In recent years, the landscape of hypertension diagnosis and management has undergone significant transformation. As the burden of cardiovascular disease continues to rise globally, the importance of clear and effective guidance for identifying and treating high blood pressure has become ever more urgent. The release of new blood pressure guidelines in the United States, particularly those informed by the American Heart Association (AHA), marks a pivotal shift in how clinicians evaluate and respond to hypertension. These updated recommendations reflect a growing understanding of cardiovascular risk, early intervention strategies, and the long-term impact of even modest elevations in blood pressure.
The AHA guidelines for hypertension, which are widely regarded as a benchmark for cardiovascular care, have redefined what constitutes high blood pressure and how it should be categorized. This reclassification has important implications for both clinicians and patients, influencing everything from screening protocols to treatment thresholds. By revisiting the guideline for high blood pressure, healthcare professionals are equipped with a more nuanced framework to assess cardiovascular risk and intervene earlier, potentially preventing serious outcomes like heart attacks, strokes, and kidney damage.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Understanding the AHA Definition of Hypertension
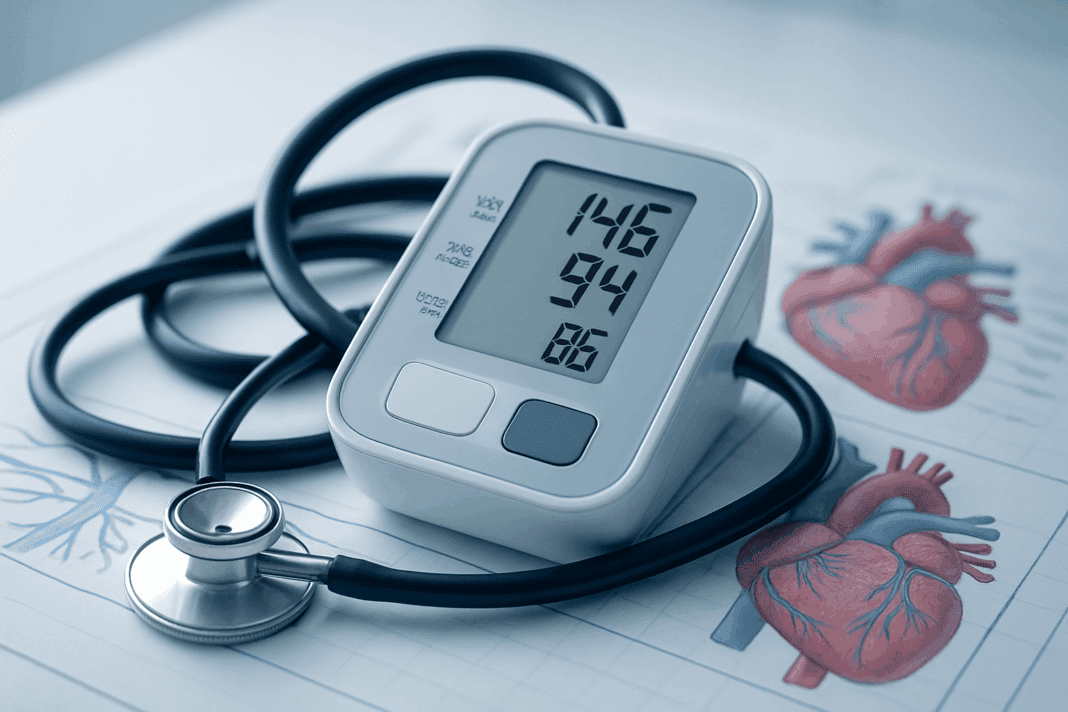
Central to the new guidelines is a revised understanding of what constitutes hypertension. According to the AHA definition of hypertension, a systolic blood pressure of 130 mm Hg or higher, or a diastolic pressure of 80 mm Hg or higher, now qualifies as high blood pressure. This represents a significant change from previous definitions, which typically set the threshold at 140/90 mm Hg. The rationale for this shift is grounded in extensive research demonstrating that even lower levels of blood pressure can significantly increase the risk of cardiovascular events.
