Introduction: Why Understanding the Layer Surrounding the Heart Is Essential for Heart Health
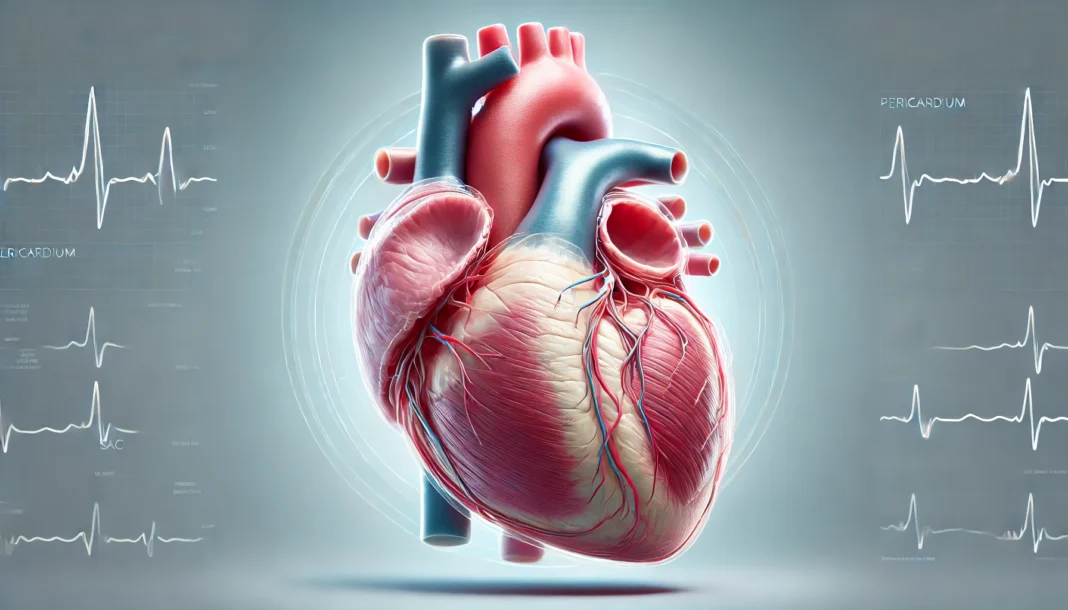
The heart is more than a solitary muscle pumping blood—it is an intricately protected organ, shielded and supported by a specialized anatomical structure known as the pericardium. For anyone seeking to understand cardiovascular function or looking to improve heart health, grasping what is the layer surrounding the heart—and how it contributes to overall well-being—is fundamental. The pericardium is not simply a passive covering. It actively participates in the mechanical and immunological functioning of the heart, ensuring the stability, protection, and optimal performance of one of the body’s most vital organs.
You may also like: 5 Ways to Keep Your Heart Healthy and Prevent Cardiovascular Disease
In modern cardiovascular medicine, conditions involving the pericardium are increasingly recognized for their role in heart disease symptoms and complications. Whether it’s pericarditis, pericardial effusion, or constrictive pericardial disease, dysfunctions of this protective sac can be just as life-threatening as coronary artery blockages. Therefore, understanding the structure, function, and potential pathology of the pericardium is no longer solely the concern of cardiologists—it is valuable knowledge for patients, caregivers, and anyone aiming to preserve cardiovascular health.
In this comprehensive article, we will explore the anatomical and physiological characteristics of the pericardium in detail. We’ll examine the layers of the heart, delve into the specific structures within the pericardial sac, and clarify essential terminology such as the pericardial cavity, visceral pericardium, and fibrous pericardium. By the end, you’ll not only be able to define pericardium but also understand its vital role in safeguarding your heart against mechanical stress, infection, and dysfunction.
What Is the Pericardium and Why Does It Matter?
To define pericardium in its simplest terms, it is a double-walled sac that encloses the heart and the roots of the great vessels. This sac is not just a protective wrapper; it plays several key physiological roles that are critical for healthy cardiovascular function. Structurally, the pericardium serves as the boundary between the heart and surrounding thoracic organs, shielding it from infection and mechanical interference. Functionally, it lubricates the beating heart, prevents overexpansion during diastole, and maintains the heart’s position in the chest cavity.
