Sleep is one of the most fundamental biological processes required for physical and mental restoration. For millions of adults, however, a full night’s sleep is disrupted by a recurring and perplexing problem: waking up every 2 hours. This pattern of sleep interruption not only diminishes the restorative power of slumber but also signals potential underlying health concerns that merit careful attention. While occasional awakenings are common and not necessarily cause for concern, persistent and patterned sleep fragmentation can significantly impair quality of life, leading to fatigue, cognitive decline, emotional instability, and increased risk of chronic disease. Understanding why this phenomenon occurs, its physiological underpinnings, and the steps one can take to regain continuous, restorative rest is essential for improving sleep health.
You may also like: 12 Critical Signs to Watch For: How to Know If You Have Sleep Insomnia and What to Do Next
Understanding Normal Sleep Architecture
To grasp why waking up every 2 hours is problematic, it is first necessary to understand what constitutes normal sleep. Sleep consists of multiple cycles, each typically lasting around 90 to 120 minutes, and moving through stages of non-REM (rapid eye movement) and REM sleep. Non-REM stages include light sleep (stage 1 and 2) and deep sleep (stage 3), also known as slow-wave sleep, which is critical for physical recovery. REM sleep, by contrast, is associated with dreaming and plays a vital role in memory consolidation and emotional regulation.
Healthy adults experience four to six of these cycles each night, ideally without prolonged awakenings. Brief arousals at the end of a cycle are normal and often go unnoticed. However, when individuals wake up every 2 hours consistently and find themselves alert or unable to fall back asleep, this indicates a disruption in the natural progression of sleep architecture. These awakenings may coincide with transitions between cycles, but when they become habitual or distressing, they point to underlying issues.
Common Causes of Sleep Fragmentation in Adults
There are a multitude of factors that can contribute to adults waking up every 2 hours, ranging from lifestyle habits and environmental disturbances to medical and psychological conditions. One of the most common culprits is sleep maintenance insomnia, often referred to as middle insomnia or middle of the night insomnia. Unlike sleep onset insomnia, where falling asleep is the primary issue, sleep maintenance insomnia involves waking up during the night and being unable to return to sleep.
Stress and anxiety play a significant role in this pattern. When the brain remains in a hyperaroused state, the natural ebb and flow of sleep can be easily interrupted. Additionally, fluctuations in hormones such as cortisol and melatonin can exacerbate the issue, particularly in individuals who are chronically stressed or experiencing hormonal transitions such as menopause.
Sleep apnea is another major cause of constant waking up during the night. Obstructive sleep apnea involves repeated episodes where the airway becomes partially or completely blocked, reducing oxygen levels and prompting micro-awakenings to restore airflow. Although many people with sleep apnea are unaware of these awakenings, the disruption to deep sleep and REM stages leads to significant daytime sleepiness and other health complications.
Medical conditions such as acid reflux, chronic pain, and restless leg syndrome can also cause people to wake up every 2 hours. Even mild discomfort or positional changes due to pain can trigger a return to lighter stages of sleep or full arousal. Furthermore, environmental factors such as noise, light exposure, and room temperature fluctuations can create fragmented sleep, particularly in individuals who are already vulnerable to disturbances.
