The cardiovascular system is the body’s intricate highway of blood vessels and the heart, tirelessly working to sustain life by delivering oxygen and nutrients throughout the body. One of the most accessible and essential indicators of cardiovascular health is the combination of blood pressure and pulse. Though these vital signs are routinely measured in clinical settings, their deeper implications often go unrecognized by the general public. Understanding normal blood pressure and pulse, along with the meaning of BP vitals and insights from a pulse pressure chart, can provide invaluable clues about a person’s heart health and overall physiological balance. This article explores these indicators in depth, decoding their meanings, their roles in preventive health, and how they reflect the dynamic equilibrium of the human body.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention

Decoding the Basics: What Are Blood Pressure and Pulse?
To understand what constitutes normal blood pressure and pulse, we must first define the terms and their physiological foundations. Blood pressure refers to the force exerted by circulating blood on the walls of blood vessels, measured in millimeters of mercury (mm Hg). It consists of two values: systolic pressure (the top number), representing the force during heartbeats, and diastolic pressure (the bottom number), reflecting the force when the heart rests between beats. A typical normal reading is around 120/80 mm Hg, though optimal ranges can vary slightly depending on individual health factors and age.
Pulse, on the other hand, measures the number of heartbeats per minute and is commonly felt at the wrist or neck. A normal resting pulse typically ranges from 60 to 100 beats per minute for adults, though well-conditioned athletes may have a lower resting pulse due to more efficient heart function. Together, blood pressure and pulse form part of what are often referred to as BP vitals, meaning essential measurements that provide a snapshot of cardiovascular status and overall health. These vitals are crucial not only for diagnosing acute conditions like hypertensive crises or arrhythmias but also for understanding long-term cardiovascular risk.
Why Monitoring BP Vitals Meaningfully Impacts Health Outcomes
Monitoring blood pressure and pulse provides more than just numbers on a chart—it offers real-time insights into how the heart and vessels respond to internal and external stimuli. The BP vitals meaning lies in their capacity to detect abnormalities early, sometimes before symptoms arise. For instance, elevated systolic or diastolic pressures may indicate underlying issues such as kidney disease, arterial stiffness, or excessive sympathetic nervous system activity. Conversely, an unusually low pulse could suggest bradycardia, which in some cases may be benign, but in others, may require medical intervention.
The interpretive value of these vitals is heightened when measured consistently and contextualized within a patient’s overall health profile. Chronic deviations from normal blood pressure and pulse readings are associated with increased risks for stroke, heart attack, and cognitive decline. Even moderate, sustained elevations can cause long-term damage to blood vessels and vital organs. That’s why physicians often emphasize routine monitoring, especially for individuals with comorbidities such as diabetes, obesity, or a family history of cardiovascular disease. The strategic use of home monitoring devices, when used correctly, empowers individuals to take charge of their health and identify troubling trends before they escalate into more serious conditions.
Exploring the Clinical Importance of the Pulse Pressure Chart
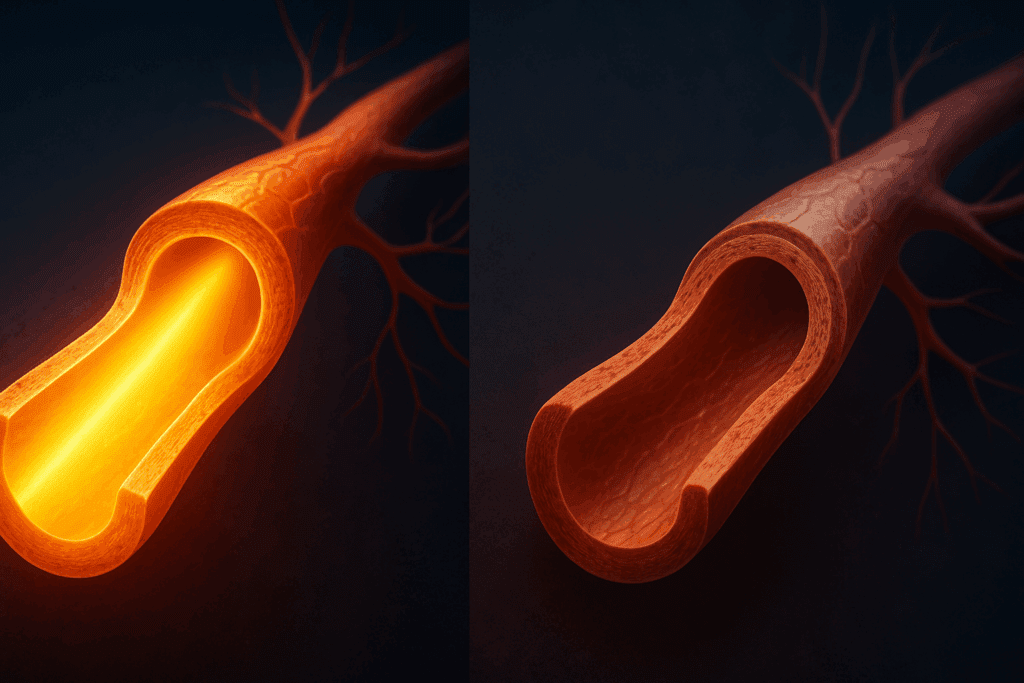
