The human heart is a marvel of biological engineering, with a network of coronary arteries that supply oxygenated blood to its muscles, ensuring continuous function. Among these, the left circumflex coronary artery (LCX artery) plays a pivotal role in maintaining cardiac health. Understanding the left circumflex coronary artery, its function, the disorders associated with it, and the available treatment options is essential for both medical professionals and individuals interested in cardiovascular health. This comprehensive article delves into the anatomy, physiological significance, potential complications, and current therapeutic advancements related to the LCX artery.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery
The Anatomy and Function of the Left Circumflex Coronary Artery
The left circumflex coronary artery, commonly referred to as the circumflex artery, originates from the left main coronary artery and follows a distinctive course around the heart. This vessel is responsible for supplying oxygen-rich blood to the lateral and posterior walls of the left ventricle, as well as parts of the left atrium. It branches out into several smaller arteries, including the circumflex branch artery, obtuse marginal artery, and left marginal artery, all of which contribute to the heart’s intricate blood supply network.
The circumflex coronary artery encircles the left side of the heart, traveling in the coronary sulcus and providing blood to essential myocardial regions. The obtuse marginal artery, a significant branch of the left circumflex, supplies the lateral wall of the left ventricle. Other important branches include the circumflex branch and the left obtuse marginal artery, both of which contribute to maintaining a robust and uninterrupted blood flow. The importance of these vessels cannot be overstated, as their functionality ensures that the heart muscle remains nourished and capable of sustaining its rhythmic contractions.
Common Disorders Affecting the Left Circumflex Coronary Artery
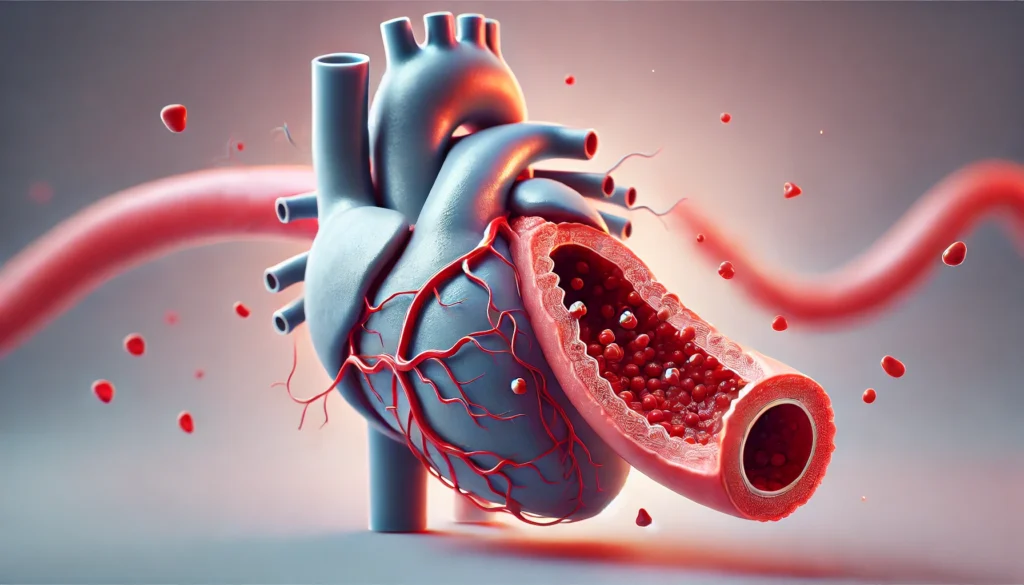
Like other coronary arteries, the LCX artery is susceptible to various cardiovascular disorders, including atherosclerosis, ischemic heart disease, and coronary artery anomalies. Atherosclerosis, a condition characterized by the buildup of plaque within arterial walls, can significantly narrow the lumen of the circumflex heart artery, impeding blood flow. This can lead to angina, myocardial infarction, or even sudden cardiac death if left untreated.
