The human circulatory system is an intricate network of blood vessels that ensure oxygen and nutrients reach every part of the body. Among the most vital components of this system are the arteries, which transport oxygen-rich blood from the heart to tissues and organs. The arteries in the leg play a crucial role in maintaining mobility, sensation, and overall limb health. Without a properly functioning arterial system, the lower extremities would suffer from inadequate blood flow, leading to a range of complications. In this comprehensive exploration, we will delve into the key functions of the arteries in the leg, common vascular issues that affect them, and the warning signs that indicate medical intervention is necessary.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery
The Anatomy and Function of the Arteries in the Leg
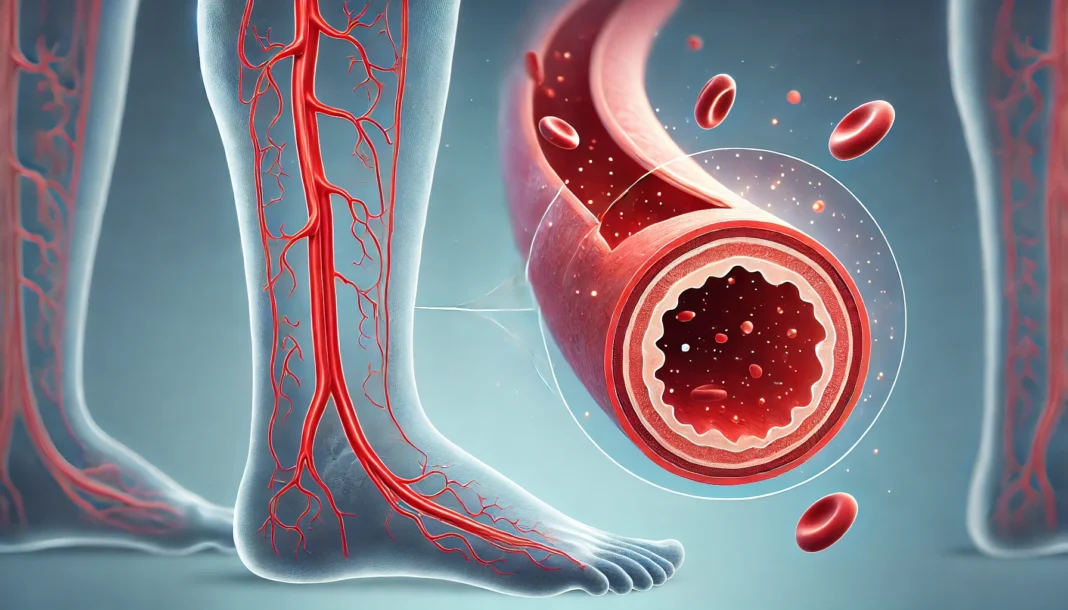
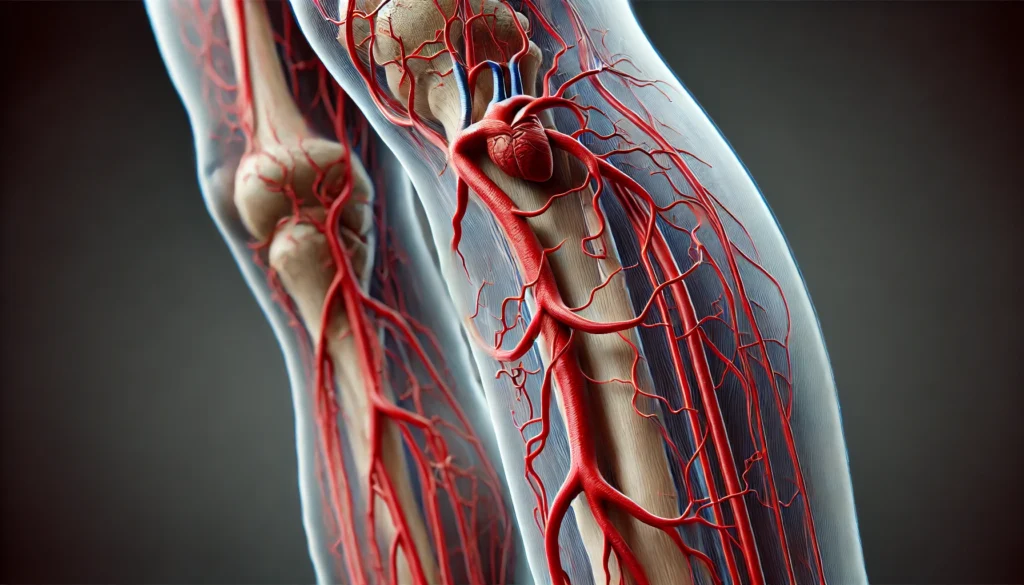
The arterial system in the leg is responsible for delivering oxygenated blood from the heart to the muscles, bones, and tissues of the lower limbs. The primary artery in the leg is the femoral artery, which originates from the external iliac artery and runs down the thigh. It branches into several smaller arteries, including the deep femoral artery and the popliteal artery, which further subdivides into the anterior tibial, posterior tibial, and peroneal arteries. These branches ensure that every region of the lower extremities receives an adequate blood supply.
