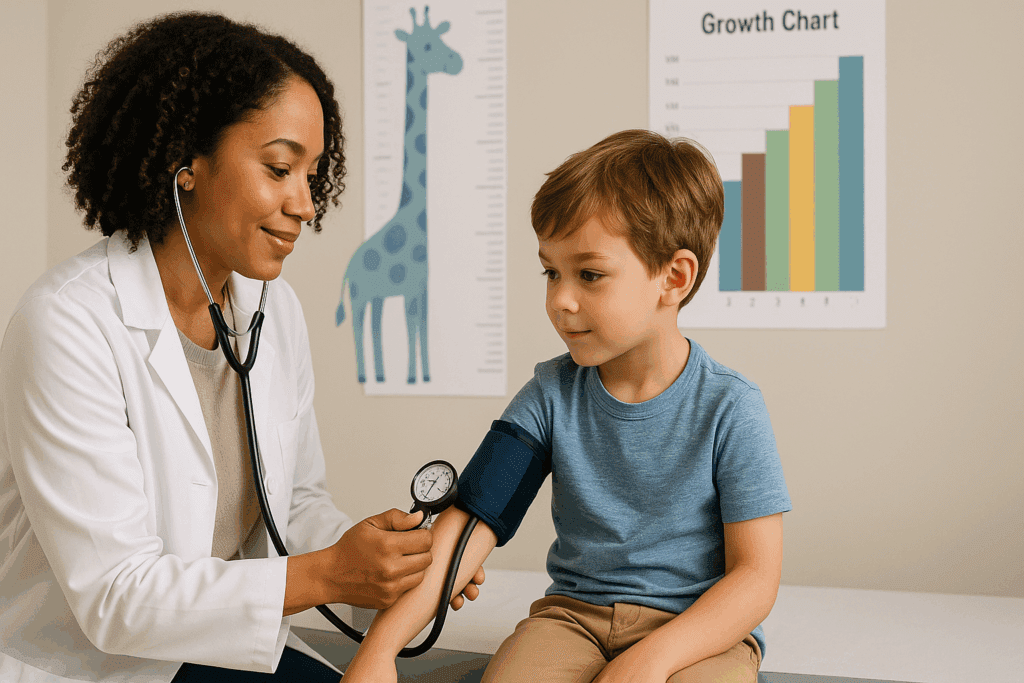
The diagnosis of high blood pressure in kids involves more than just a single elevated reading. Proper technique and consistency are vital for accuracy. Blood pressure should be measured using the correct cuff size, and the child should be calm and seated for at least five minutes before the reading. Ideally, multiple readings should be taken on separate occasions to confirm the diagnosis. Ambulatory blood pressure monitoring, which involves tracking blood pressure over 24 hours while the child goes about their normal activities, is sometimes used to rule out white-coat hypertension—an anxiety-induced elevation that occurs only in clinical settings.
In diagnosing childhood hypertension, pediatricians rely on standardized blood pressure tables based on age, height, and gender percentiles. These tables help clinicians determine whether a reading falls within the normal range or crosses into elevated or hypertensive territory. When a pattern of high readings is observed, additional assessments may be conducted to explore potential causes. These could include blood tests, urinalysis, imaging studies such as renal ultrasounds, and evaluations for endocrine or cardiovascular abnormalities.
Once a diagnosis is made, ongoing monitoring is essential. Children with hypertension may require frequent blood pressure checks, lifestyle counseling, and in some cases, pharmacological treatment. Close follow-up ensures that interventions are effective and helps to prevent complications. It also provides an opportunity to educate families about the importance of long-term cardiovascular health and the steps they can take to support it.

Lifestyle Changes and Treatment Approaches
Lifestyle modification is the cornerstone of treatment for most children with elevated blood pressure, particularly in cases of primary hypertension. Dietary adjustments, physical activity, weight management, and stress reduction can all contribute to meaningful improvements. The Dietary Approaches to Stop Hypertension (DASH) diet, which emphasizes fruits, vegetables, whole grains, and low-fat dairy products while limiting sodium, is frequently recommended for managing blood pressure in both children and adults.