Another serious condition is coronary artery disease (CAD), which often affects the left circumflex artery alongside other coronary vessels. In CAD, the progressive narrowing of the artery reduces oxygen supply to the heart, increasing the risk of ischemic episodes. Additionally, anomalies such as an absent or hypoplastic circumflex branch artery can compromise blood distribution, resulting in congenital heart defects. Understanding these disorders and their impact on the cardiovascular system is crucial for early diagnosis and effective intervention.
Symptoms and Diagnostic Approaches
Symptoms of LCX artery disorders can vary widely, depending on the severity of the blockage or abnormality. Individuals may experience chest pain (angina), shortness of breath, fatigue, or even arrhythmias. In severe cases, complete occlusion of the circumflex coronary artery can precipitate a heart attack, manifesting as intense chest pain, nausea, and diaphoresis.
To accurately diagnose left circumflex artery disease, several imaging and diagnostic techniques are employed. Coronary angiography, a gold standard procedure, allows for direct visualization of arterial blockages. Additionally, non-invasive modalities such as computed tomography angiography (CTA), magnetic resonance imaging (MRI), and stress echocardiography provide valuable insights into coronary blood flow and myocardial perfusion. Identifying the extent of obstruction and evaluating cardiac function are essential steps in formulating an appropriate treatment plan.
Treatment Options for LCX Artery Disorders
Treatment for left circumflex artery disease varies based on the severity and underlying cause of the condition. Lifestyle modifications, including dietary changes, regular exercise, and smoking cessation, are often recommended as the first line of defense against atherosclerosis and CAD. Medications such as statins, beta-blockers, and antiplatelet agents play a crucial role in managing symptoms and reducing cardiovascular risk.
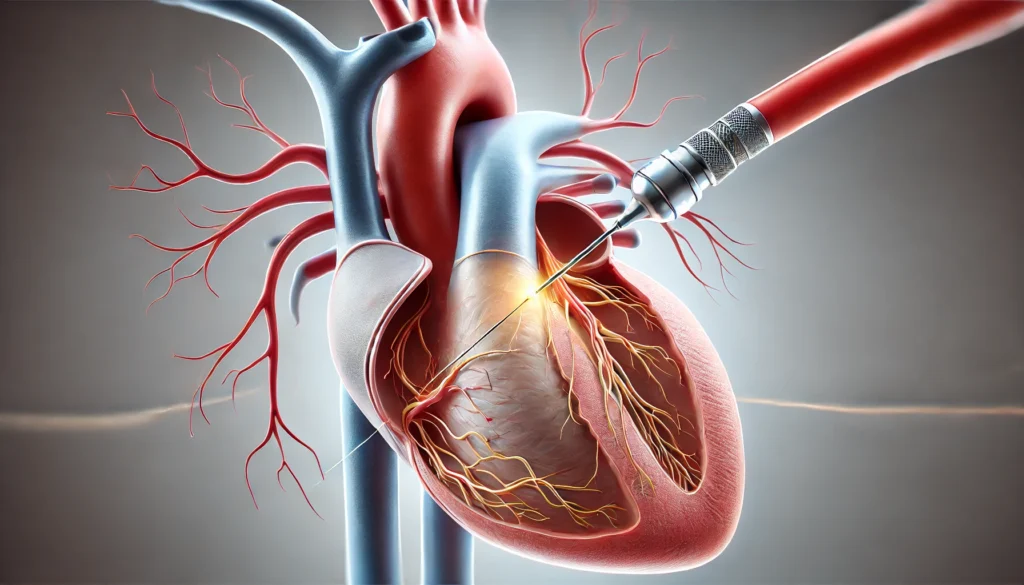
For more advanced cases, interventional procedures such as percutaneous coronary intervention (PCI) with stent placement may be necessary to restore proper blood flow. In cases of severe multi-vessel disease, coronary artery bypass grafting (CABG) remains a viable and effective surgical option. Emerging treatments, including minimally invasive robotic-assisted surgeries and gene therapy approaches, offer promising advancements in the management of LCX artery disorders.

