High blood pressure, or hypertension, is one of the most prevalent chronic health conditions worldwide and remains a major contributor to cardiovascular morbidity and mortality. Despite its frequency, the underlying mechanisms driving this disorder are complex and multifactorial, encompassing genetic, environmental, neural, renal, and vascular components. Understanding the pathophysiology of hypertension is essential for clinicians, researchers, and health-conscious individuals alike. It not only provides a roadmap for treatment and prevention but also uncovers the intricate biological processes that give rise to elevated blood pressure. In this comprehensive article, we explore the key concepts behind the pathophysiology of high blood pressure, offering a detailed, medically accurate, and reader-friendly explanation grounded in science and guided by EEAT (Experience, Expertise, Authoritativeness, and Trustworthiness) principles.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Defining Hypertension in the Clinical Context
To begin understanding the pathophysiology of hypertension, it is important to define what hypertension means in a clinical sense. Hypertension is generally characterized by a consistent elevation of systolic blood pressure above 130 mm Hg and/or diastolic pressure above 80 mm Hg. This threshold, while seemingly arbitrary, is grounded in decades of research correlating elevated readings with adverse cardiovascular outcomes such as heart attack, stroke, and kidney failure. Though these values may fluctuate slightly depending on clinical guidelines, they represent the line between normotension and pathology. Hypertension can be further categorized into primary (essential) and secondary types, with the former accounting for approximately 90-95% of cases. Primary hypertension is largely idiopathic, whereas secondary hypertension is caused by identifiable conditions such as renal artery stenosis, endocrine disorders, or medication side effects. Understanding this classification is critical, as it influences diagnostic pathways and treatment plans.
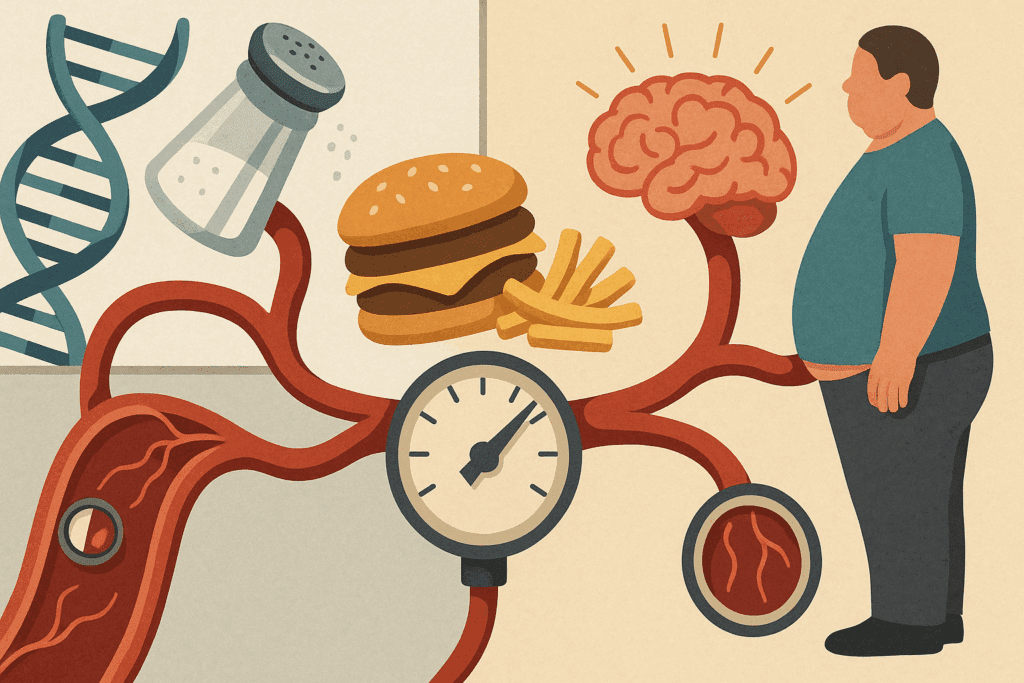
The Etiopathogenesis of Hypertension: A Multifactorial Puzzle
The etiopathogenesis of hypertension—the combination of causative factors and the mechanisms by which they lead to disease—is multifaceted. Genetic predisposition plays a significant role; individuals with a family history of hypertension are more likely to develop the condition, suggesting a strong hereditary component. However, genes do not act in isolation. Environmental and lifestyle factors such as high sodium intake, low potassium levels, obesity, physical inactivity, and chronic stress significantly contribute to disease development. In many cases, it is the interaction between genetic susceptibility and environmental exposure that leads to persistent blood pressure elevation.