This updated definition is not merely semantic. It underscores the critical need for early detection and intervention, especially in populations at heightened risk. The lowered blood pressure cut off is intended to prompt lifestyle changes and, when necessary, medical therapy before complications arise. By expanding the scope of individuals considered to have hypertension, the guidelines aim to facilitate a more proactive approach to cardiovascular health. This also aligns with broader public health goals to reduce the prevalence of heart disease and stroke through earlier and more aggressive risk management.
The Evolution of Hypertension Guidelines in the United States
The trajectory of hypertension guidelines in the United States reveals a dynamic interplay between evolving scientific evidence and clinical practice. Historically, guidelines for managing high blood pressure were more lenient, with higher thresholds for diagnosis and treatment initiation. However, landmark studies like the Systolic Blood Pressure Intervention Trial (SPRINT) have shown that tighter control of blood pressure can yield significant cardiovascular benefits, even in older adults and those with high-risk profiles.
In response to this evidence, the AHA and the American College of Cardiology (ACC) jointly released new blood pressure guidelines that emphasized earlier diagnosis and more individualized treatment strategies. These guidelines not only revised the hypertension classification system but also highlighted the importance of integrating clinical judgment with standardized protocols. The shift represents a departure from a one-size-fits-all approach, favoring a more tailored model that considers each patient’s unique risk factors and comorbidities.

Hypertension Classification and Its Clinical Relevance
One of the most consequential aspects of the updated guidelines is the new system for hypertension classification. According to the classification of high blood pressure established by the AHA and ACC, blood pressure readings are now categorized into several stages: normal (<120/80 mm Hg), elevated (120–129/<80 mm Hg), Stage 1 hypertension (130–139/80–89 mm Hg), and Stage 2 hypertension (140/90 mm Hg or higher). This more granular classification system helps clinicians better understand the severity of a patient’s condition and make more informed decisions about treatment.
The implications of this classification extend beyond nomenclature. For example, individuals with Stage 1 hypertension may not require pharmacological treatment if they are at low risk for cardiovascular disease, but they should still receive counseling on lifestyle modifications. Conversely, patients with elevated cardiovascular risk may benefit from early initiation of antihypertensive medication even at lower thresholds. This nuanced approach allows for greater precision in managing hypertension and reduces the likelihood of both undertreatment and overtreatment.

Impacts on Clinical Practice and Patient Outcomes
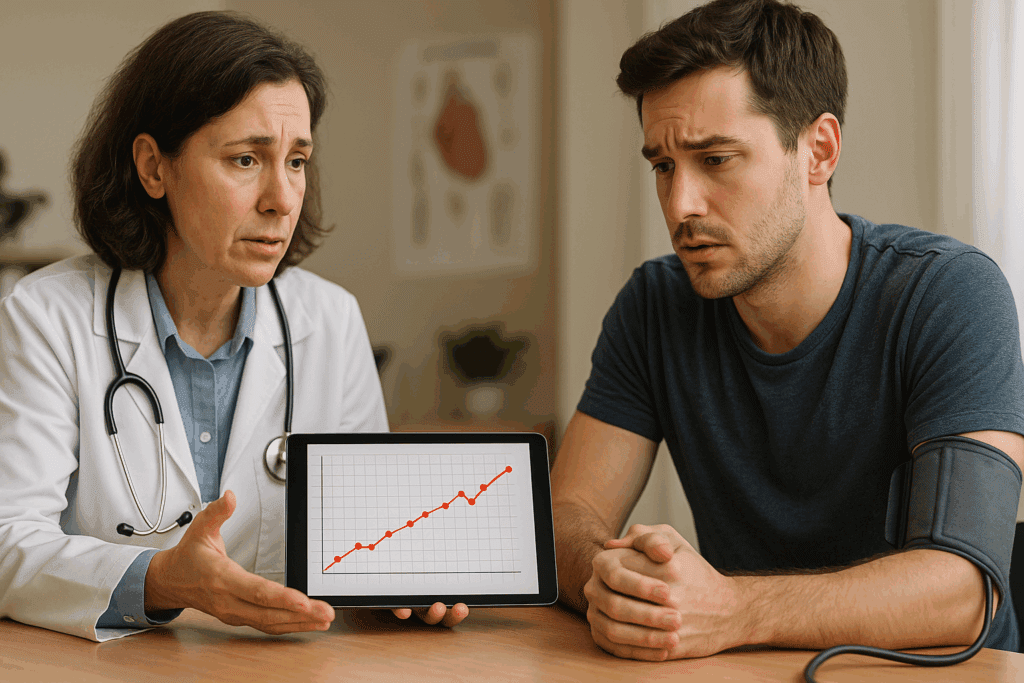
The adoption of the guideline for high blood pressure as defined by the new standards has introduced significant changes in clinical practice. Primary care providers, cardiologists, and other healthcare professionals are now encouraged to adopt a more aggressive stance in identifying and managing high blood pressure. This includes greater reliance on home blood pressure monitoring, more frequent assessments, and a stronger emphasis on patient education.