Frequently Asked Questions (FAQ) About the Left Circumflex Coronary Artery
1. What is the significance of the left circumflex coronary artery in overall heart health?
The left circumflex coronary artery plays a crucial role in supplying oxygenated blood to the lateral and posterior regions of the heart, particularly the left ventricle and left atrium. Without adequate blood flow from the left circumflex, the heart muscle can become deprived of oxygen, increasing the risk of ischemic damage. This artery works in conjunction with the left anterior descending artery and right coronary artery to ensure complete perfusion of the heart. Because of its location, blockages in the left circumflex coronary artery can lead to specific types of heart attacks that affect the back and side of the heart, sometimes making them harder to detect than those involving the left anterior descending artery. Regular cardiovascular screenings, including stress tests and imaging studies, can help monitor the health of the left circumflex and prevent complications.
2. How does the anatomy of the left circumflex artery differ from other coronary arteries?
Unlike the left anterior descending artery, which runs along the front of the heart, the left circumflex artery wraps around the heart’s left side in the coronary sulcus. The circumflex heart artery branches off into smaller vessels, including the obtuse marginal artery and left marginal artery, which further distribute blood to the myocardium. Another distinguishing feature is its variability in dominance—while in most individuals, the right coronary artery is dominant, in about 15-20% of people, the left circumflex artery extends further to supply the posterior descending artery, making it the dominant artery. This variability impacts how blood flow is restored in cases of coronary artery disease. Understanding these anatomical differences is essential for cardiologists planning interventions such as bypass grafting or angioplasty.
3. What are the early warning signs of left circumflex artery disease?
Symptoms of left circumflex artery disease can be subtle compared to other coronary conditions, but they often include exertional chest pain, fatigue, and breathlessness. Because the left circumflex supplies the lateral and posterior heart walls, pain may radiate to the back or left shoulder rather than the more classic left-sided chest pain. Silent ischemia—reduced blood flow without noticeable symptoms—can also occur, especially in individuals with diabetes or older adults. In some cases, irregular heart rhythms may be an early sign of poor perfusion due to left circumflex narrowing. Identifying these symptoms early through routine cardiovascular check-ups can lead to better outcomes.
4. How do lifestyle choices impact the health of the left circumflex artery?
Lifestyle factors significantly influence the health of the left circumflex artery, as well as other coronary arteries. A diet high in saturated fats and processed sugars contributes to atherosclerosis, which can narrow the artery and reduce blood flow. Regular physical activity helps maintain arterial flexibility and prevents plaque accumulation, which is crucial for the circumflex branch and obtuse marginal artery. Chronic stress and poor sleep patterns can elevate cortisol and blood pressure levels, which may contribute to endothelial dysfunction and arterial stiffness. Additionally, smoking introduces harmful chemicals that accelerate arterial damage, leading to increased susceptibility to ischemic heart disease. Implementing a heart-healthy lifestyle, including a balanced diet, exercise, and stress management, can protect the left circumflex and overall cardiovascular health.
5. How does the left circumflex artery interact with other coronary vessels?
The left circumflex artery functions within a complex network of coronary vessels that work together to provide continuous myocardial perfusion. It anastomoses with the right circumflex artery in some individuals, creating collateral circulation that can help compensate for blockages. The circumflex branch artery and left obtuse marginal artery extend from the left circumflex, ensuring efficient blood distribution to the lateral myocardium. When there is a blockage in the left circumflex, the right coronary artery may partially compensate through collateral pathways, though this is not always sufficient to prevent ischemia. Understanding these vascular interactions helps cardiologists determine the best treatment strategies for coronary artery disease.
6. What imaging techniques are most effective for diagnosing left circumflex artery disease?
Coronary angiography remains the gold standard for directly visualizing left circumflex artery disease, allowing interventional cardiologists to assess the severity of blockages. Non-invasive imaging, such as coronary computed tomography angiography (CTA), provides a detailed view of arterial plaques and luminal narrowing. Stress echocardiography can be useful in detecting ischemia related to left circumflex blockages by evaluating heart function under exertion. In cases where small branches such as the circumflex branch artery or obtuse marginal artery are involved, magnetic resonance angiography (MRA) may offer additional insights. Choosing the right diagnostic method depends on the patient’s symptoms, risk factors, and the suspected extent of arterial involvement.