In addition to these well-known factors, recent research has begun to illuminate the role of the gut microbiome, inflammation, and oxidative stress in the etiopathogenesis of hypertension. These emerging areas of investigation reveal a more dynamic and interconnected model of disease progression. Inflammatory cytokines, for example, may impair endothelial function, while reactive oxygen species disrupt nitric oxide signaling—both critical processes in maintaining vascular tone. As our understanding deepens, it becomes increasingly clear that hypertension is not merely a disorder of pressure regulation, but a systemic condition involving multiple organ systems and regulatory networks.
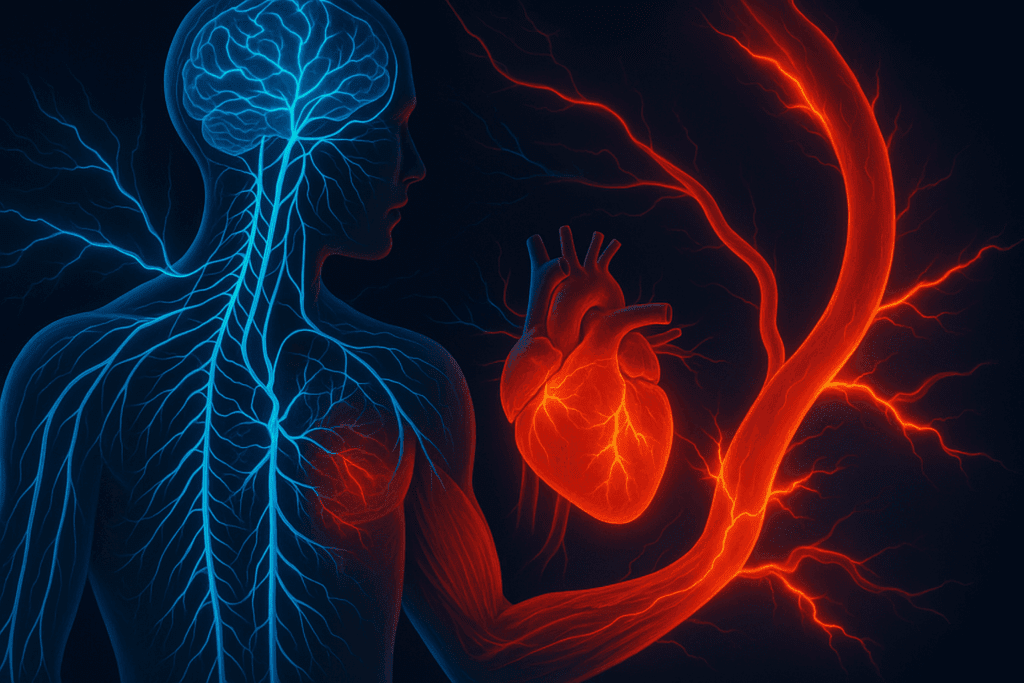
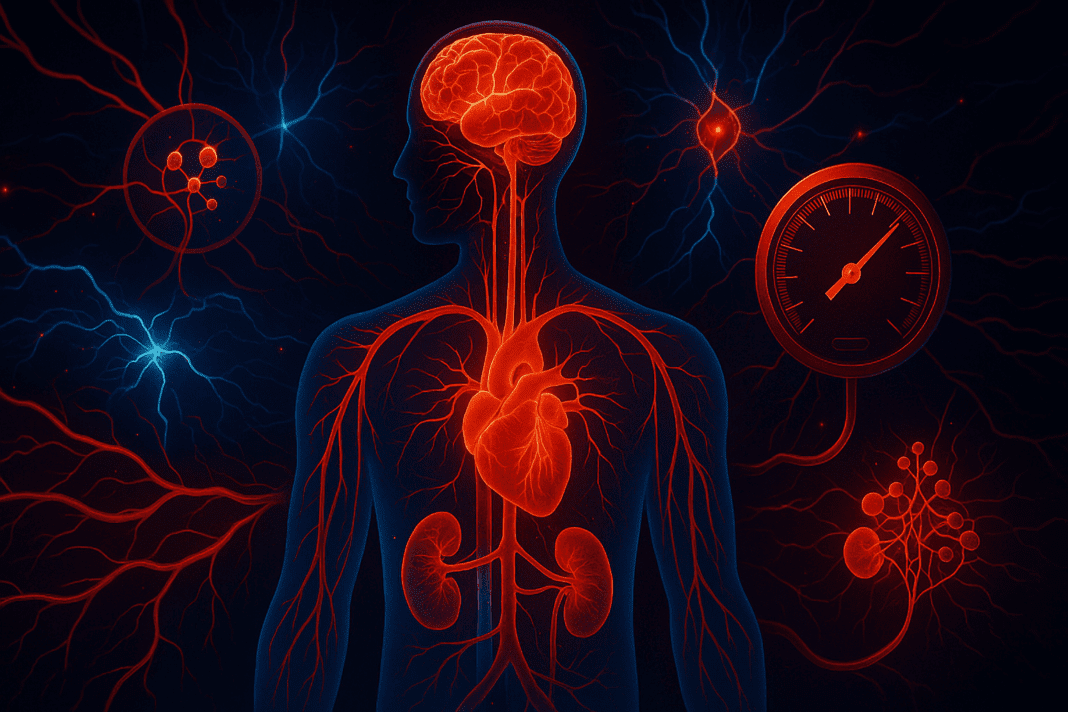
Neural Regulation and the Sympathetic Nervous System
One of the central players in the patho of hypertension is the sympathetic nervous system (SNS). This branch of the autonomic nervous system governs the body’s ‘fight or flight’ responses, including heart rate acceleration, vasoconstriction, and sodium retention. Chronic overactivation