For patients, these changes can be empowering. The heightened awareness and earlier detection of hypertension offer more opportunities to engage in preventive behaviors, such as dietary changes, increased physical activity, and smoking cessation. Moreover, by catching hypertension earlier, clinicians can tailor interventions that are less invasive and more sustainable over the long term. Patients are also more likely to understand the importance of managing their blood pressure proactively, especially when they are educated about the broader health implications.
Implementing the AHA Guidelines for Hypertension in Diverse Populations
A crucial aspect of the new blood pressure guidelines is their emphasis on equity and inclusivity. Hypertension does not affect all populations equally; disparities in prevalence, access to care, and treatment outcomes are well-documented. The AHA guidelines for hypertension take these disparities into account by encouraging clinicians to consider social determinants of health and cultural factors when evaluating and treating patients.
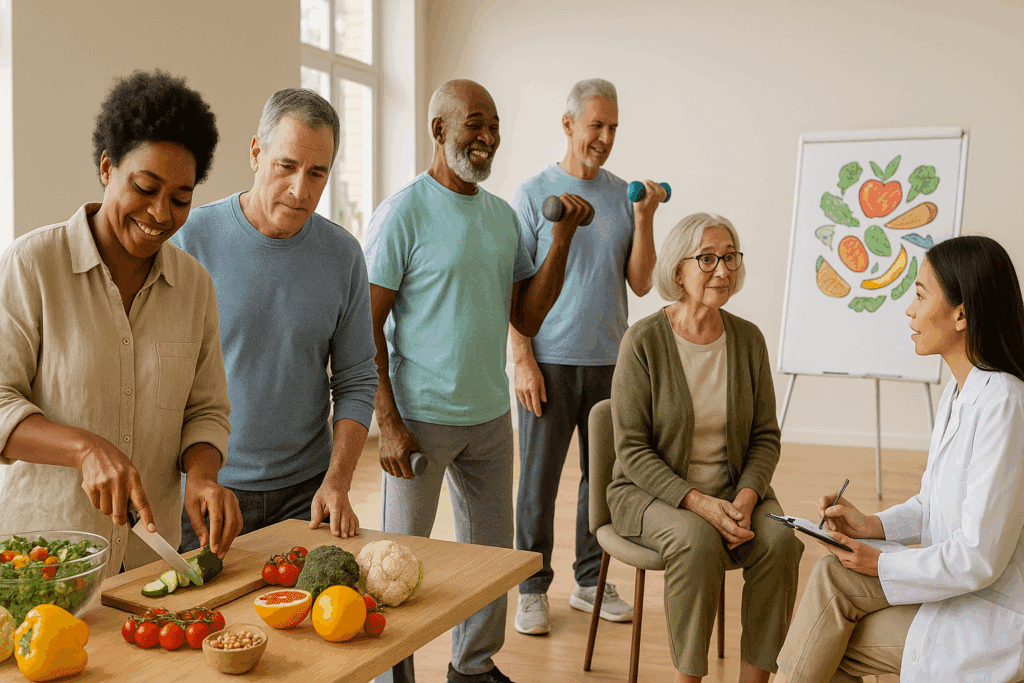
For instance, African American adults are disproportionately affected by high blood pressure and its complications. Tailoring interventions to this population, such as promoting culturally appropriate dietary changes and improving access to affordable medications, can significantly enhance outcomes. Similarly, the guidelines advocate for greater use of community health programs and partnerships to extend hypertension management beyond traditional healthcare settings.
