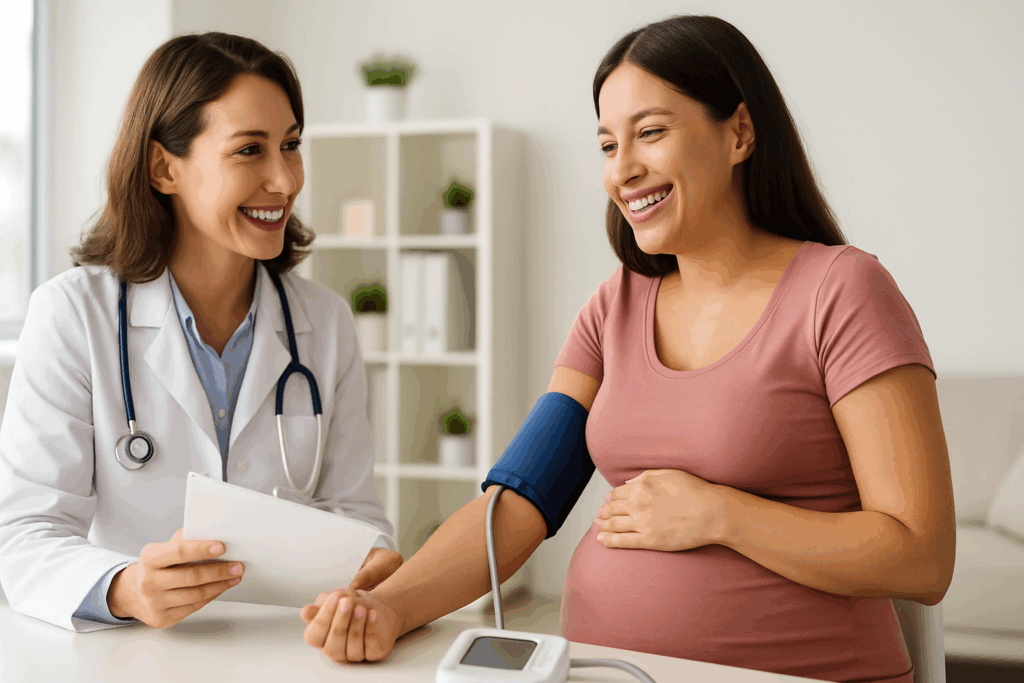
Introduction: The Vital Role of Blood Pressure Monitoring During Pregnancy
Pregnancy is a transformative period filled with physiological changes that affect nearly every system of the body. Among these changes, fluctuations in blood pressure are particularly significant and demand careful attention. For expectant mothers, understanding what is considered high blood pressure in pregnancy is crucial, not only for safeguarding their own cardiovascular health but also for ensuring the optimal development and well-being of their unborn child. High blood pressure during pregnancy, also known as hypertensive disorders of pregnancy, can range from mild elevations that require monitoring to severe complications that pose serious health risks to both mother and baby.
As awareness of gestational hypertension and related conditions has increased, so too has the need for reliable, evidence-based information. Many women ask, “What is considered high blood pressure for a pregnant woman?” or seek to interpret a blood pressure chart for pregnancy to determine whether their readings fall within a normal range. Others want to know how to prevent high blood pressure during pregnancy or are concerned about how to lower blood pressure during pregnancy safely. With such widespread concerns, it becomes clear that a comprehensive understanding of blood pressure in pregnancy is essential.
This article explores the nuances of normal blood pressure in pregnancy, the thresholds for concern, the differences between gestational hypertension and preeclampsia, and the best practices for prevention and management. Drawing on current medical guidelines and incorporating practical insights, we aim to equip pregnant women and their families with the knowledge needed to navigate these complex issues with confidence and care.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Defining Normal Blood Pressure in Pregnancy: What Is Considered Healthy?
During pregnancy, a woman’s cardiovascular system undergoes significant adaptations to support the growing fetus. These changes often cause a temporary dip in blood pressure during the first and second trimesters, followed by a gradual return to pre-pregnancy levels in the third trimester. Despite these fluctuations, a general guideline exists for what constitutes normal blood pressure in pregnancy. For a pregnant woman, normal blood pressure is typically defined as a reading below 140/90 mm Hg. The ideal range often falls closer to 110/70 mm Hg to 120/80 mm Hg.
Clinicians rely on these thresholds to determine whether a pregnant woman is maintaining a healthy blood pressure. A consistent reading above 140/90 mm Hg on two separate occasions, at least four hours apart, is classified as high blood pressure in pregnancy. However, slight variations in the average blood pressure for a pregnant woman are considered acceptable due to physiological changes. The term “normal bp in pregnant woman” should always be contextualized within the stage of pregnancy and the individual’s baseline health status.
Monitoring is critical, as what is considered high blood pressure for a pregnant woman may differ slightly depending on whether the reading occurs early or late in pregnancy. For example, a mild elevation in the second trimester may not be cause for alarm but requires close observation. A blood pressure chart for pregnancy provides a valuable visual tool to help expectant mothers and healthcare providers track trends and detect abnormalities early. The goal is to recognize deviations from the normal blood pressure range during pregnancy before complications arise.
Gestational Hypertension and Preeclampsia: Understanding the Differences
One of the most common questions regarding hypertensive disorders in pregnancy is the distinction between gestational hypertension and preeclampsia. Both conditions involve elevated blood pressure but differ in severity and associated symptoms. Gestational hypertension refers to new-onset high blood pressure after 20 weeks of pregnancy in a woman who previously had normal blood pressure. It does not initially include signs of organ damage or protein in the urine.