The pericardium is typically divided into two major components: the fibrous pericardium and the serous pericardium. Together, these form the pericardial sac, a structure whose mechanical resilience and fluid-lubricated surfaces ensure the heart can beat continuously without friction or displacement. If you’ve ever wondered what is a pericardial structure’s role in health and disease, the answer lies in its multitasking capabilities—it acts as both a protector and a facilitator of normal heart function.
Understanding the pericardium also matters because conditions affecting it can have serious consequences. For instance, pericardial effusion—a buildup of fluid in the pericardial cavity—can impede the heart’s ability to fill and contract, leading to cardiac tamponade, a life-threatening emergency. Thus, the pericardium is far more than an anatomical afterthought; it is an essential element of the cardiovascular system with direct implications for survival and health.
The Layers of the Heart: More Than Just Muscle
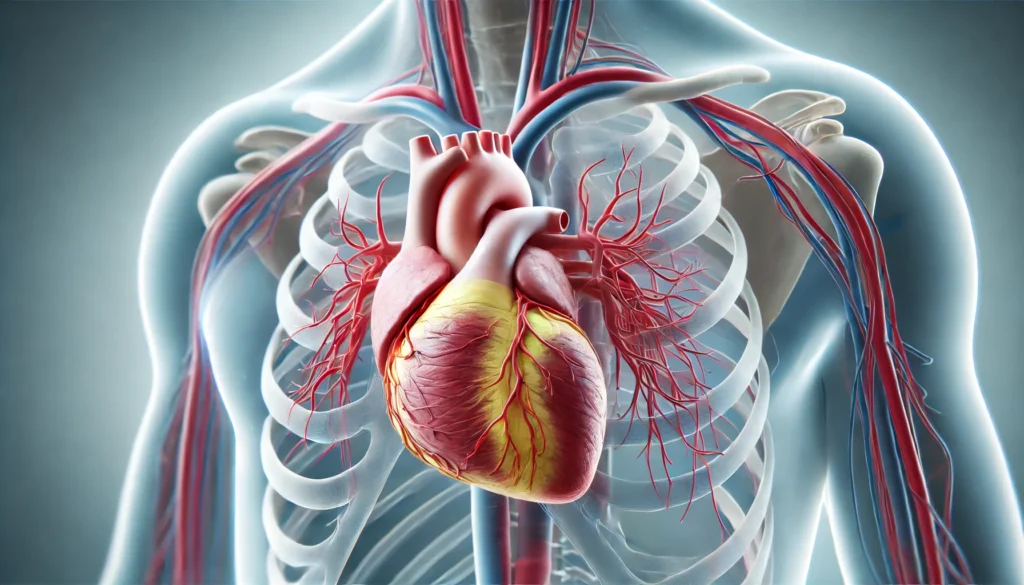
Many assume the heart is simply a muscular pump, but it actually consists of multiple distinct layers, each with specific structural and functional roles. These layers of the heart are typically classified into three: the endocardium, myocardium, and epicardium. These are sometimes collectively referred to as the heart’s three layers, and each contributes to the organ’s resilience and performance.
The innermost layer, known as the endocardium, is a smooth, thin membrane that lines the interior of the heart chambers. It also includes the valves and plays a role in reducing turbulence during blood flow. The endocardium is often referred to as the inner lining of the heart, and its integrity is crucial in preventing conditions like infective endocarditis.
The middle layer, the myocardium, is the muscular tissue responsible for the contraction of the heart. It’s the thickest and most mechanically active layer, composed of specialized cardiac muscle fibers. Much of the heart’s electrical activity and pumping force originate in the myocardium, and any damage to this layer—such as from a heart attack—can significantly impair cardiovascular performance.
The outermost layer, called the epicardium, is actually synonymous with the visceral pericardium, one of the two layers of the serous pericardium. This highlights a fascinating overlap between the pericardium and the heart’s structural layers. In fact, the visceral pericardium is the part of the pericardium attached directly to the myocardium, forming a smooth surface that is in intimate contact with the cardiac muscle. When asking which part is attached to the myocardium from pericardium, the answer is unequivocally the visceral layer.