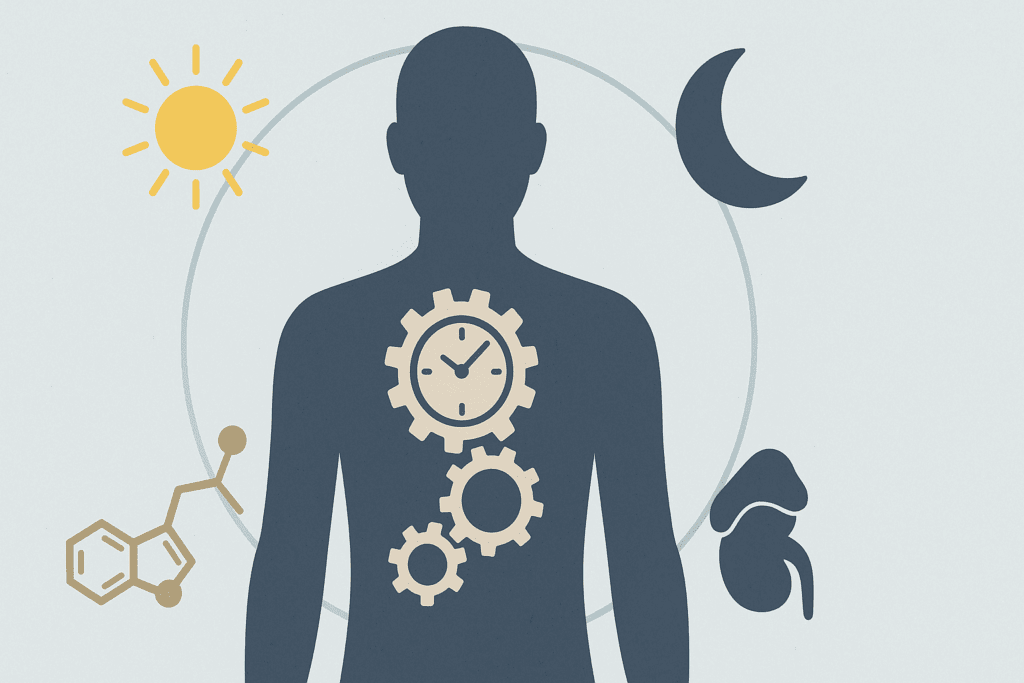
The Role of Circadian Rhythms and Hormonal Cycles
Our internal biological clock, or circadian rhythm, orchestrates a multitude of physiological processes, including the sleep-wake cycle. Disruption to circadian rhythms, whether due to irregular sleep schedules, shift work, or excessive screen exposure before bed, can lead to waking up in the middle of the night. For example, melatonin production typically increases in the evening and promotes sleep onset, while cortisol peaks in the early morning to prepare the body for wakefulness.
When this natural rhythm is altered, such as by artificial light exposure that suppresses melatonin or by stress that elevates nighttime cortisol, the body may misfire its sleep signals. The result can be waking up at 3am or at regular intervals throughout the night. This misalignment not only interferes with the quality of sleep but can create a self-perpetuating cycle where the body becomes conditioned to waking at certain times.
In women, hormonal changes during menstruation, pregnancy, and menopause can significantly impact sleep maintenance. For instance, declines in progesterone during perimenopause can reduce the depth of sleep and increase vulnerability to arousals. Hot flashes and night sweats further compound this effect, making it challenging to achieve uninterrupted rest.
Psychological Factors: Anxiety, Depression, and Cognitive Hyperarousal
Emotional health is deeply intertwined with sleep. Individuals experiencing depression often report waking up early in the morning and being unable to return to sleep. This form of early morning awakening is particularly common in melancholic depression and is often resistant to behavioral interventions without concurrent treatment of the mood disorder itself.
Anxiety, on the other hand, tends to manifest as racing thoughts, a heightened sense of vigilance, and physiological arousal that makes it difficult to stay asleep. The body’s fight-or-flight system, designed for survival in times of threat, becomes chronically activated in anxiety disorders. This heightened state of awareness means that even minor stimuli—a creaking floorboard or a slight shift in body position—can lead to full wakefulness. Over time, the brain becomes conditioned to anticipate these awakenings, reinforcing the cycle of sleep fragmentation.
Cognitive hyperarousal also plays a significant role in why people can’t fall back asleep after waking up. Individuals may find themselves lying awake with thoughts racing about work, family responsibilities, or existential concerns. The bedroom, meant to be a sanctuary for rest, becomes a place of mental turmoil. This association between the bed and wakefulness perpetuates sleep maintenance insomnia, making behavioral interventions essential for breaking the cycle.
Waking Up Every 2 Hours: When It Signals a Sleep Disorder
While occasional nighttime awakenings are common, regularly waking up every 2 hours may indicate a diagnosable sleep disorder. Chronic sleep maintenance insomnia, as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), involves difficulty staying asleep for at least three nights per week over a period of three months, with associated distress or impairment in daily functioning.
Sleep apnea, particularly in its milder forms, can go undiagnosed for years. Individuals may simply attribute their fatigue to stress or age, unaware that they are experiencing dozens or even hundreds of micro-arousals each night. A sleep study (polysomnography) is often necessary to diagnose obstructive or central sleep apnea, both of which require targeted interventions ranging from continuous positive airway pressure (CPAP) therapy to positional therapy and weight management.
Another condition to consider is periodic limb movement disorder (PLMD), characterized by involuntary leg movements during sleep that can lead to arousals. Unlike restless leg syndrome, which occurs when awake, PLMD happens during sleep and may be reported by bed partners rather than recognized by the individual. Similarly, circadian rhythm sleep-wake disorders, such as advanced sleep phase disorder, can lead to waking up during the night and an inability to return to sleep.