One of the less commonly understood, yet clinically significant, metrics derived from blood pressure readings is pulse pressure—the difference between systolic and diastolic values. A pulse pressure chart is used by clinicians to assess whether the differential is within a healthy range. A normal pulse pressure typically falls between 40 and 60 mm Hg. Values outside this range can signal potential cardiovascular problems. For example, a widened pulse pressure (e.g., 160/70) might indicate stiff arteries, which are often a precursor to cardiovascular disease in older adults. Conversely, a narrow pulse pressure (e.g., 90/70) may point to reduced stroke volume, which could result from conditions like heart failure or shock.
Understanding the implications of a pulse pressure chart is essential for those managing hypertension or heart disease. The chart enables healthcare providers to discern subtle shifts in cardiovascular function that might be missed when focusing solely on systolic and diastolic numbers. It adds nuance to BP vitals, meaning it contributes an extra dimension to our assessment of heart health. Additionally, researchers have found that elevated pulse pressure may be a stronger predictor of certain cardiac events than either systolic or diastolic pressure alone. This finding underscores the importance of incorporating pulse pressure into routine cardiovascular evaluations.

Factors That Influence Normal Blood Pressure and Pulse
Numerous variables affect what is considered normal blood pressure and pulse. Age is one of the most significant. As individuals age, arteries naturally lose some of their elasticity, which can result in higher systolic readings. Consequently, what may be considered elevated blood pressure in a young adult might be within the acceptable range for an older adult, depending on the context. Gender can also play a role, with some studies suggesting that premenopausal women tend to have lower blood pressure compared to men of the same age, although this trend can reverse after menopause due to hormonal changes.
Lifestyle choices also have a profound effect. Physical activity, stress levels, diet, alcohol consumption, and tobacco use all influence blood pressure and heart rate. Regular aerobic exercise, for example, often leads to lower resting pulse and improved blood pressure control. In contrast, chronic stress or high sodium intake can elevate both metrics. Medical conditions, including thyroid disorders, anemia, and sleep apnea, also influence BP vitals, meaning that deviations from normal values are not always linked directly to cardiovascular pathology. Comprehensive evaluation is required to determine the underlying causes of abnormal readings, reinforcing the need for personalized medical guidance.
Interpreting Trends in BP Vitals: What Fluctuations Can Tell You
While single measurements can be informative, tracking trends in blood pressure and pulse over time yields a more comprehensive picture of cardiovascular health. Occasional fluctuations are expected and usually not cause for concern. Stress, caffeine, medications, and even time of day can temporarily influence readings. However, persistent elevations or declines may warrant further investigation. For example, consistently elevated morning blood pressure has been associated with an increased risk of stroke, while nocturnal hypertension may indicate the presence of underlying disease.
A person who sees a gradual increase in pulse pressure over months or years might be experiencing early signs of arterial stiffness. Similarly, repeated observations of a heart rate consistently above 100 beats per minute, even at rest, could suggest an overactive thyroid or an arrhythmia like atrial fibrillation. Interpreting these trends within the framework of a pulse pressure chart helps clinicians contextualize readings and recommend appropriate interventions. By recognizing patterns early, interventions such as medication adjustment, lifestyle changes, or additional diagnostic testing can be initiated promptly.