Exploring the Pericardium Layers: Fibrous and Serous Components
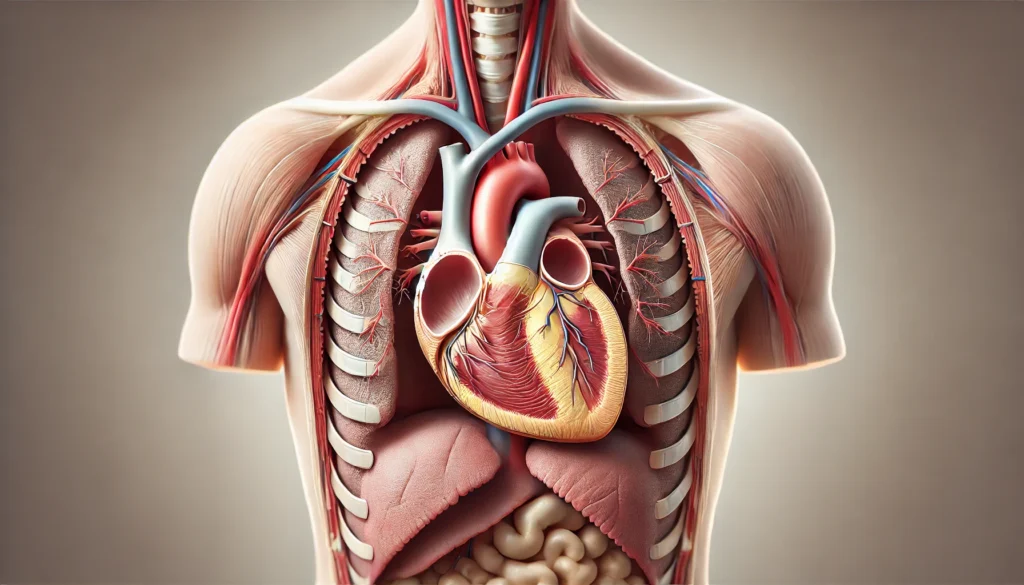
The pericardium layers can be classified into the fibrous pericardium and the serous pericardium, each with unique anatomical characteristics and functions. The fibrous pericardium is the outermost layer. It is composed of dense, irregular connective tissue and serves as a robust barrier that protects the heart from physical trauma and overdistension. This layer anchors the heart to surrounding structures such as the diaphragm, sternum, and great vessels, ensuring that the heart maintains its central position in the thoracic cavity.
Inside the fibrous pericardium lies the serous pericardium, which is itself subdivided into two layers: the parietal pericardium and the visceral pericardium. These two thin but essential membranes create the pericardial cavity between them. This cavity is filled with a small volume of lubricating fluid—typically 15 to 50 milliliters in healthy individuals—that reduces friction as the heart beats and shifts.
The parietal pericardium lines the inner surface of the fibrous sac, while the visceral pericardium is directly adherent to the heart’s surface. Collectively, these structures ensure that the heart remains well-positioned, protected, and able to function without irritation. The pericardial sac, which encompasses all these components, is thus a critical structure whose integrity is vital to cardiovascular health. When considering what membrane lines the heart cavity and facilitates smooth contraction, the serous pericardial layers and their intervening cavity are the answer.
Understanding the Pericardial Cavity: A Lubricated Space for Cardiac Motion
The pericardial cavity is more than just a space; it is a functional anatomical zone essential for the unhindered movement of the heart. Located between the parietal and visceral layers of the serous pericardium, this cavity contains serous fluid that acts as a lubricant. This prevents the friction that would otherwise occur with every heartbeat—an estimated 100,000 times per day.
This lubrication is crucial during dynamic cardiovascular changes, especially during strenuous physical activity when the heart must beat faster and harder. Without a properly functioning pericardial cavity, the mechanical friction between heart tissues could lead to inflammation or even mechanical injury. Furthermore, the tightly regulated volume of pericardial fluid ensures that the heart is cushioned but not compressed. Any significant deviation from this fluid balance, such as in pericardial effusion, can result in pathological conditions that restrict cardiac filling and output.