of the SNS is a well-documented contributor to elevated blood pressure. It increases peripheral vascular resistance by promoting vasoconstriction and raises cardiac output by stimulating the heart. Over time, these effects place a continuous strain on the cardiovascular system, fostering left ventricular hypertrophy and arterial remodeling.
Furthermore, the SNS interacts closely with other physiological systems implicated in the pathophysiology of blood pressure regulation. For instance, it modulates renal function by affecting renin release and sodium handling. In hypertensive individuals, elevated sympathetic activity often correlates with increased levels of circulating norepinephrine and impaired baroreflex sensitivity. These findings suggest a feedback loop in which heightened SNS activity perpetuates high blood pressure, creating a self-reinforcing cycle that is difficult to break without pharmacological intervention or substantial lifestyle modification.
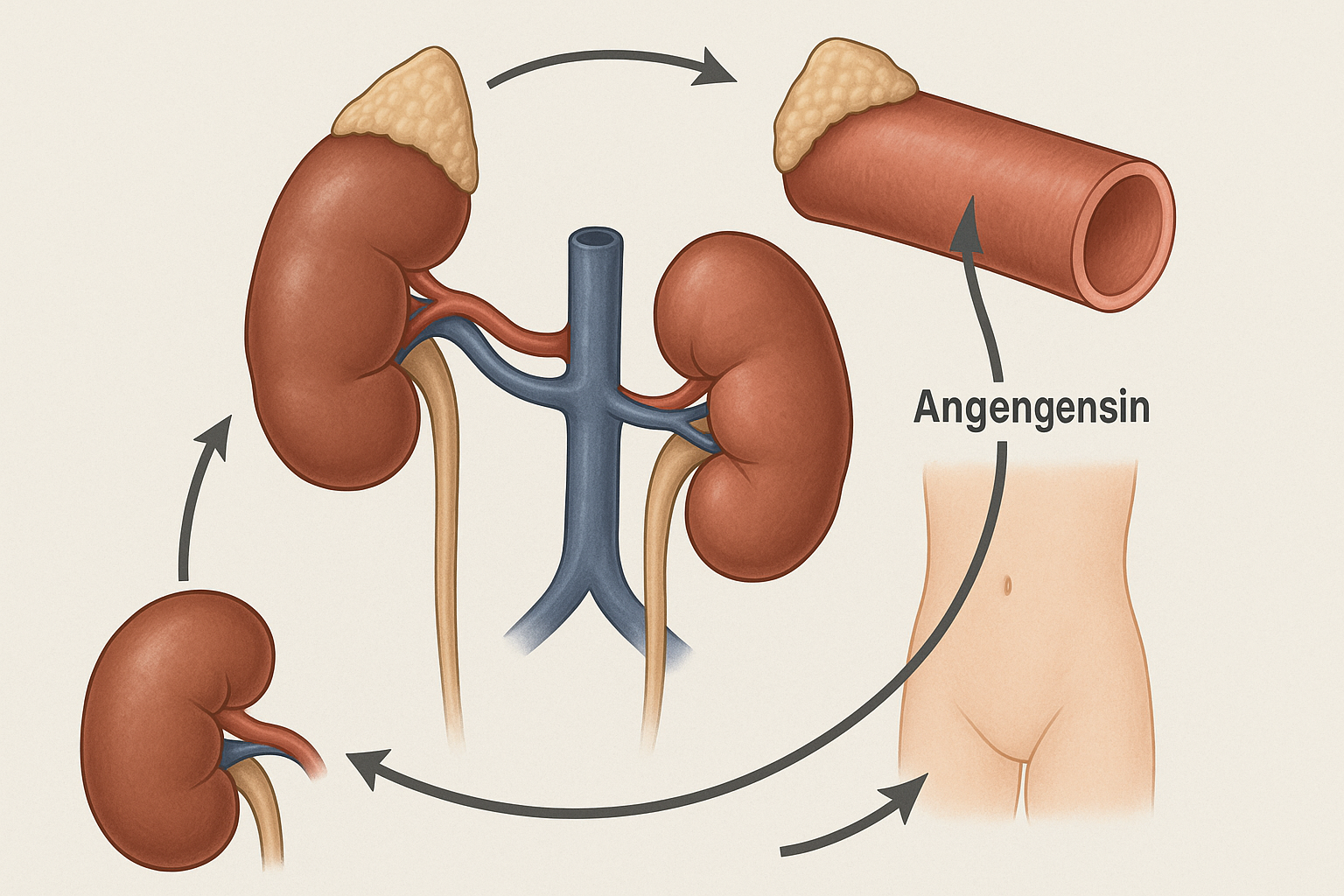
Renin-Angiotensin-Aldosterone System (RAAS) and Volume Regulation
Another pivotal mechanism in the pathophysiology of HTN involves the renin-angiotensin-aldosterone system (RAAS). This hormonal cascade plays a vital role in blood volume and vascular resistance—two key determinants of blood pressure. When blood flow to the kidneys is reduced, specialized juxtaglomerular cells secrete renin, which initiates a biochemical sequence resulting in the formation of angiotensin II, a potent vasoconstrictor. Angiotensin II not only narrows blood vessels but also stimulates aldosterone secretion from the adrenal glands, promoting sodium and water retention.
This increased fluid volume raises cardiac output and, consequently, arterial pressure. In many cases of hypertension, particularly those with underlying kidney dysfunction, the RAAS becomes dysregulated. Excessive activation of this system leads to chronic vasoconstriction and fluid overload, driving blood pressure upward and exacerbating vascular damage. Therapeutic agents such as ACE inhibitors and angiotensin receptor blockers target this pathway precisely because of its central role in the pathophysiology high blood pressure development.