Each artery serves a specific function. The femoral artery is the main conduit for blood flow to the leg, while the popliteal artery, located behind the knee, plays a pivotal role in supplying blood to the lower leg and foot. The tibial arteries extend down to the foot, ensuring that even the smallest capillaries receive necessary oxygen and nutrients. Without these arteries functioning properly, the tissues of the leg would experience ischemia, a condition characterized by insufficient blood supply that can lead to tissue damage or necrosis.
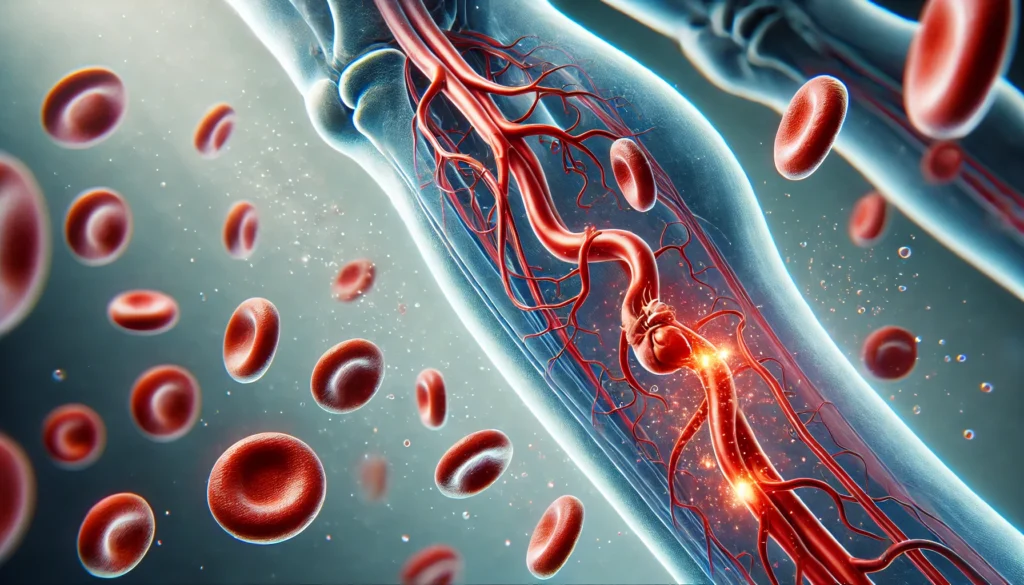
Arterial veins in the leg also play a supportive role, working in tandem with the arterial system to maintain efficient circulation. While veins primarily return deoxygenated blood to the heart, the interaction between arteries and veins is essential for overall vascular health. Arterial and venous coordination ensures that oxygenated and deoxygenated blood circulates efficiently, preventing complications such as swelling, clot formation, and venous insufficiency.