Clinically, the pericardial cavity becomes a focus of concern in inflammatory conditions like pericarditis or in fluid accumulation from infections, trauma, or cancer. This makes awareness of what is a pericardial cavity and how it functions not just an academic exercise but a practical necessity in diagnosing and managing cardiovascular diseases. In this sense, the pericardial cavity acts as both a buffer and a warning system—when compromised, it signals deeper problems within the heart or the body.
The Function of the Pericardium in Cardiovascular Health
The pericardium function is multifaceted, encompassing mechanical, immunological, and physiological roles. Mechanically, it acts as a shock absorber, protecting the heart from external trauma. It also stabilizes the heart’s position, preventing torsional or excessive movement during vigorous physical activity. Physiologically, it provides a lubricated environment, thanks to the pericardial cavity, and facilitates pressure equalization between the heart chambers.
In addition to its mechanical support, the pericardium serves an important role in immune defense. It forms a barrier that limits the spread of infection from surrounding organs, such as the lungs or esophagus, to the heart. Moreover, the pericardial fluid contains immune cells and proteins that help identify and neutralize pathogens, reducing the risk of infectious pericarditis.
The pericardium also plays a role in cardiac mechanics by preventing overdistension. When venous return increases during exercise or volume overload, the pericardial sac prevents the ventricles from expanding beyond safe limits. This intrinsic regulation helps maintain cardiac efficiency and prevents dilation-related pathologies. Therefore, the pericardium layers contribute not only to structural integrity but also to dynamic cardiovascular adaptation, underscoring their essential role in heart health.
Pericardial Disorders: When the Heart’s Shield Becomes a Source of Disease
Although the pericardium is a protective structure, it is not immune to disease. Disorders of the pericardium can result in severe and often life-threatening conditions. Pericarditis, for example, is an inflammatory disease of the pericardium that causes sharp chest pain, often mistaken for a heart attack. It may be viral, bacterial, autoimmune, or idiopathic in origin. The inflammation leads to increased fluid production, which may result in pericardial effusion.
Pericardial effusion itself is a condition where excess fluid accumulates in the pericardial cavity. This can escalate into cardiac tamponade—a critical state where the heart is compressed by the fluid, impairing its ability to pump effectively. Surgical drainage or pericardiocentesis is often required to relieve the pressure and restore function.
Another serious condition is constrictive pericarditis, where the pericardial sac becomes thickened and scarred, losing its elasticity. This prevents the heart from expanding properly, leading to symptoms of heart failure such as fatigue, swelling, and shortness of breath. Understanding the pericardial sac and how it can become pathologically rigid helps clinicians identify and treat this uncommon but serious disorder.
Diagnostic Approaches and Imaging of the Pericardium
Diagnosing pericardial disease requires a detailed understanding of cardiac anatomy and the use of advanced imaging techniques. Echocardiography remains the first-line modality for assessing pericardial effusion and tamponade. It provides real-time visualization of the heart chambers, pericardial cavity, and fluid dynamics.
Computed tomography (CT) and magnetic resonance imaging (MRI) offer more detailed views of the pericardium layers, particularly in cases of suspected constrictive pericarditis or malignancy. These modalities can visualize the thickness of the fibrous pericardium, the presence of calcifications, or pericardial masses that may not be evident on echocardiography.
In certain cases, pericardial biopsy or fluid analysis may be necessary to identify infectious or malignant etiologies. Understanding what membrane lines the heart cavity and how to image it accurately is essential for differential diagnosis and treatment planning. In this regard, cardiologists, radiologists, and cardiovascular surgeons must all be fluent in the anatomy and pathology of the pericardium to ensure accurate diagnosis and optimal outcomes.