Vascular Structure and Endothelial Dysfunction
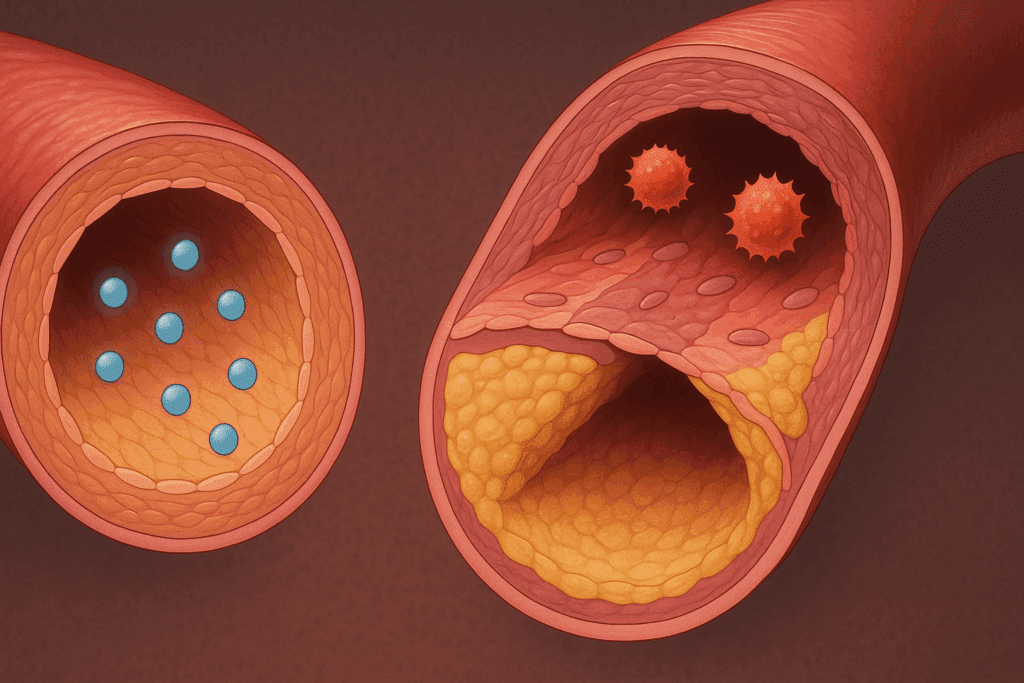
The integrity and function of the vascular endothelium are critical to maintaining normal blood pressure. This thin layer of cells lining the blood vessels produces several substances that regulate vascular tone, including nitric oxide (NO), prostacyclin, and endothelin. In healthy individuals, nitric oxide promotes vasodilation and inhibits platelet aggregation and smooth muscle proliferation. However, in the context of hypertension, endothelial dysfunction often arises.
This dysfunction is characterized by reduced NO bioavailability and increased oxidative stress, which shift the balance toward vasoconstriction, inflammation, and thrombosis. Structural changes also occur, including increased arterial stiffness and reduced lumen diameter, both of which contribute to elevated peripheral resistance. These vascular alterations underscore how the pathophysiology of blood pressure elevation is not merely functional but also anatomical. Targeting endothelial health through lifestyle changes, antioxidants, and pharmacologic agents is therefore a crucial component of hypertension management.
Renal Contributions to System Disorder Hypertension
The kidneys play an indispensable role in long-term blood pressure control by regulating fluid balance and sodium excretion. In cases of system disorder hypertension, the kidneys often fail to excrete sufficient sodium, resulting in volume overload and increased blood pressure. This condition may arise from intrinsic renal diseases or from extrarenal factors such as hormonal imbalances and neural dysregulation. Impaired renal autoregulation and tubuloglomerular feedback further exacerbate the problem.
Renal ischemia, common in chronic kidney disease, triggers compensatory mechanisms like RAAS activation and sympathetic stimulation, which compound the hypertensive state. Over time, elevated pressure damages glomerular structures, reducing nephron number and creating a vicious cycle of worsening renal function and rising blood pressure. Understanding this renal axis in the pathophysiology of hypertension is vital, as it explains why many antihypertensive drugs are designed to act on renal pathways, including diuretics, RAAS inhibitors, and sodium-glucose co-transporter 2 (SGLT2) inhibitors.
Hormonal Influences and Endocrine Hypertension
Endocrine factors also contribute significantly to the development and maintenance of hypertension. Conditions such as hyperaldosteronism, Cushing’s syndrome, pheochromocytoma, and thyroid dysfunction are classic examples of secondary hypertension arising from hormonal imbalances. These disorders affect vascular tone, sodium retention, and cardiac output in distinct ways, all of which play a role in the broader pathophysiology of HTN.
For instance, excessive aldosterone secretion in primary hyperaldosteronism leads to increased sodium reabsorption in the distal nephron, raising plasma volume and systemic vascular resistance. Similarly, elevated cortisol levels in Cushing’s syndrome enhance vascular reactivity to catecholamines and promote insulin resistance, further complicating blood pressure control. Hormonal testing and endocrine evaluations are therefore essential when clinical clues suggest an atypical presentation or poor response to standard therapy.