Why Do I Keep Waking Up at 3am? The Mystery of the Witching Hour
Among those experiencing fragmented sleep, many report waking up at the same time every night, often around 3am. This pattern can be particularly distressing, leading individuals to question why they keep waking up at 3am and whether it signifies a deeper problem. From a physiological perspective, 3am often coincides with the end of the second or third sleep cycle, a time when REM sleep is more prominent. Because REM is a lighter stage of sleep, it is more susceptible to interruption.
Cortisol levels also begin to rise during this period, preparing the body for the coming day. In individuals with elevated baseline stress or dysregulated cortisol rhythms, this increase can trigger awakening. Additionally, low blood sugar levels may play a role, especially in individuals with metabolic disorders or those who eat dinner early and do not snack before bed. A drop in glucose can activate the sympathetic nervous system, leading to waking up wide awake at night and feeling hungry or anxious.
Spiritual or cultural interpretations of the 3am awakening have persisted for centuries, often referred to as the “witching hour.” While these interpretations can offer comfort or a sense of meaning, it is essential to also evaluate physiological, psychological, and behavioral factors that may be contributing to the phenomenon.
What To Do When You Can’t Fall Back Asleep
One of the most frustrating experiences for those with middle insomnia is waking during the night and being unable to return to sleep. This often leads to clock-watching, increased frustration, and heightened physiological arousal—all of which make sleep even more elusive. Sleep experts recommend a technique called stimulus control, which involves getting out of bed if unable to fall back asleep within 20 minutes. Engaging in a quiet, non-stimulating activity such as reading under dim light can help reset the brain’s association between the bed and wakefulness.
It is also important to avoid screens during this time. The blue light emitted from phones and tablets suppresses melatonin production, further delaying the return to sleep. Deep breathing exercises, progressive muscle relaxation, and mindfulness techniques can help calm the nervous system and promote drowsiness. Avoiding ruminative thinking by shifting attention to neutral imagery or repeating a calming phrase can also be effective.
For some individuals, cognitive behavioral therapy for insomnia (CBT-I) offers a long-term solution. This evidence-based approach addresses the thoughts and behaviors that perpetuate insomnia and has been shown to be more effective than medication in many cases. CBT-I typically involves sleep restriction, cognitive restructuring, and the development of healthy sleep habits, all aimed at consolidating sleep and reducing nighttime awakenings.
Medical Treatments and Professional Help for Waking Up During the Night
When behavioral interventions are not sufficient, medical treatment may be necessary. Sleep specialists can conduct assessments to determine whether conditions such as sleep apnea, PLMD, or circadian rhythm disorders are present. In some cases, medications may be prescribed to help sleeping through the night, though these are typically used as a short-term measure.
Non-benzodiazepine sleep aids such as zolpidem (Ambien) or eszopiclone (Lunesta) may be recommended for sleep maintenance insomnia. However, these medications carry risks of dependence, next-day drowsiness, and cognitive side effects, particularly in older adults. Melatonin supplements can be helpful for circadian rhythm misalignment, but should be used judiciously and under medical supervision.
Emerging therapies such as chronotherapy (gradually adjusting sleep times) and bright light therapy are gaining traction in the treatment of circadian rhythm disorders. These approaches can help realign the body’s internal clock and reduce instances of waking up in the middle of the night. Additionally, addressing comorbid conditions such as depression, anxiety, or chronic pain is essential, as these often exacerbate sleep disturbances.
Lifestyle Adjustments to Support Uninterrupted Sleep
Small changes in lifestyle can have a profound impact on sleep continuity. Establishing a consistent bedtime and wake time, even on weekends, reinforces circadian rhythms and improves sleep quality. Limiting caffeine and alcohol intake—particularly in the hours leading up to bedtime—is critical, as both substances can interfere with sleep architecture and promote nighttime awakenings.
Creating an optimal sleep environment is equally important. This includes keeping the bedroom cool, dark, and quiet, and removing electronic devices that emit light or noise. Investing in a comfortable mattress and pillows that support proper alignment can also reduce physical discomfort that may cause awakening. Practicing a calming bedtime routine, such as taking a warm bath, reading a book, or engaging in gentle stretching, helps signal to the body that it is time to wind down.
For those who frequently wake up every 2 hours, it may be helpful to keep a sleep diary to identify patterns and triggers. Recording factors such as bedtime, wake times, food intake, mood, and exercise can reveal correlations that inform treatment strategies. Over time, these insights can guide personalized interventions that address the root cause of sleep fragmentation.