Encouraging regular physical activity is another key strategy. The American Academy of Pediatrics advises that children and adolescents engage in at least 60 minutes of moderate to vigorous physical activity most days of the week. This could include sports, biking, swimming, or even active play. Limiting screen time and promoting outdoor activities can help reduce sedentary behavior and improve overall cardiovascular fitness.
In cases where lifestyle modifications are insufficient or the child has secondary hypertension, medication may be prescribed. Common classes of antihypertensive drugs used in pediatric populations include ACE inhibitors, angiotensin receptor blockers (ARBs), calcium channel blockers, and diuretics. The choice of medication depends on the underlying cause, severity of hypertension, and presence of coexisting conditions. Treatment is often started at a low dose and adjusted as needed, with careful monitoring for side effects and efficacy.
The Long-Term Impact of Untreated Pediatric Hypertension
The implications of untreated high blood pressure in kids extend far beyond childhood. Elevated blood pressure during the early years of life has been associated with structural changes in the heart, such as left ventricular hypertrophy, which can lead to long-term cardiac dysfunction. Additionally, hypertension in teens and younger children can predispose them to atherosclerosis, chronic kidney disease, and metabolic syndrome later in life.
Research shows that children with persistently high blood pressure are more likely to become hypertensive adults, particularly if other risk factors such as obesity or a sedentary lifestyle persist. This continuity underscores the importance of early detection and intervention. Managing blood pressure during childhood is not just about preventing immediate symptoms—it is a critical step in reducing the burden of cardiovascular disease across the lifespan.
Moreover, the psychological effects of chronic illness in childhood should not be overlooked. Repeated medical visits, dietary restrictions, and the need for daily medications can impact a child’s self-esteem and social development. Comprehensive care should therefore include support for emotional and mental health, with resources such as counseling and peer support groups made available when needed.
Educating Families and Promoting Preventive Care
Effective management of childhood hypertension requires active involvement from families. Education is key—parents must understand what normal blood pressure for 5 year old or normal bp for 4 year old means in practical terms. They should know how to interpret readings, recognize potential warning signs, and implement lifestyle changes at home. Simple steps such as preparing low-sodium meals, encouraging active play, and modeling healthy behavior can make a significant difference.
Healthcare providers play a critical role in guiding families through the diagnostic and treatment process. Well-child visits offer an ideal opportunity to discuss blood pressure, growth patterns, nutrition, and activity levels. In cases where high blood pressure in kids is identified, providers should offer clear explanations and collaborative care plans that empower families to take ownership of their child’s health.
School systems and community programs can also support preventive efforts by promoting physical education, providing healthy meal options, and raising awareness about childhood hypertension. Public health campaigns that highlight the importance of regular screenings and early intervention can help shift the perception of hypertension from an adult-only concern to a whole-family issue.
Looking Ahead: The Future of Pediatric Blood Pressure Management
As our understanding of childhood hypertension evolves, so too does the approach to its management. Advances in wearable technology and home monitoring devices now allow families to track blood pressure readings in real time, enabling earlier detection and more responsive care. These tools can also help children become more engaged in their own health, fostering a sense of agency that can last into adulthood.
Future research is exploring the genetic and epigenetic factors that contribute to blood pressure regulation in children, which could lead to more personalized treatment strategies. Scientists are also investigating the long-term effects of early-life exposures—such as prenatal nutrition, environmental toxins, and stress—on cardiovascular risk, paving the way for preventive interventions even before birth.
Ultimately, the goal is to create a healthcare environment where pediatric hypertension is recognized, addressed, and managed with the same urgency as other chronic conditions. By continuing to refine our screening tools, treatment options, and public health strategies, we can help ensure that today’s children grow into heart-healthy adults.