7. What are the surgical and non-surgical treatment options for left circumflex artery disease?
Treatment for left circumflex artery disease depends on the severity of arterial blockage and the patient’s overall health. Non-surgical approaches include lifestyle modifications, medications such as statins and antiplatelet therapy, and enhanced external counterpulsation (EECP), which can improve collateral circulation. In cases where narrowing is significant, percutaneous coronary intervention (PCI) with stent placement can restore blood flow. For patients with extensive disease affecting multiple vessels, coronary artery bypass grafting (CABG) using a vein or artery graft to bypass the left circumflex artery may be necessary. Recent advancements in minimally invasive robotic-assisted surgeries have made some procedures less invasive, reducing recovery time while ensuring effective revascularization.
8. How does left circumflex artery disease differ from right circumflex artery disease?
While both the left circumflex and right circumflex arteries play critical roles in coronary circulation, they supply different heart regions and have distinct clinical implications when diseased. The right circumflex artery primarily supplies blood to the right ventricle, right atrium, and parts of the posterior heart, whereas the left circumflex focuses on the lateral and posterior left ventricle. Because of this, a blockage in the right circumflex artery may cause inferior myocardial infarctions, while left circumflex occlusion often leads to lateral or posterior infarctions. Understanding these differences is important for tailored treatment approaches and predicting patient outcomes following an acute coronary event.
9. Can collateral circulation help compensate for a blocked left circumflex artery?
Collateral circulation is the body’s natural ability to develop alternative blood flow pathways in response to arterial blockages. When the left circumflex artery becomes narrowed, small blood vessels may form connections with branches of the right circumflex artery or the left anterior descending artery. This process can help preserve myocardial function, though it is often insufficient in completely preventing ischemic damage. Exercise and certain medications, such as statins, have been shown to promote collateral vessel development over time. While collateral circulation is beneficial, severe obstructions in the left circumflex still require medical intervention to ensure adequate blood flow to the heart muscle.
10. What future advancements are being explored for treating left circumflex artery disease?
The field of cardiology continues to advance, with new treatments emerging for left circumflex artery disease. Research is exploring bioresorbable stents that gradually dissolve after restoring blood flow, reducing the long-term risks associated with metal stents. Gene therapy is being investigated as a means to promote new blood vessel growth in ischemic areas, potentially benefiting patients with extensive left circumflex artery disease. Artificial intelligence is also playing a role in diagnosing and predicting coronary artery disease progression, enabling more personalized treatment strategies. Additionally, advancements in catheter-based interventions are making percutaneous procedures safer and more efficient. These innovations hold promise for improving patient outcomes and reducing the burden of coronary artery disease worldwide.
Conclusion: Prioritizing Cardiovascular Health and Awareness
Understanding the left circumflex coronary artery and its significance in cardiovascular function is essential for both medical professionals and the general population. Awareness of common disorders, their symptoms, and available treatments can aid in early detection and prompt medical intervention, reducing the risk of severe cardiac events. As medical research continues to advance, innovative diagnostic and therapeutic approaches will further enhance our ability to treat and manage left circumflex artery diseases effectively. Prioritizing heart health through preventive measures, lifestyle modifications, and regular medical check-ups remains a cornerstone of cardiovascular wellness.
coronary artery circulation, cardiac blood supply, myocardial ischemia, heart attack prevention, coronary artery function, left heart circulation, cardiac perfusion, coronary artery occlusion, cardiovascular health tips, cardiac imaging techniques, angioplasty and stenting, coronary artery disease management, heart disease risk factors, myocardial infarction symptoms, cardiac rehabilitation strategies, advanced heart treatments, coronary artery bypass grafting, lifestyle changes for heart health, emerging heart disease therapies, heart health supplements
Further Reading:
A Practical Approach to Left Main Coronary Artery Disease
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