Common Arterial Disorders in the Leg
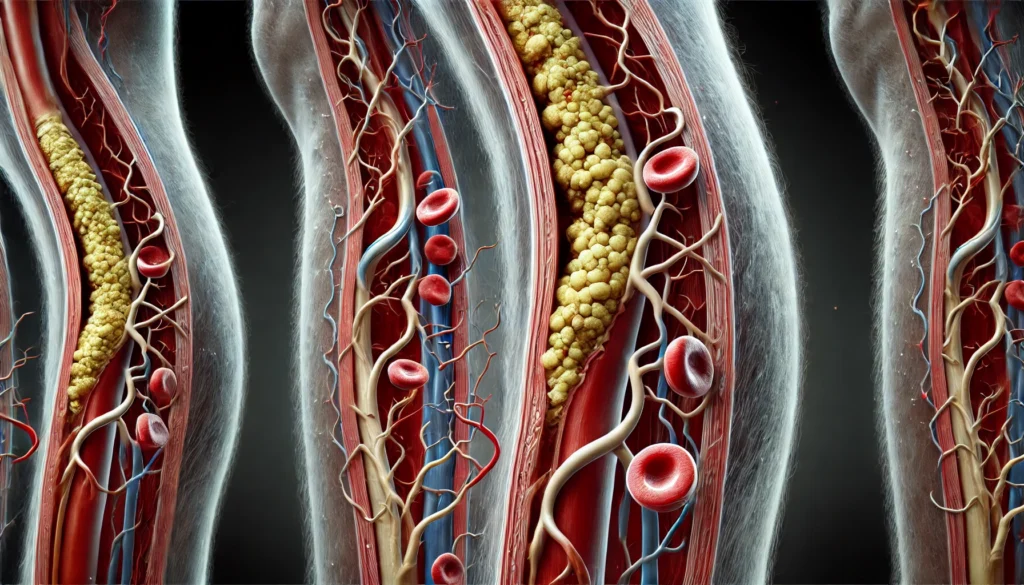
Several conditions can affect the arteries in the leg, leading to compromised blood flow and serious health consequences. One of the most prevalent disorders is peripheral artery disease (PAD), a condition in which plaque buildup narrows the arteries and restricts circulation. PAD is commonly caused by atherosclerosis, a process in which fatty deposits accumulate on arterial walls, reducing their elasticity and obstructing blood flow. Individuals with PAD often experience leg pain, cramping, and fatigue, particularly during physical activity. As the disease progresses, symptoms may worsen, leading to non-healing wounds, infections, and even gangrene in severe cases.
Another common issue is deep vein thrombosis (DVT), which, although primarily a venous condition, can impact arterial health by creating blockages that disrupt normal circulation. DVT occurs when a blood clot forms in a deep vein, typically in the legs, and poses a significant risk if the clot dislodges and travels to the lungs, resulting in a pulmonary embolism. While arterial veins in the leg work to prevent such complications, underlying vascular issues can still contribute to life-threatening conditions.
Aneurysms, though less common, can also develop in the leg’s arteries. A popliteal artery aneurysm, for example, occurs when the artery behind the knee weakens and balloons outward. This condition increases the risk of blood clots, which can obstruct circulation and lead to limb-threatening ischemia. Left untreated, aneurysms can rupture, causing severe internal bleeding and necessitating emergency medical intervention.
Risk Factors and Causes of Arterial Conditions in the Leg
Understanding the factors that contribute to arterial disorders can help individuals take preventive measures to protect their vascular health. Several risk factors predispose individuals to conditions affecting the arteries in the leg, with lifestyle choices playing a significant role. Smoking, for example, is one of the most detrimental habits for arterial health. The chemicals in tobacco damage blood vessel walls, promote inflammation, and accelerate the progression of atherosclerosis, significantly increasing the risk of PAD and other circulatory problems.
Diabetes is another major contributor to arterial disease. Chronically high blood sugar levels damage blood vessels over time, leading to poor circulation and an increased likelihood of developing PAD. Many diabetics suffer from peripheral neuropathy, a condition that reduces sensation in the legs and feet, making them less aware of developing sores or ulcers that can become infected due to inadequate blood flow.
Hypertension, or high blood pressure, also plays a critical role in arterial health. Persistent elevated pressure in the arteries causes wear and tear on the vessel walls, making them more susceptible to plaque buildup and narrowing. Additionally, high cholesterol levels contribute to atherosclerosis by facilitating the accumulation of fatty deposits within the arteries, further restricting circulation.
Genetic factors, while less controllable, can also influence an individual’s risk of developing arterial conditions. A family history of vascular disease increases the likelihood of experiencing similar issues, emphasizing the importance of proactive monitoring and lifestyle modifications to mitigate risks.
When to Seek Medical Help for Arterial Issues
Recognizing the warning signs of arterial disease in the leg is crucial for timely intervention and effective treatment. Symptoms such as persistent leg pain, cramping, or weakness—particularly when walking or exercising—may indicate PAD and should not be ignored. A condition known as claudication, characterized by pain that subsides with rest but returns during activity, is a hallmark of arterial blockages and warrants medical evaluation.