Why Do I Wake Up Middle of the Night? A Holistic Perspective
Answering the question of why one wakes up in the middle of the night requires a holistic perspective that considers biological, psychological, environmental, and lifestyle factors. Rather than attributing sleep disturbances to a single cause, it is more accurate to view them as the result of a confluence of influences that interact in complex ways. Addressing these requires a multidimensional approach that may involve medical evaluation, psychological support, behavioral modification, and environmental optimization.
Ultimately, restoring restful sleep is not just about avoiding awakenings but about nurturing the conditions that allow the brain and body to move through sleep stages naturally and uninterrupted. When approached with curiosity, patience, and support from knowledgeable professionals, even long-standing sleep difficulties can be improved.
Frequently Asked Questions (FAQ) on Disrupted Sleep and Nighttime Awakenings
How can I retrain my brain if I keep waking up every 2 hours?
Retraining your brain to sleep through the night requires a strategic approach that emphasizes consistency, cognitive rewiring, and environmental conditioning. Begin by establishing a non-negotiable sleep and wake time, even on weekends, to reinforce circadian rhythm stability. If you’re waking up every 2 hours, your brain may have developed a conditioned arousal pattern tied to those intervals. To interrupt this cycle, avoid checking the clock when you awaken and instead practice relaxation techniques like breathwork or guided imagery immediately. Over time, pairing bedtime with calming activities and limiting mental stimulation in the hour before sleep can gradually shift your brain’s association with the bedroom from one of alertness to restfulness.
What are lesser-known lifestyle triggers for waking up in the middle of the night?
While obvious culprits such as caffeine and noise are commonly addressed, subtle factors often go overlooked. For example, consuming high-sodium foods late in the evening can lead to dehydration, prompting nocturnal thirst or urination. Similarly, using certain medications like beta-blockers or antidepressants may interfere with REM sleep, causing fragmented sleep patterns. Overexposure to LED lighting during the day can also dampen melatonin production at night, subtly disrupting sleep architecture. Another trigger is emotional processing: high emotional intensity in the evening—even from a dramatic film or heated discussion—can linger and contribute to waking up during the night. Identifying and adjusting these seemingly minor habits can yield significant improvements in sleep continuity.
Why do I wake up at 3am even when I feel emotionally calm before bed?
Waking up at 3am can occur even in the absence of overt emotional stress due to physiological shifts that are independent of mood. One primary reason is the natural surge in cortisol that begins in the early hours of the morning, preparing your body for the day. For some individuals, this hormonal transition occurs more abruptly, triggering full wakefulness. Additionally, this timeframe often coincides with the lighter stages of REM sleep, during which people are more vulnerable to arousals. Low blood sugar or early signs of insulin resistance can also lead to nocturnal awakenings as the body attempts to stabilize glucose levels. If you consistently wake at this hour and can’t fall back asleep, consider working with a sleep physician to evaluate your cortisol patterns and metabolic health.
How do I distinguish between normal and pathological maintenance insomnia?
Maintenance insomnia becomes clinically significant when it occurs at least three times per week for three months or longer, resulting in noticeable daytime impairment. However, distinguishing it from normal sleep variability requires attention to both frequency and functional impact. Occasional waking is common and often resolves with minor adjustments. In contrast, pathological sleep maintenance insomnia is typically resistant to basic lifestyle changes and may be accompanied by signs such as irritability, cognitive fog, or excessive sleep effort. If you find yourself dreading bedtime, relying heavily on sleep aids, or experiencing a progressive decline in energy levels, it’s likely time to seek a comprehensive sleep evaluation. Understanding whether the problem stems from a chronic sleep disorder or situational stress can guide targeted treatment.
What can adults waking up every 2 hours do to regulate their internal clock more effectively?
Adults waking up every 2 hours often suffer from a disrupted circadian rhythm, which can be gently recalibrated through behavioral and environmental alignment. Exposure to natural sunlight within 30 minutes of waking is a powerful way to anchor your biological clock. Evening routines should include dim lighting and the elimination of electronic screens at least one hour before bed. Eating meals at consistent times, avoiding naps longer than 30 minutes, and incorporating mild evening exercise (without overstimulation) all support circadian regulation. In some cases, using low-dose timed melatonin—under professional guidance—can help reinforce the natural sleep-wake rhythm and reduce the recurrence of constant waking up during the night.
Can unresolved trauma be linked to waking up in the middle of the night?