How to Maintain Healthy BP Vitals Naturally
Maintaining normal blood pressure and pulse does not always require pharmacological intervention. Many individuals can preserve or restore healthy BP vitals through lifestyle modifications. Nutrition plays a central role. Diets rich in fruits, vegetables, whole grains, and lean proteins—such as the DASH (Dietary Approaches to Stop Hypertension) diet—have been shown to significantly reduce blood pressure. Limiting sodium intake, increasing potassium through natural food sources like bananas and leafy greens, and avoiding excessive alcohol can also support cardiovascular function.
Regular physical activity is another cornerstone. Engaging in at least 150 minutes of moderate aerobic exercise per week can help lower both systolic and diastolic pressures and promote a more efficient heart rate. Stress management is equally vital. Chronic stress activates the sympathetic nervous system, leading to sustained elevations in both blood pressure and pulse. Mindfulness practices, such as meditation, yoga, and deep breathing exercises, have demonstrated measurable benefits in lowering cardiovascular stress markers. When lifestyle adjustments are combined and sustained, they can significantly impact BP vitals, meaning that patients often find themselves needing fewer medications or avoiding them altogether.
Medical Interventions and When They Are Necessary
Despite best efforts at prevention, many individuals will eventually require medical intervention to manage their blood pressure or heart rate. Antihypertensive medications, including ACE inhibitors, beta-blockers, calcium channel blockers, and diuretics, are frequently prescribed depending on the specific nature and cause of hypertension. Heart rate abnormalities may necessitate medications like beta-blockers or antiarrhythmic drugs, or in some cases, the use of pacemakers.
The decision to initiate medical therapy is based not only on blood pressure readings but also on other risk factors, including age, cholesterol levels, smoking status, and the presence of diabetes or kidney disease. Physicians often use pulse pressure as an additional risk stratification tool, especially when assessing older adults. A patient with seemingly controlled systolic and diastolic pressures but a widening pulse pressure might still be at risk and benefit from further medical evaluation or treatment. Thus, the pulse pressure chart is not simply an academic tool—it informs real-world treatment decisions that can alter the trajectory of a patient’s health.
The Future of Cardiovascular Monitoring: From Wearables to AI
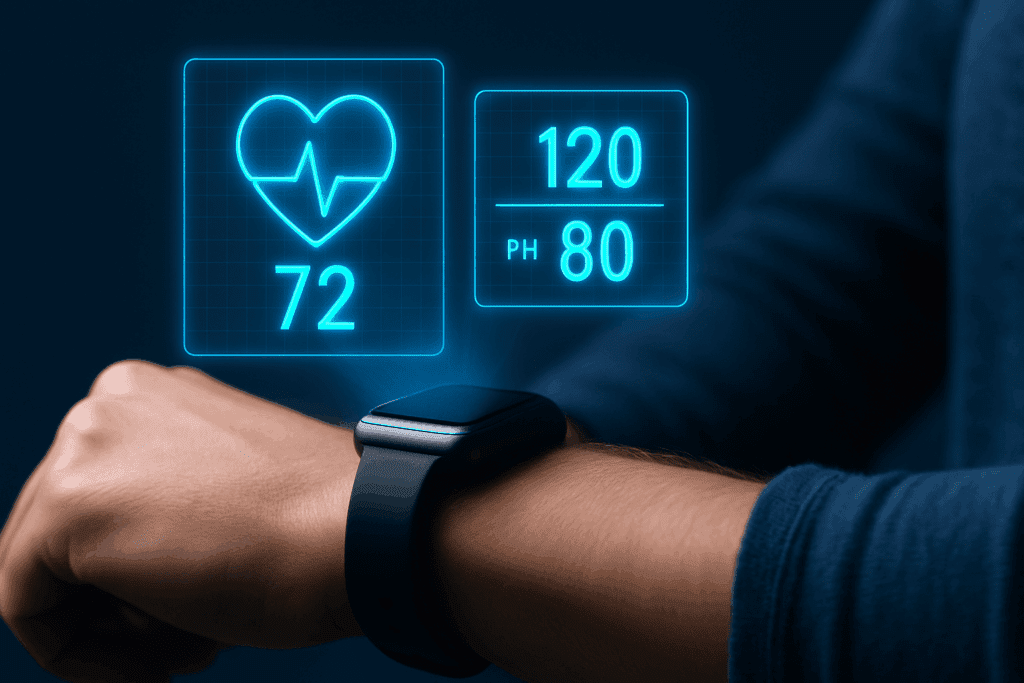
Advancements in digital health technology have revolutionized how we monitor and interpret blood pressure and pulse. Wearable devices, such as smartwatches and fitness trackers, now offer continuous heart rate monitoring and, in some models, blood pressure estimation. These tools provide users with valuable data that can reveal patterns and prompt timely medical consultations. The future likely holds even greater integration of artificial intelligence to analyze these data streams, offering predictive analytics that could forecast hypertension risk or detect arrhythmias before they become symptomatic.