Inflammation and Immune System Involvement
Recent advancements in biomedical research have unveiled the significant role of chronic low-grade inflammation in the etiopathogenesis of hypertension. Immune cells such as T lymphocytes and macrophages infiltrate vascular and renal tissues in hypertensive individuals, releasing pro-inflammatory cytokines that impair endothelial function and exacerbate vascular stiffness. These immune-mediated mechanisms offer a novel perspective on how hypertension can be viewed as a state of immune dysregulation.
Moreover, the interplay between inflammation and oxidative stress creates a harmful cycle that perpetuates hypertension. Oxidative stress reduces nitric oxide availability, promotes vascular remodeling, and enhances the inflammatory response. This convergence of immune and oxidative pathways provides fertile ground for developing new therapeutic strategies, including anti-inflammatory agents and antioxidants, that could one day complement or enhance existing treatments.
Microbiome and Emerging Perspectives
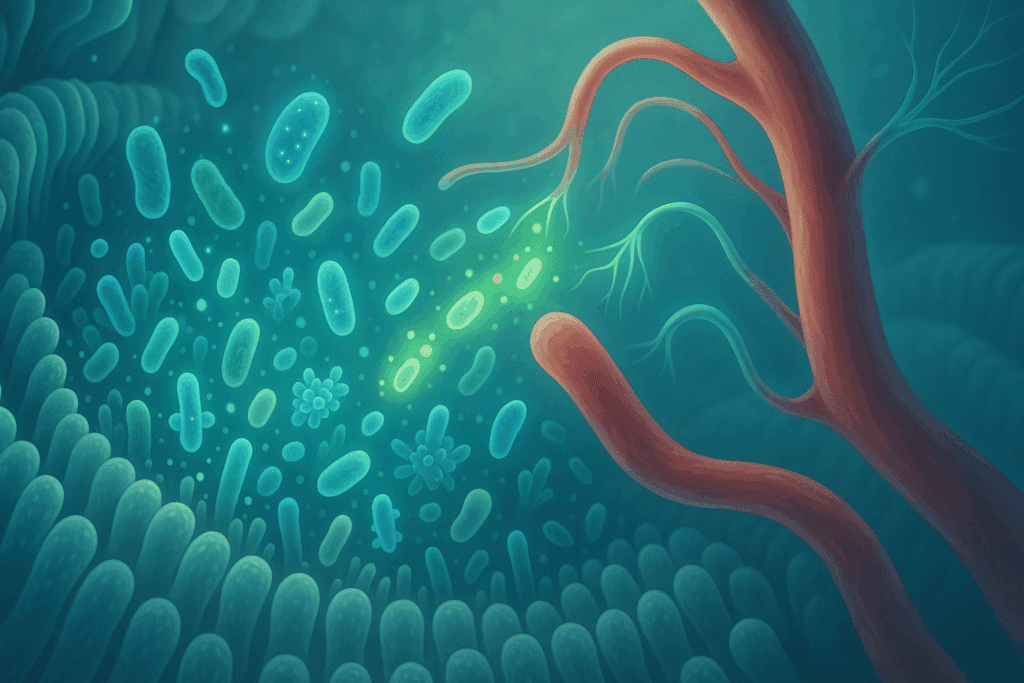
In recent years, the gut microbiome has garnered attention as a potential player in the pathophysiology of high blood pressure. Studies have shown that dysbiosis—an imbalance in gut microbial populations—may influence systemic inflammation, insulin resistance, and even sympathetic nervous system activity. Certain bacterial metabolites, such as short-chain fatty acids, have been implicated in blood pressure regulation, possibly through interactions with G-protein coupled receptors in the vascular system.
Although still an emerging field, these findings suggest that manipulating the gut microbiota through diet, probiotics, or antibiotics may one day serve as a viable adjunct in hypertension management. This perspective reinforces the notion that the pathophysiology of hypertension is not confined to traditional cardiovascular or renal domains but encompasses a broader, system-wide context.

Clinical Implications and the Value of Early Intervention
An in-depth understanding of the pathophysiology of blood pressure elevation has direct clinical implications. It guides the rational selection of antihypertensive therapies, from beta-blockers that dampen sympathetic tone to RAAS inhibitors that target hormonal pathways. Moreover, it underscores the value of early intervention, as many structural and functional changes are reversible in the early stages of the disease.