Integration with Lifestyle Medicine and Preventive Care
One of the defining features of the updated hypertension guidelines in the United States is their integration with lifestyle medicine. Rather than relying solely on medication, the guidelines place strong emphasis on lifestyle interventions as first-line therapy, particularly for those with Stage 1 hypertension and no history of cardiovascular disease. This includes recommendations for the DASH (Dietary Approaches to Stop Hypertension) diet, sodium reduction, regular physical activity, moderation of alcohol intake, and weight management.
These recommendations are supported by a robust body of evidence. Clinical trials have shown that lifestyle modifications can lead to meaningful reductions in blood pressure, sometimes rivaling the effects of medication. Moreover, lifestyle changes often have synergistic benefits, improving lipid profiles, insulin sensitivity, and overall metabolic health. By promoting holistic care, the guidelines empower patients to take a more active role in managing their health, thereby fostering long-term adherence and better outcomes.

Technological Advancements and Home Monitoring
The shift toward early and aggressive hypertension management has been facilitated by advancements in health technology. Home blood pressure monitoring devices are now more accurate, affordable, and user-friendly than ever before. The guidelines encourage the use of these devices to provide a more accurate picture of a patient’s blood pressure over time, which is particularly useful for diagnosing white coat hypertension and masked hypertension.
Telemedicine and digital health platforms have also become essential tools in implementing the new guidelines. These technologies allow for remote monitoring, virtual consultations, and real-time feedback, thereby enhancing continuity of care. For patients in rural or underserved areas, such tools can bridge gaps in access and ensure that blood pressure control remains a priority, even outside of traditional clinical settings. These innovations align with the broader goals of the guideline htn recommendations, which emphasize accessibility, accuracy, and individualized care.
Challenges in Implementation and Provider Education
Despite the numerous benefits of the new blood pressure guidelines, implementation remains a challenge. Many providers still adhere to outdated protocols, and there is often a lag in the adoption of new clinical practices. This underscores the need for ongoing education and training, particularly in primary care settings where hypertension is most commonly managed.
Professional societies and academic institutions have a vital role to play in disseminating the updated guidelines and supporting clinicians in their application. Continuing medical education programs, clinical decision support tools, and peer-reviewed literature can help bridge knowledge gaps and reinforce best practices. Additionally, aligning reimbursement models with guideline-based care can incentivize providers to prioritize blood pressure management, ultimately improving adherence and patient outcomes.
Looking Ahead: Future Directions in Hypertension Research and Policy
As our understanding of hypertension evolves, so too will the guidelines that govern its diagnosis and treatment. Future iterations of the guideline for high blood pressure may incorporate emerging biomarkers, genetic risk factors, and novel therapeutics. Personalized medicine, powered by advancements in genomics and artificial intelligence, promises to revolutionize how clinicians assess and manage cardiovascular risk.
Policy initiatives will also play a critical role. Expanding access to affordable healthcare, improving health literacy, and addressing social determinants of health are all essential to achieving the goals set forth by the AHA guidelines for hypertension. Collaboration between public health agencies, healthcare systems, and community organizations will be necessary to implement these changes on a broad scale. By fostering a supportive ecosystem for hypertension management, we can make meaningful strides in reducing the burden of cardiovascular disease.