Frequently Asked Questions (FAQ): Understanding the Pericardium and the Layers of the Heart
1. Can changes in altitude or pressure affect the pericardial cavity and overall heart function?
Yes, sudden changes in altitude or atmospheric pressure can influence the pericardial cavity, particularly in individuals with preexisting pericardial or cardiac conditions. The pericardial cavity, which exists between the visceral pericardium and parietal pericardium, maintains a specific fluid pressure that supports frictionless cardiac motion. When environmental pressure changes rapidly—such as during high-altitude ascents or deep-sea dives—the fluid dynamics within the pericardial sac may be disrupted, occasionally leading to symptoms like chest tightness or shortness of breath. While healthy individuals typically adapt well to such changes, those with compromised pericardium function, such as in constrictive pericarditis, may experience exacerbated symptoms. Therefore, patients with known heart pericardium issues are often advised to consult their physician before engaging in high-pressure activities.
2. How does the pericardium interact with the immune system during cardiac infections?
The pericardium layers play a surprisingly active role in immune surveillance and inflammatory response during cardiac infections. When pathogens enter the bloodstream or migrate from nearby organs, the pericardial sac can act as an immunological barrier, limiting the spread to the inner lining of the heart. Moreover, the fibrous pericardium contains lymphatic vessels and immune cells capable of initiating localized responses. In cases of viral pericarditis, the pericardial cavity may become inflamed, producing excess fluid and triggering fever and chest pain. As research continues, scientists are exploring how immune modulation in the pericardium could help mitigate broader systemic inflammation in heart disease.
3. Are there surgical interventions that specifically target the pericardium without affecting the heart muscle?
Yes, there are several surgical approaches that involve the pericardium but spare the heart muscle itself. One such procedure is pericardiectomy, which involves the partial or complete removal of the fibrous pericardium to relieve constriction in cases of chronic pericarditis. Surgeons must carefully navigate the pericardium layers to avoid damage to the underlying myocardium. These procedures are guided by precise imaging to preserve the visceral pericardium, which part is attached to the myocardium from pericardium and is critical for maintaining epicardial integrity. In some cases, pericardial window procedures are performed to drain excess fluid from the pericardial cavity, alleviating pressure without compromising the 3 layers of the heart.
4. Can lifestyle changes improve the resilience of the pericardium and associated structures?
While the pericardium is not typically the direct target of lifestyle interventions, healthy habits can indirectly support its function and reduce the risk of related disorders. Diets rich in anti-inflammatory nutrients, such as omega-3 fatty acids, have been shown to reduce systemic inflammation that could compromise pericardium layers. Regular cardiovascular exercise improves thoracic muscle tone, which may reduce external strain on the pericardial sac and enhance lymphatic drainage from the pericardial cavity. Additionally, stress-reduction practices like yoga and meditation can positively impact autonomic regulation, indirectly benefiting the heart pericardium and its surrounding structures. Though the pericardium isn’t often mentioned in wellness regimens, these practices offer protective effects.
5. How does aging affect the structure and function of the pericardial sac?
As individuals age, the pericardial sac may undergo structural and functional changes that can subtly impact cardiac performance. The fibrous pericardium often becomes stiffer with age, reducing its elasticity and ability to buffer volume fluctuations in the heart. Similarly, the pericardial cavity may exhibit changes in fluid composition or volume regulation, sometimes contributing to minor forms of pericardial effusion. The visceral pericardium can also accumulate fibrotic tissue, increasing the risk of adhesions to the myocardium. These age-related modifications to the pericardium function can diminish cardiac resilience during stress or illness, making cardiovascular health maintenance especially important in older adults.
6. What are the implications of congenital abnormalities in the pericardium?
Congenital defects in the pericardium are rare but clinically significant when present. Conditions such as congenital absence of the pericardial sac or incomplete formation of the parietal pericardium can lead to abnormal heart positioning or excessive cardiac motion. These anomalies may not affect the inner lining of the heart directly, but they can distort the spatial relationships between the layers of the heart and surrounding thoracic structures. In extreme cases, absence of the pericardium layers can result in herniation of the heart through the pericardial opening, which poses life-threatening risks. Early detection through imaging and surgical intervention is often essential to prevent long-term complications.