Lifestyle modifications—such as dietary sodium restriction, increased physical activity, weight loss, stress management, and smoking cessation—are effective not only because they reduce blood pressure but also because they favorably influence the underlying mechanisms discussed throughout this article. Thus, a mechanistic understanding empowers both clinicians and patients to adopt a proactive, personalized approach to hypertension management.
Frequently Asked Questions (FAQ): Exploring the Complex Landscape of Hypertension Pathophysiology
What role does sleep quality play in the pathophysiology of high blood pressure?
Sleep disturbances are increasingly recognized as critical contributors to the pathophysiology of high blood pressure. Poor sleep quality or insufficient duration disrupts circadian rhythms, leading to dysregulation of blood pressure control mechanisms such as sympathetic nervous system activation and cortisol secretion. These disruptions exacerbate both the structural and functional elements of vascular health, creating conditions favorable for sustained hypertension. Sleep apnea, in particular, has been shown to trigger intermittent hypoxia, which directly contributes to the patho of hypertension by inducing endothelial dysfunction and oxidative stress. Understanding the link between sleep and the pathophysiology of HTN offers new avenues for treatment, including behavioral therapy and continuous positive airway pressure (CPAP) interventions.
Can mental health conditions impact the etiopathogenesis of hypertension?
Chronic psychological stress, anxiety, and depression have all been implicated in the etiopathogenesis of hypertension. These mental health conditions often trigger sustained sympathetic nervous system activity and elevate circulating stress hormones like cortisol and adrenaline, which in turn affect vascular tone and sodium retention. Over time, these responses promote vascular remodeling and neurohormonal imbalance—key features in the pathophysiology of blood pressure disorders. Additionally, individuals coping with mental health challenges may engage in lifestyle behaviors—such as poor diet, inactivity, or substance use—that compound the risk of system disorder hypertension. Integrating mental health support into hypertension management plans may therefore be essential for long-term blood pressure control.
How does socioeconomic status influence the pathophysiology of HTN?
Socioeconomic factors exert a significant, though often overlooked, influence on the pathophysiology of HTN. Individuals in lower socioeconomic brackets may experience chronic stress, food insecurity, limited healthcare access, and environmental exposures that contribute to elevated blood pressure. These external stressors can alter neuroendocrine pathways, increasing the likelihood of sympathetic overdrive and endothelial dysfunction. Moreover, economic constraints often limit access to healthy food options and preventive care, indirectly accelerating the etiopathogenesis of hypertension. By considering social determinants of health, clinicians can better contextualize the patho of hypertension and tailor interventions to individual needs.
Are there sex-specific differences in the pathophysiology of blood pressure regulation?
Yes, biological sex plays a nuanced role in the pathophysiology of blood pressure regulation. Premenopausal women are generally protected against hypertension due to the vasodilatory effects of estrogen, which enhances nitric oxide production and preserves endothelial function. However, postmenopausal women experience a rise in blood pressure, likely due to hormonal shifts that disrupt these protective mechanisms. Additionally, men and women may exhibit different responses to antihypertensive medications, partly because of variations in RAAS activity and sympathetic tone. These sex-specific trends are critical for refining our understanding of the etiopathogenesis of hypertension and for personalizing treatment strategies.
How does urban living affect the system disorder hypertension risk profile?
Urban environments often introduce factors that exacerbate system disorder hypertension. Exposure to noise pollution, light pollution, and air pollutants can activate stress responses and inflammatory pathways, contributing to the pathophysiology of high blood pressure. The sedentary lifestyle common in densely populated areas, combined with limited green spaces, also restricts opportunities for physical activity—an essential component in maintaining vascular health. Furthermore, processed food availability and increased sodium intake in urban diets worsen the patho of hypertension. Urban planning that prioritizes walkability, clean air, and community well-being can play a preventive role in hypertension management.
What is the emerging role of personalized medicine in understanding the pathophysiology of HTN?