Frequently Asked Questions: Navigating the New Blood Pressure Guidelines and Hypertension Classification
1. How do the new blood pressure guidelines influence health screenings in younger adults?
The new blood pressure guidelines have broadened the scope of hypertension detection among younger populations who were traditionally not seen as high-risk. With the updated blood pressure cut off set at 130/80 mm Hg, younger adults may now receive earlier interventions that focus on lifestyle modifications rather than medications. This is particularly valuable given the growing incidence of prehypertension in individuals under 40, which often goes undetected. Early diagnosis through more frequent screenings not only promotes healthier habits at a younger age but also reduces the cumulative risk of cardiovascular disease later in life. These refined hypertension guidelines in the United States allow clinicians to intervene at a stage where long-term damage can still be prevented, leading to better health trajectories across the lifespan.
2. What psychological impact can a hypertension diagnosis based on the new guidelines have?
Receiving a hypertension diagnosis under the new blood pressure guidelines can be psychologically complex. While early identification is clinically beneficial, being labeled hypertensive at lower thresholds can induce anxiety or feelings of vulnerability, especially in patients with no prior health issues. This underscores the importance of clinician-patient communication, ensuring that the guideline for high blood pressure is framed as an opportunity for prevention rather than a definitive sign of illness. Addressing patient concerns and offering mental health support, especially in primary care settings, can help mitigate potential stress. Educating patients on how the AHA guidelines for hypertension reflect proactive healthcare rather than disease labeling is key to managing psychological responses effectively.
3. How does the updated hypertension classification affect health insurance policies?
The redefined hypertension classification has begun to influence how health insurers assess risk and determine eligibility or premiums. While it varies by provider, some insurers may view individuals newly classified under the guideline htn criteria as higher risk, potentially affecting access to preferred rates. However, forward-thinking insurance companies are now offering wellness incentives or discounted premiums for individuals actively managing their blood pressure through lifestyle changes. These shifts reflect a growing alignment between the classification of high blood pressure and preventive care initiatives in public health. It also suggests that patients can benefit from engaging with their insurers about how their proactive health behaviors, informed by current hypertension guidelines, can lead to better coverage options.
4. Are digital health tools helping patients adhere to the guideline for high blood pressure?
Yes, digital health innovations play a critical role in supporting patients as they navigate the expectations of the guideline for high blood pressure. Mobile apps now allow users to track daily readings, medication adherence, diet, and physical activity—all of which contribute to sustained blood pressure control. Integration with wearables and telemedicine platforms enables real-time feedback and physician monitoring, reinforcing patient engagement. These tools are especially helpful in underserved or rural areas where in-person access to specialists is limited. By leveraging technology, patients can better align their lifestyle with the objectives of hypertension guidelines in the United States, promoting a more empowered and self-managed approach to care.
5. What role does workplace health policy play under the new blood pressure guidelines?
Workplace wellness programs are increasingly aligning with the new blood pressure guidelines to support employee health and productivity. Many employers now offer free screenings, nutrition education, and fitness incentives based on data tied to the AHA guidelines for hypertension. The classification of high blood pressure as a major chronic condition in occupational health settings has led to changes in how absenteeism and health-related productivity losses are managed. By identifying employees who fall within the updated blood pressure cut off and offering supportive resources, employers can reduce healthcare costs and improve overall workplace morale. This intersection of hypertension guidelines and corporate wellness demonstrates how public health strategies can influence private sector policies.
6. Are there any controversies surrounding the AHA definition of hypertension?
Some experts have debated whether the AHA definition of hypertension lowers diagnostic thresholds too far, potentially leading to overtreatment. Critics argue that labeling large portions of the population as hypertensive based solely on the revised blood pressure cut off may encourage unnecessary pharmacological interventions. However, proponents emphasize that the updated definition enables earlier risk identification, especially when accompanied by lifestyle-based strategies. The hypertension classification changes are rooted in robust evidence, yet ongoing discourse continues around balancing early detection with individualized care. These conversations illustrate the complexity of implementing hypertension guidelines while maintaining patient-centered, evidence-informed practice.