These innovations complement traditional methods rather than replace them. While convenient, consumer-grade devices may lack the precision of clinical tools, making professional interpretation still essential. Nonetheless, the trend toward greater personal engagement with BP vitals reflects a broader shift in healthcare—one that values proactive, data-driven, and individualized care. As patients become more informed and equipped, their ability to maintain normal blood pressure and pulse will likely improve, leading to better outcomes and reduced healthcare costs.
Frequently Asked Questions: Understanding Blood Pressure, Pulse, and Cardiovascular Health
1. Can mental health conditions impact normal blood pressure and pulse readings?
Absolutely. Chronic mental health conditions such as anxiety and depression can significantly influence cardiovascular metrics, including what is considered normal blood pressure and pulse. Individuals with generalized anxiety disorder often exhibit elevated heart rates and blood pressure during periods of acute stress or panic. This heightened physiological response stems from an overactive sympathetic nervous system, which primes the body for a ‘fight or flight’ reaction. Over time, the strain placed on the cardiovascular system can subtly shift baseline vitals, skewing perceptions of normalcy. Understanding the broader implications of mental health on bp vitals meaning allows clinicians to better contextualize fluctuations and determine whether they represent transient psychological responses or emerging physiological patterns.
2. How does climate and altitude affect blood pressure and pulse readings?
Environmental factors such as climate and elevation can play a surprisingly large role in influencing normal blood pressure and pulse. At high altitudes, oxygen availability decreases, causing the body to compensate by increasing heart rate and sometimes blood pressure. This response helps ensure adequate oxygen delivery to tissues but can mimic pathological readings if not interpreted correctly. Similarly, extreme heat or humidity can lower blood pressure temporarily through vasodilation and fluid loss, sometimes accompanied by an elevated pulse. By expanding our understanding of bp vitals meaning to include environmental context, healthcare providers can avoid misdiagnosing conditions or prescribing unnecessary treatments based solely on readings taken under unusual circumstances.
3. Can your sleep habits affect your pulse pressure chart readings?
Yes, sleep quality and duration have profound effects on cardiovascular regulation and can influence data on a pulse pressure chart. Sleep deprivation often leads to increased sympathetic nervous system activity, which raises both systolic blood pressure and resting pulse, thereby widening pulse pressure. In contrast, adequate and high-quality sleep allows the body to enter a state of parasympathetic dominance, lowering heart rate and blood pressure, and stabilizing cardiovascular rhythms. Over time, poor sleep can lead to persistent deviations in normal blood pressure and pulse, elevating long-term cardiovascular risk. Monitoring bp vitals meaning in the context of sleep habits offers a more holistic view of patient health and can guide more tailored lifestyle recommendations.
4. What role does hydration play in maintaining healthy BP vitals?
Hydration status has a direct and immediate impact on blood pressure and heart rate, making it a critical yet often overlooked component of cardiovascular wellness. Inadequate fluid intake can lead to a drop in blood volume, which may cause hypotension and a compensatory increase in heart rate. On the other hand, overhydration in individuals with kidney or heart issues can increase blood volume excessively, potentially worsening hypertension. By understanding how fluid balance modifies the pulse pressure chart and affects normal blood pressure and pulse, individuals can use hydration as a tool for maintaining equilibrium. This nuanced approach to bp vitals meaning is especially important in elderly populations and those with pre-existing heart or renal conditions.
5. Are there gender differences in interpreting BP vitals and pulse pressure charts?
Yes, gender differences in hormone levels, vascular elasticity, and autonomic regulation all contribute to variations in bp vitals meaning and pulse pressure interpretation. For example, premenopausal women typically have lower systolic blood pressure due to the protective effects of estrogen on vascular tone. However, after menopause, this trend often reverses, with increased pulse pressure and higher cardiovascular risk. Men, conversely, tend to exhibit higher systolic pressures at younger ages and may show signs of arterial stiffness earlier. Recognizing these gender-based variations is essential for accurate interpretation of normal blood pressure and pulse data and for making informed decisions based on pulse pressure chart trends.