Frequently Asked Questions: Childhood Hypertension and Pediatric Blood Pressure
What can cause sudden spikes in kids’ blood pressure, even if they’re otherwise healthy?
Sudden spikes in kids’ blood pressure can be caused by acute stress, dehydration, pain, or even certain over-the-counter medications such as decongestants. Children may also experience transient elevations due to anxiety during medical appointments, commonly known as “white coat syndrome.” In some cases, hidden dietary triggers like excessive caffeine from energy drinks or high sodium intake from processed snacks can also play a role. It’s important to contextualize these spikes within the broader pattern of a child’s cardiovascular health rather than rely on isolated readings. When evaluating kids blood pressure trends, ongoing monitoring and keeping a blood pressure diary can help distinguish between temporary fluctuations and true underlying hypertension.
How does physical activity influence normal blood pressure for a 5 year old and what exercises are best?
Regular physical activity plays a crucial role in regulating blood pressure, even for young children. For a normal blood pressure for 5 year old children, incorporating daily movement like dancing, biking, swimming, or unstructured outdoor play helps maintain vascular health. These activities improve endothelial function, enhance blood flow, and encourage the heart to pump more efficiently. Avoiding a sedentary lifestyle is essential, especially as early cardiovascular patterns often continue into adolescence and adulthood. Parents should be aware that promoting consistent, joyful movement can be one of the most effective long-term strategies to maintain healthy kids blood pressure and prevent the early onset of chronic conditions.
Why do some children with normal body weight still develop childhood hypertension?
Although obesity is a well-known risk factor, some children with average or even below-average weight can still develop childhood hypertension due to genetic predisposition, kidney disorders, hormonal imbalances, or structural heart anomalies. A family history of high blood pressure in kids increases the likelihood, especially if both parents are affected. In these cases, the underlying cause may not be lifestyle-related but rooted in renal or endocrine dysfunction. Routine screening is still essential for children who appear healthy but have known risk factors. Monitoring normal bp for 4 year old children or others within the same age group ensures that even those without outward symptoms receive timely diagnosis and care.
Is high blood pressure in teens more likely to affect boys or girls?
The prevalence of high blood pressure in teens tends to vary by gender, especially during puberty. Boys are slightly more prone to developing hypertension in teens, particularly due to hormonal changes, greater lean muscle mass, and lifestyle behaviors such as higher sodium consumption or lower levels of physical activity. However, girls are not exempt—certain conditions such as polycystic ovary syndrome (PCOS) and hormonal contraceptive use may elevate risk. Lifestyle stressors like academic pressure or social dynamics can affect both genders differently, contributing to fluctuating blood pressure for teens. Therefore, it’s crucial to screen both boys and girls regularly, regardless of visible symptoms or body composition.
How can schools help reduce the risk of high blood pressure in kids?
Schools play a pivotal role in shaping children’s long-term health behaviors. Implementing nutritious meal programs, integrating frequent physical education, and fostering mindfulness or stress-relief techniques can contribute meaningfully to reducing high blood pressure in kids. By creating environments that promote whole-child wellness—addressing nutrition, movement, and mental health—schools can be powerful allies in combating childhood hypertension. Even small changes, such as replacing vending machine snacks with healthier options or offering brief movement breaks during class, can support normal bp for a teenager and reduce sedentary behaviors. Collaborative efforts between educators, parents, and healthcare providers create the strongest foundation for prevention.
What are the psychological effects of being diagnosed with hypertension in teens?
Receiving a diagnosis of hypertension in teens can trigger anxiety, self-consciousness, or a sense of isolation, especially if lifestyle changes or medications are required. Adolescents are often sensitive to anything that makes them feel different from their peers, and chronic health conditions can carry a social stigma. This emotional impact can, paradoxically, worsen blood pressure if stress levels are not managed effectively. Helping teens understand that managing their health is a strength rather than a weakness is key to building resilience. Offering support groups or counseling alongside education about normal bp for a teenager can help normalize their experience and reinforce positive self-image.