7. How are rural healthcare systems adapting to the new hypertension guidelines?
Rural healthcare systems often face resource constraints that make it challenging to fully implement new hypertension guidelines. However, initiatives such as telehealth expansion and mobile clinics are helping bridge the gap by delivering guideline htn care directly to remote populations. Training programs for rural healthcare providers now increasingly incorporate up-to-date hypertension classification and treatment protocols. Community-based outreach efforts, including partnerships with local churches or agricultural organizations, help raise awareness about the new blood pressure guidelines in culturally relevant ways. By decentralizing care and using technology, rural systems are finding innovative methods to integrate the AHA guidelines for hypertension despite systemic limitations.
8. What are the implications of the new guidelines for pediatric and adolescent populations?
Although the primary focus of the AHA guidelines for hypertension is adult populations, the updated framework has prompted increased attention toward pediatric blood pressure trends. With childhood obesity rates rising, many clinicians are applying elements of the hypertension guidelines in the United States to screen for early signs of vascular risk in adolescents. While formal pediatric thresholds remain distinct, the lower blood pressure cut off for adults signals a need for vigilance in monitoring at-risk youth. School-based health programs and pediatric wellness initiatives are starting to incorporate education on blood pressure, exercise, and nutrition. As awareness grows, future updates may expand guideline htn protocols to explicitly include younger age groups.
9. How might future revisions to hypertension guidelines incorporate personalized medicine?
The future of hypertension guidelines is likely to be shaped by personalized medicine, integrating genetic profiling and biomarker analysis into routine care. Emerging research suggests that individual responses to antihypertensive medications and lifestyle interventions vary significantly, which could redefine the guideline for high blood pressure on a more granular level. Machine learning algorithms are also being developed to predict cardiovascular risk based on a combination of blood pressure data, genomic markers, and social determinants of health. As precision medicine evolves, the classification of high blood pressure will become more individualized, helping clinicians tailor interventions more effectively. This would mark a significant advancement beyond the current population-based AHA definition of hypertension.
10. What public health campaigns are emerging in response to the hypertension guidelines in the United States?
In response to the hypertension guidelines in the United States, a number of public health campaigns have emerged that target both clinicians and the general public. Initiatives like “Know Your Numbers” and “Measure Up/Pressure Down” aim to educate Americans about the importance of monitoring blood pressure and understanding the implications of the new blood pressure guidelines. Community health fairs, pharmacy-based screenings, and mobile wellness units are bringing guideline htn resources to more neighborhoods, particularly in underserved communities. These efforts not only disseminate the AHA definition of hypertension but also equip individuals with tools to make informed health decisions. Through multimedia education and community engagement, these campaigns are helping translate clinical hypertension guidelines into practical, accessible action.
Conclusion: The Evolving Landscape of Hypertension Care and Its Impact on Public Health
The revised hypertension guidelines in the United States represent a landmark moment in cardiovascular medicine. By lowering the blood pressure cut off, redefining hypertension classification, and emphasizing early intervention, the new blood pressure guidelines have shifted the paradigm toward proactive, personalized care. The AHA definition of hypertension now reflects a deeper understanding of cardiovascular risk and the importance of timely action.
For clinicians, these guidelines offer a comprehensive framework for improving diagnosis and treatment, while for patients, they provide a roadmap to better health through lifestyle changes, education, and ongoing monitoring. The integration of technology, attention to health disparities, and focus on evidence-based practice underscore the strength and relevance of the current approach.
As we continue to refine the guideline htn framework and expand its reach, it is essential to remain grounded in the principles of Experience, Expertise, Authoritativeness, and Trustworthiness. These pillars not only enhance the credibility of clinical recommendations but also ensure that patients receive the highest standard of care. The journey toward optimal blood pressure control is ongoing, but with the guidance of thoughtful, scientifically grounded policy, it is one that holds great promise for individuals and communities alike.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Blood pressure and the new ACC/AHA hypertension guidelines
International Society of Hypertension Global Hypertension Practice Guidelines
New ACC/AHA High Blood Pressure Guidelines Lower Definition of Hypertension