Other concerning symptoms include coldness or numbness in the lower extremities, slow-healing wounds, and discoloration of the skin. In severe cases, individuals may develop critical limb ischemia, a condition where blood flow is so restricted that ulcers and infections become common, posing a significant risk of amputation if left untreated. Any sudden or severe pain, swelling, or changes in skin color should prompt immediate medical attention, as these could indicate an acute arterial blockage or an impending complication.
Physicians use various diagnostic tools to assess arterial health, including ankle-brachial index (ABI) tests, Doppler ultrasound, and angiography. These tests help identify the presence and severity of blockages, allowing healthcare providers to determine the most appropriate course of treatment, which may include lifestyle changes, medication, or surgical intervention.
Frequently Asked Questions (FAQ) About the Arteries in the Leg
What role does the main artery in the leg play in overall circulation?
The main artery in the leg, known as the femoral artery, is critical for supplying oxygenated blood to the lower extremities. It originates from the external iliac artery and travels down the thigh, where it branches into several smaller arteries that provide nutrients and oxygen to muscles and tissues. This continuous blood supply supports mobility, endurance, and wound healing by ensuring that cells receive adequate oxygen and nutrients. If the femoral artery becomes blocked or narrowed, circulation is compromised, leading to pain, weakness, and, in severe cases, tissue damage. Proper circulation in the lower extremities is crucial not only for walking and movement but also for preventing complications like ulcers, infections, and even amputation in extreme cases.
How do arterial veins in the leg support vascular health?
Arterial veins in the leg work alongside arteries to facilitate efficient circulation and maintain a balance between oxygenated and deoxygenated blood flow. While arteries transport oxygen-rich blood from the heart to the tissues, veins return deoxygenated blood back to the heart for reoxygenation. The efficiency of this process depends on the proper functioning of valves in the veins, which prevent blood from pooling or flowing backward. When veins fail to perform effectively, conditions such as venous insufficiency or deep vein thrombosis (DVT) can develop, increasing the risk of swelling, clotting, and impaired circulation. Maintaining healthy veins and arteries through physical activity, hydration, and proper posture can help prevent these complications.
Can poor circulation in the arteries in the leg lead to permanent damage?
Yes, prolonged poor circulation in the arteries in the leg can result in serious and sometimes irreversible damage. When blood flow is significantly reduced due to arterial blockages, tissues may not receive enough oxygen, leading to ischemia. Over time, this lack of oxygen can cause muscle weakness, chronic pain, slow-healing wounds, and, in extreme cases, tissue necrosis. If left untreated, conditions such as peripheral artery disease (PAD) or critical limb ischemia (CLI) can increase the risk of amputation. Early detection and intervention, including lifestyle changes, medication, and in some cases, surgical procedures, can help prevent permanent damage and restore proper circulation.
What are the early warning signs of arterial disease in the leg?
The earliest symptoms of arterial disease in the leg often include intermittent claudication, which is characterized by pain, cramping, or fatigue in the legs during physical activity that subsides with rest. Other warning signs may include coldness or numbness in the feet, slow-healing sores, and changes in skin color, such as paleness or a bluish tint. In more advanced cases, individuals may notice hair loss on the legs, brittle toenails, and even ulcers or wounds that do not heal properly. These symptoms should not be ignored, as they can indicate the progression of vascular disease that may require medical intervention. Seeking medical attention at the onset of symptoms can help prevent further complications and improve long-term outcomes.
How can lifestyle changes improve arterial health in the legs?
Implementing key lifestyle changes can significantly improve arterial health and prevent conditions such as atherosclerosis, which contributes to artery narrowing and reduced blood flow. Regular physical activity, particularly exercises that promote circulation such as walking, cycling, or swimming, can enhance blood vessel function and reduce the risk of arterial blockages. Maintaining a heart-healthy diet that is low in saturated fats and rich in fiber can help control cholesterol levels, preventing the buildup of fatty plaques in the arteries. Quitting smoking is one of the most impactful steps individuals can take, as tobacco use directly damages blood vessels and accelerates the development of arterial disease. Managing underlying conditions such as diabetes and hypertension through medication and dietary modifications can also play a crucial role in preserving vascular health.
Are there medical treatments available for arterial blockages in the leg?