Are there technological tools parents can use to monitor 4 year old blood pressure at home?
Yes, several pediatric-specific digital blood pressure monitors are now available that make it easier for parents to track their child’s cardiovascular health at home. These tools are designed with smaller cuff sizes and child-friendly interfaces, allowing accurate and non-intimidating measurements. Tracking normal blood pressure for 4 year old children consistently at home can help identify trends that may not be obvious during annual checkups. Some models sync with apps to provide graphs and alerts, facilitating more informed discussions with healthcare providers. As these tools evolve, they may become indispensable in the early identification of childhood hypertension, particularly in families with known genetic risks.
How does poor sleep affect blood pressure for teens and younger children?
Sleep quality and duration are often overlooked factors in cardiovascular health, especially in pediatric populations. Inadequate sleep disrupts hormonal balance, increases sympathetic nervous system activity, and can elevate both systolic and diastolic pressures. Teens who sleep fewer than seven hours per night are particularly at risk, as this habit is often paired with increased screen time and high-stress academic routines. Similarly, disrupted sleep in young children—especially those with sleep apnea or inconsistent routines—can interfere with maintaining a normal bp for 4 year old or 5-year-old kids. Encouraging age-appropriate sleep hygiene is a practical, evidence-based intervention that supports blood pressure regulation.
Is dietary salt always harmful for kids, or does it depend on the child?
While high sodium intake is widely recognized as a risk factor for elevated blood pressure, its impact can vary depending on the child’s overall health and genetic background. Some children are salt-sensitive, meaning their blood pressure responds more strongly to dietary sodium, even at moderate levels. For others, especially those who are physically active and eat otherwise balanced meals, occasional indulgence may have less of an impact. Monitoring normal blood pressure for 5 year old children in the context of their full dietary pattern provides a more accurate picture than focusing on one nutrient alone. Parents should prioritize whole, minimally processed foods while being mindful of hidden sodium in items like bread, deli meats, and packaged snacks.
What are future directions in research for treating high blood pressure in kids?
Current research is exploring the use of genetics, machine learning, and microbiome analysis to better understand and treat high blood pressure in kids. Scientists are investigating how gut bacteria may influence vascular function, and how personalized nutrition plans could eventually be tailored to a child’s genetic profile. Artificial intelligence tools are also being developed to analyze vast datasets and predict which children are most at risk of childhood hypertension before symptoms appear. These innovations promise more precise, individualized care that could go beyond today’s one-size-fits-all approach. As these technologies become mainstream, they may redefine how we diagnose and manage everything from 4 year old blood pressure concerns to chronic hypertension in teens.
A Lifelong Commitment to Cardiovascular Health Begins in Childhood
Recognizing and managing high blood pressure in kids is a critical part of supporting lifelong heart health. Whether it’s understanding what constitutes normal bp for a teenager or monitoring 4 year old blood pressure trends, early attention to these factors can prevent serious complications down the road. As childhood hypertension becomes increasingly prevalent, it’s vital that parents, educators, healthcare providers, and policymakers work together to promote awareness, encourage preventive practices, and ensure access to appropriate care.
Normal blood pressure for 4 year old children, like that for older kids and teens, must be contextualized within a child’s overall health profile. The same holds true for interpreting blood pressure for teens or assessing whether high blood pressure as a teenager is a temporary issue or a sign of an ongoing condition. In all cases, the earlier a problem is detected and addressed, the better the outcome is likely to be.
With the right combination of education, lifestyle support, medical intervention, and community engagement, childhood hypertension can be managed effectively. More importantly, these efforts lay the foundation for a healthier adult population—one that is better equipped to navigate the challenges of chronic disease and embrace a future of well-being and vitality.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
High Blood Pressure in Children
High blood pressure in children
Patient education: High blood pressure in children (Beyond the Basics)