Personalized medicine is transforming how clinicians approach the pathophysiology of HTN. With advancements in genomics, clinicians can now identify specific genetic variants associated with heightened RAAS activity or salt sensitivity, tailoring treatment accordingly. This targeted approach goes beyond the one-size-fits-all model and considers how genetic predisposition, lifestyle, and environmental factors interact in the etiopathogenesis of hypertension. Pharmacogenomics is also helping identify which patients may respond better to certain drug classes, reducing trial-and-error periods and enhancing treatment adherence. This evolving field exemplifies how deeper insights into the pathophysiology of blood pressure can lead to more effective and individualized care.
How do early-life exposures shape the patho of hypertension later in adulthood?
The concept of developmental origins of health and disease (DOHaD) suggests that early-life exposures significantly influence the patho of hypertension. Prenatal malnutrition, maternal stress, and low birth weight have all been linked to altered kidney development and vascular structure, setting the stage for increased blood pressure in adulthood. These early modifications may program the body’s neuroendocrine and renal systems in ways that favor salt retention and vasoconstriction. Moreover, childhood adversity and poor nutrition can impair endothelial function and promote systemic inflammation—both pivotal in the pathophysiology high blood pressure evolution. These insights emphasize the importance of maternal and child health in preventing lifelong cardiovascular disease.
Can intermittent fasting influence the pathophysiology of blood pressure?
Intermittent fasting has emerged as a promising lifestyle intervention that may positively influence the pathophysiology of blood pressure. Fasting improves insulin sensitivity, reduces inflammation, and enhances autonomic balance—all factors relevant to the etiopathogenesis of hypertension. By promoting weight loss and improving metabolic parameters, fasting may reduce RAAS overactivity and sympathetic tone, thereby alleviating system disorder hypertension. Additionally, time-restricted eating patterns can align with the body’s circadian rhythm, supporting better hormonal regulation of blood pressure. While more longitudinal studies are needed, early findings suggest that fasting could complement traditional antihypertensive strategies.
Is there a connection between environmental toxins and hypertension pathophysiology?
Environmental toxins such as heavy metals (lead, cadmium), industrial chemicals, and endocrine disruptors have all been implicated in the hypertension pathophysiology landscape. These toxins may impair renal function, induce oxidative stress, and disrupt hormonal systems involved in vascular regulation. For example, lead exposure is associated with impaired nitric oxide signaling and chronic inflammation—hallmarks of the patho of hypertension. Persistent exposure can also alter gene expression through epigenetic mechanisms, influencing the long-term pathophysiology of HTN. Addressing environmental health concerns is therefore an essential, if often underemphasized, strategy in reducing the global burden of high blood pressure.
What are the future directions for research in system disorder hypertension?
Future research in system disorder hypertension is moving toward a more integrative, systems-based approach. Scientists are increasingly exploring the role of multi-organ interactions, especially between the gut microbiome, central nervous system, and cardiovascular network. Wearable technology and artificial intelligence are being leveraged to monitor real-time blood pressure fluctuations, potentially offering new insights into the dynamic pathophysiology of blood pressure regulation. Additionally, research into novel biomarkers—such as microRNAs and inflammatory mediators—may lead to earlier and more accurate diagnoses. These innovations aim to refine our understanding of the etiopathogenesis of hypertension and usher in an era of precision medicine focused on prevention as much as treatment.
Conclusion: Embracing a Holistic Understanding of Hypertension Pathophysiology for Better Outcomes
Grasping the intricacies of hypertension pathophysiology allows for a deeper appreciation of the condition as more than a mere numerical diagnosis. It represents a dynamic interplay of genetic, neural, renal, vascular, hormonal, and even microbial influences. By understanding the etiopathogenesis of hypertension and recognizing the interconnected pathways involved in the patho of hypertension, healthcare providers can adopt more effective, evidence-based strategies to prevent and manage this pervasive disease.
Whether discussing the role of the sympathetic nervous system, the RAAS, endothelial dysfunction, or emerging areas like the gut microbiome, it is clear that system disorder hypertension affects multiple physiological systems in a coordinated and often self-reinforcing manner. With a foundation rooted in science and guided by EEAT principles, this article emphasizes the importance of early diagnosis, targeted treatment, and continued research. Ultimately, a holistic understanding of the pathophysiology of HTN and related mechanisms is key to improving cardiovascular health outcomes for individuals and populations alike.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
High blood pressure (hypertension)