7. How do pericardial disorders impact diagnostic imaging and cardiac interpretation?
The presence of pericardial abnormalities can complicate the interpretation of diagnostic imaging. For instance, pericardial effusion in the pericardial cavity may obscure echocardiographic windows or mimic other thoracic masses. Similarly, calcifications within the fibrous pericardium may be misread as myocardial pathology unless carefully distinguished by computed tomography or magnetic resonance imaging. Understanding the anatomical layout of the pericardium layers is crucial in distinguishing true myocardial disease from pericardial conditions. Cardiologists trained to define pericardium boundaries during imaging can more accurately assess abnormalities that affect the 3 layers of the heart.
8. In what ways do autoimmune diseases target the heart pericardium?
Autoimmune diseases like systemic lupus erythematosus and rheumatoid arthritis frequently involve the pericardium as part of a larger inflammatory process. These conditions may provoke inflammation of both the parietal pericardium and visceral pericardium, leading to recurrent pericarditis. When the immune system erroneously attacks the pericardium layers, it may result in persistent chest pain, fluid buildup in the pericardial cavity, or fibrotic thickening. Over time, repeated inflammatory cycles can lead to scarring of the pericardial sac, potentially impairing its protective function. Immunosuppressive therapy is often required to preserve pericardium function and prevent irreversible damage to the heart three layers.
9. How do modern imaging techniques distinguish between the layers of the heart and the pericardium?
Advances in imaging technology now allow clinicians to distinguish the layers of the heart from the surrounding pericardium with exceptional precision. High-resolution cardiac MRI can differentiate the endocardium, myocardium, and epicardium, which collectively make up the heart three layers. It also identifies inflammation or thickening in the parietal pericardium or fibrous pericardium. Ultrasound contrast agents and Doppler techniques can further delineate the dynamic relationship between pericardium layers and cardiac function. This ability to map what membrane lines the heart cavity and detect variations in pericardial composition has revolutionized the early diagnosis and management of heart disease.
10. What are emerging research areas involving the pericardium and cardiovascular therapy?
Cutting-edge research is exploring how the pericardium might serve as a delivery route for targeted cardiovascular therapies. For instance, scientists are investigating whether gene-editing tools or anti-inflammatory agents can be administered directly into the pericardial cavity for localized treatment. This approach could minimize systemic side effects while enhancing therapeutic impact on the visceral pericardium and surrounding heart structures. Additionally, regenerative medicine is looking at how engineered pericardium layers might be used to repair damaged regions of the pericardial sac or even interface with bioartificial hearts. These developments highlight the evolving understanding of what is the layer surrounding the heart—not just as anatomy, but as a frontier for innovation in cardiac care.
Conclusion: The Heart Pericardium—A Vital Yet Underappreciated Shield of Cardiac Health
In the vast and complex world of cardiovascular anatomy, the pericardium often escapes notice. Yet, as we’ve explored in depth, this structure plays an indispensable role in maintaining the heart’s form and function. From the fibrous pericardium that anchors the heart in place to the delicate visceral and parietal pericardium layers that create the pericardial cavity, each element of this protective envelope is finely tuned for performance and protection.
Understanding what is the layer surrounding the heart is not simply a matter of academic interest. It has practical, even lifesaving implications in the detection, diagnosis, and treatment of a wide range of cardiovascular conditions. The heart three layers—including the inner lining of the heart, the muscular myocardium, and the epicardial covering—work in concert with the pericardium to ensure that every beat of the heart is both powerful and protected.
As awareness grows about the pericardium function and its importance, so too does the potential for earlier diagnosis and more effective treatment of pericardial disorders. Whether you are a medical professional, a student, or a patient trying to understand your diagnosis, recognizing the role of the pericardium is essential for grasping the full picture of cardiovascular health. This knowledge not only enriches our understanding of human anatomy but empowers us to better protect the vital rhythm of life.
cardiac anatomy, heart lining structure, epicardial tissue, pericardial inflammation, cardiac membrane layers, heart sac diseases, thoracic cavity protection, cardiovascular physiology, myocardial support structures, cardiac friction reduction, immune response in heart, fluid dynamics of the heart, chronic pericarditis management, cardiac imaging techniques, cardiovascular immune defense, thoracic organ relationships, heart health and aging, cardiac diagnostic innovation, localized heart therapies, autoimmune heart conditions
Further Reading:
What to Know About Pericardial Effusion
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.