6. Can wearable technology accurately track BP vitals and pulse pressure trends?
Wearable devices have revolutionized personal health monitoring, but their reliability in capturing comprehensive bp vitals meaning varies widely. Most wearables provide reasonably accurate heart rate data, particularly during rest. However, their blood pressure estimates, often based on optical sensors and algorithms, can be inconsistent. Despite these limitations, long-term trends captured by wearables—especially for pulse and activity patterns—can offer valuable insight into cardiovascular rhythms. While they may not replace clinical tools for precise pulse pressure chart interpretation, wearables serve as an excellent supplement, prompting users to seek medical evaluation when concerning patterns emerge.
7. How do postural changes affect the interpretation of blood pressure and pulse readings?
Posture significantly affects cardiovascular readings, making context essential when assessing normal blood pressure and pulse. For instance, when moving from a lying to a standing position, blood pressure may momentarily drop, and pulse may rise to compensate for gravitational shifts in blood flow. This phenomenon, known as orthostatic hypotension, can be particularly pronounced in older adults or those on diuretic medications. Misinterpreting these transient changes without considering posture can lead to inaccurate assessments of bp vitals meaning. For meaningful analysis, measurements should ideally be taken under consistent postural conditions, or postural changes should be documented alongside the readings.
8. What do fluctuations in pulse pressure chart values suggest about vascular health?
Pulse pressure fluctuations can be a subtle but telling indicator of vascular health. An increasingly widened pulse pressure over time may point to stiffening arteries, a hallmark of vascular aging and increased cardiovascular risk. Conversely, consistently narrow pulse pressure might suggest reduced cardiac output, potentially linked to heart failure or severe aortic stenosis. These variations are not always captured by standard blood pressure readings alone, which is why the pulse pressure chart provides added diagnostic value. Understanding these shifts can help clinicians implement early interventions before overt symptoms arise, making it a critical component of interpreting bp vitals meaning beyond the basics.
9. Can seasonal changes affect normal blood pressure and pulse values?
Seasonal changes, especially temperature fluctuations, can influence cardiovascular dynamics and subtly alter what’s considered normal blood pressure and pulse. In colder months, vasoconstriction narrows blood vessels, often leading to higher systolic readings, while summer heat encourages vasodilation, potentially lowering blood pressure and increasing heart rate. These physiological adaptations are normal but can be misinterpreted if not seasonally contextualized. Such changes may also impact readings on a pulse pressure chart, which could show artificially widened or narrowed values depending on the ambient conditions. Understanding how seasons shape bp vitals meaning allows for more informed assessments, particularly for those managing chronic cardiovascular conditions.
10. How can psychological awareness and biofeedback training improve BP vitals regulation?
Psychological tools like mindfulness and biofeedback can enhance autonomic regulation, making them effective for improving normal blood pressure and pulse. Biofeedback training helps individuals gain voluntary control over involuntary functions, such as heart rate and vascular tone, by providing real-time data and reinforcing calming strategies. Over time, this can lead to more stable readings on a pulse pressure chart and reduced reliance on medication. Furthermore, understanding bp vitals meaning within the framework of self-awareness promotes greater accountability and engagement with one’s health. These mind-body approaches offer a promising, non-invasive avenue for cardiovascular wellness, particularly when integrated into broader lifestyle and clinical strategies.
Conclusion: What Your BP Vitals and Pulse Pressure Chart Reveal About Long-Term Heart Health
Understanding normal blood pressure and pulse is far more than a matter of checking boxes during a doctor’s visit. These vital signs are windows into the complex interplay between the heart, blood vessels, and nervous system. Their significance deepens when interpreted in the context of a pulse pressure chart, which provides nuanced insight into arterial health and cardiac function. The meaning of BP vitals becomes especially powerful when individuals and healthcare providers work together to track trends, understand influencing factors, and take timely action based on those insights.
Whether through lifestyle changes, medical treatment, or the use of wearable technology, maintaining healthy cardiovascular metrics is within reach for many. It begins with awareness and is sustained through informed choices. By paying attention to the body’s signals and understanding the layered story that blood pressure and pulse tell, individuals can take meaningful steps toward lasting heart health. The tools and knowledge are available—it’s up to each of us to use them wisely and proactively.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Vital Signs (Body Temperature, Pulse Rate, Respiration Rate, Blood Pressure)
Understand Your Blood Pressure Reading Using a Blood Pressure Chart