Yes, a variety of medical treatments are available to address arterial blockages in the leg, depending on the severity of the condition. In early stages, medications such as statins, blood thinners, and vasodilators can help manage symptoms and slow disease progression. Minimally invasive procedures like angioplasty and stent placement can open narrowed arteries and restore normal blood flow. In more advanced cases, surgical interventions such as bypass surgery may be necessary to create an alternative route for blood circulation. Physicians may also recommend supervised exercise therapy, which has been shown to improve symptoms and overall vascular function in individuals with PAD. Seeking early medical consultation can help determine the best treatment strategy for maintaining leg artery health.
How does diabetes affect the arteries in the leg?
Diabetes has a profound impact on the arteries in the leg, as consistently high blood sugar levels contribute to vascular damage over time. Elevated glucose levels promote inflammation and stiffening of the arterial walls, making them more susceptible to plaque buildup and narrowing. This condition, known as diabetic angiopathy, increases the risk of developing peripheral artery disease, leading to reduced circulation and slower wound healing. Additionally, diabetes-related nerve damage (neuropathy) can mask symptoms of arterial disease, making it difficult for individuals to recognize circulation problems until complications arise. Managing blood sugar levels through proper diet, medication, and regular medical check-ups is essential for protecting vascular health and preventing diabetes-related complications in the legs.
Can exercise help improve circulation in the arteries in the leg?
Yes, exercise is one of the most effective ways to enhance circulation and improve arterial health in the legs. Regular physical activity stimulates blood flow, strengthens blood vessels, and encourages the formation of new capillaries, which help compensate for reduced circulation due to blockages. Walking, in particular, is highly beneficial for individuals with peripheral artery disease, as it promotes the development of collateral circulation—alternative pathways that bypass narrowed arteries. Low-impact exercises like swimming and cycling can also improve vascular function without putting excessive strain on the joints. Consistency is key, and individuals should aim for at least 30 minutes of moderate exercise most days of the week to maintain optimal circulation.
What is the difference between arterial veins in the leg and regular veins?
The term “arterial veins in the leg” is sometimes used to describe the interplay between the arterial and venous systems rather than a distinct type of blood vessel. Arteries carry oxygen-rich blood from the heart to the lower extremities, while veins return oxygen-depleted blood back to the heart. Unlike veins, arteries have thick, muscular walls that can withstand high-pressure blood flow. Veins, on the other hand, rely on valves to prevent blood from flowing backward. Both systems must function efficiently to ensure proper circulation, and any disruption in either can lead to conditions such as varicose veins, venous insufficiency, or arterial blockages.
When should someone see a doctor for leg artery problems?
Medical attention should be sought as soon as symptoms of poor circulation or arterial disease appear. Persistent leg pain, numbness, skin discoloration, or slow-healing wounds are all signs that circulation may be compromised. If symptoms worsen over time or interfere with daily activities, a vascular specialist can perform diagnostic tests such as an ankle-brachial index (ABI) or Doppler ultrasound to assess blood flow. Delaying medical care can increase the risk of complications, including critical limb ischemia, which may require more aggressive treatment such as surgery or limb amputation. Early detection and intervention can improve outcomes and help preserve mobility and overall health.
Conclusion
The arteries in the leg are vital for sustaining healthy circulation and ensuring the lower extremities receive the oxygen and nutrients they need. However, various conditions, including peripheral artery disease, aneurysms, and deep vein thrombosis, can compromise arterial function and lead to severe health consequences. Understanding the risk factors, recognizing early symptoms, and seeking timely medical care can help prevent complications and improve overall vascular health. By adopting lifestyle changes, such as quitting smoking, managing diabetes, and maintaining a healthy blood pressure, individuals can significantly reduce their risk of arterial disease. If symptoms of arterial dysfunction arise, prompt medical evaluation is essential to prevent further deterioration and ensure the best possible outcomes.
leg artery health, blood circulation in legs, vascular health tips, peripheral artery disease prevention, femoral artery function, improving leg blood flow, signs of poor circulation, managing vascular disease, healthy arteries and veins, leg pain and circulation, blocked arteries symptoms, diabetes and circulation, preventing blood clots, artery disease risk factors, best exercises for circulation, maintaining vascular health, leg artery blockage treatment, symptoms of arterial insufficiency, impact of smoking on circulation, arterial health and aging
Further Reading:
Vascular Disease (Vasculopathy)
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.