Yes, trauma—especially when unprocessed—can disrupt the nervous system’s sense of safety during sleep, often manifesting as sudden awakenings in the middle of the night. Individuals with a history of trauma may experience heightened vigilance even in sleep, resulting in exaggerated responses to minor noises or sensations. These awakenings are often accompanied by vivid dreams or feelings of dread that interfere with the ability to return to sleep. Practices such as trauma-informed therapy, EMDR, and somatic experiencing can help reduce these subconscious alarms. Over time, calming the body’s threat detection systems can significantly reduce episodes of waking up in the middle of the night due to psychological tension.
What strategies help most when I can’t fall back asleep during the night?
If you wake up and can’t fall back asleep, it’s essential to avoid activating stress responses that worsen alertness. First, stay away from screens and bright light, which suppress melatonin. Instead, try engaging in a repetitive, neutral mental activity such as counting backward from 300 in threes or recalling the lyrics to a calming song. These techniques subtly divert attention from ruminative thoughts while easing the brain toward drowsiness. If you’re still awake after 20–30 minutes, leave the bedroom and engage in a quiet, relaxing task under low light until you feel sleepy again. Consistent application of this method helps weaken the association between your bed and wakefulness, a key component in treating middle of the night insomnia.
Is sleep maintenance insomnia more common in certain personality types or professions?
Yes, research suggests that individuals with high levels of conscientiousness, perfectionism, or emotional sensitivity are more likely to experience sleep maintenance insomnia. These personality traits often contribute to cognitive hyperarousal—persistent mental activity even during periods of rest. Professions with irregular hours or high performance demands, such as healthcare workers, entrepreneurs, or military personnel, also show higher rates of middle insomnia. The pressure to perform combined with unpredictable schedules can fragment sleep architecture, leading to chronic disruptions. Addressing underlying personality factors through cognitive-behavioral strategies or stress resilience training can be highly effective for these populations in restoring healthy sleep patterns.
Why am I wide awake at night even after a physically exhausting day?
Paradoxically, physical exhaustion doesn’t guarantee deep sleep, particularly if mental stimulation remains high. When the mind remains hyperactive—due to emotional strain, digital overstimulation, or unresolved mental loops—the body may still interpret the environment as unsafe for sleep. Additionally, excessive physical exertion too close to bedtime can elevate adrenaline and core body temperature, both of which delay sleep onset. To help sleeping through the night, shift strenuous workouts to earlier in the day and prioritize calming wind-down routines in the evening. Practices like yin yoga, magnesium-rich meals, and thermal regulation (such as a warm bath followed by a cool room) can better synchronize the mind and body for uninterrupted rest.
How can technology help manage chronic waking up every 2 hours without increasing dependency?
Modern sleep technology can support individuals who keep waking up at 3am or experience fragmented sleep, but it must be used thoughtfully. Smart sleep trackers with EEG sensors can provide detailed insight into sleep cycles, highlighting when and why awakenings occur. Digital CBT-I programs—delivered via apps—allow users to access professional-grade therapy without needing in-person visits. Wearable biofeedback devices can also coach breathing and heart rate variability to induce parasympathetic (rest-and-digest) responses during nighttime awakenings. However, it’s important to avoid obsessive data analysis, which can increase anxiety around sleep. Used wisely, these tools offer actionable information and emotional support, making them valuable adjuncts in addressing sleep maintenance insomnia or constant waking up during the night.
Reclaiming Rest: Overcoming Waking Up Every 2 Hours for Better Sleep Health
Waking up every 2 hours is more than a nuisance; it is a signal from the body that something is amiss. Whether due to stress, hormonal imbalance, sleep apnea, circadian disruption, or anxiety, this pattern of fragmented sleep can erode both physical and mental well-being over time. The good news is that there are effective strategies available to address this issue. From lifestyle changes and sleep hygiene improvements to professional therapies and medical interventions, a variety of tools exist to help people return to deep, uninterrupted slumber.
Understanding the root causes of waking up every 2 hours empowers individuals to take proactive steps toward better rest. When we respect sleep as a vital pillar of health and give it the attention it deserves, the rewards extend far beyond the bedroom. Improved mood, sharper thinking, enhanced immunity, and a more resilient body are all within reach. In a world that often glorifies productivity at the expense of rest, reclaiming sleep is an act of self-care, wisdom, and health preservation. And for those who find themselves staring at the ceiling at 3am, that transformation begins with awareness, commitment, and the willingness to seek help when needed.