Preeclampsia, on the other hand, is a more serious condition characterized by high blood pressure along with signs of organ dysfunction, most commonly involving the kidneys, liver, or brain. Symptoms may include proteinuria (protein in the urine), severe headaches, visual disturbances, upper abdominal pain, and elevated liver enzymes. Gestational hypertension vs preeclampsia is not just a clinical distinction—it also determines the intensity of monitoring and the potential need for early delivery.
The progression from gestational hypertension to preeclampsia is a critical area of concern. Research shows that approximately 15 to 25 percent of women with gestational hypertension may go on to develop preeclampsia. Therefore, identifying what is considered high blood pressure in pregnancy and intervening early is essential to prevent complications such as eclampsia (seizures), HELLP syndrome, or placental abruption.
It is also important to recognize that gestational hypertension and preeclampsia may overlap, leading to confusion. Terms like gestational hypertension vs preeclampsia or gestational htn vs preeclampsia often appear in medical records and patient discussions. Distinguishing these conditions requires not only careful monitoring of blood pressure but also laboratory testing and clinical evaluation.
What Causes High Blood Pressure During Pregnancy?
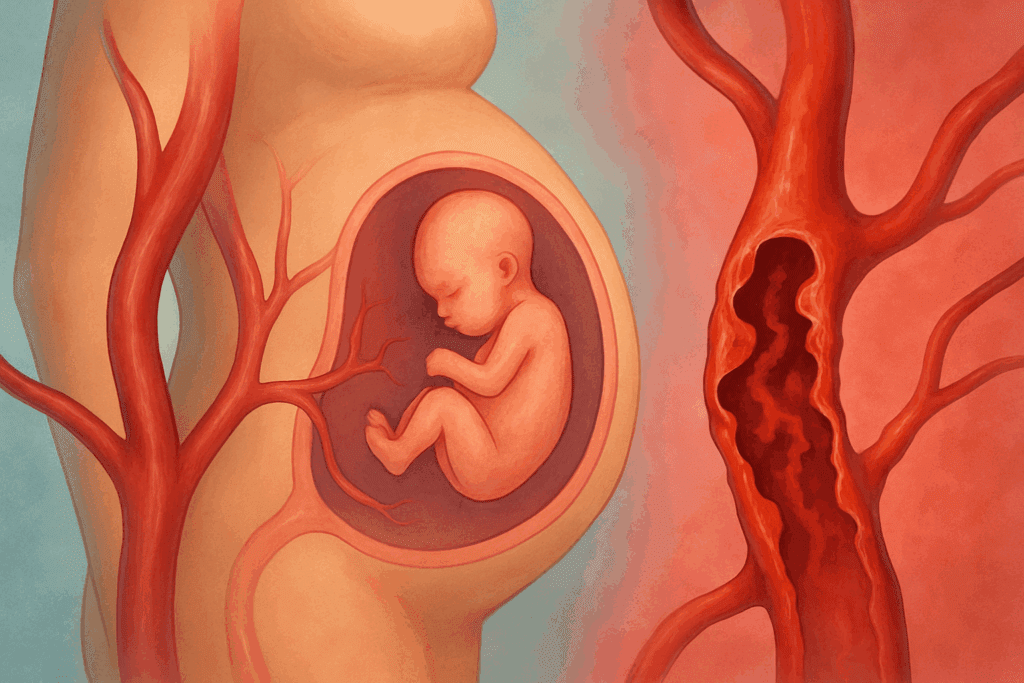
Understanding what causes high blood pressure during pregnancy requires an exploration of both physiological and pathological factors. In many cases, the condition is multifactorial, meaning that several contributing elements interact to elevate blood pressure. Genetic predisposition, preexisting hypertension, autoimmune disorders, and metabolic conditions such as obesity and diabetes can increase a woman’s risk. Environmental factors, including stress, poor nutrition, and sedentary lifestyle, also play a role.
One contributing factor unique to pregnancy is the complex interaction between the placenta and maternal blood vessels. Abnormal placental development or function can lead to insufficient blood flow, triggering the release of inflammatory markers and vasoconstrictors that elevate blood pressure. This mechanism is strongly associated with pregnancy induced hypertension and preeclampsia.
Chronic hypertension in pregnancy—defined as high blood pressure present before pregnancy or before 20 weeks of gestation—can complicate these dynamics further. In such cases, the distinction between gestational hypertension and preeclampsia becomes more nuanced, as baseline hypertension masks new-onset changes.
Importantly, the question “can you have high blood pressure without preeclampsia?” is frequently raised by concerned patients. The answer is yes: not all cases of high blood pressure during pregnancy progress to preeclampsia, especially when managed appropriately. Still, the potential for escalation exists, making continuous evaluation essential.

How to Prevent High Blood Pressure During Pregnancy
Preventing high blood pressure during pregnancy begins with early prenatal care and lifestyle modifications. Regular monitoring by healthcare providers allows for early detection of abnormal trends, making it easier to intervene before hypertension becomes severe. Educating women about the importance of blood pressure checks and helping them understand the average blood pressure for a pregnant woman empowers them to participate actively in their care.
Lifestyle adjustments are especially effective. Maintaining a healthy weight before and during pregnancy, engaging in moderate physical activity, and following a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can significantly lower the risk. Sodium reduction is also recommended, particularly for women with borderline readings. These measures can help maintain a pregnant woman’s normal blood pressure, thereby reducing the likelihood of complications.
Managing stress is another often-overlooked component. Chronic stress can increase cortisol levels, contributing to vascular constriction and elevated blood pressure. Techniques such as prenatal yoga, meditation, and mindfulness have been shown to promote cardiovascular health during pregnancy. Avoiding tobacco and limiting caffeine intake are also part of a comprehensive strategy for how to prevent high blood pressure during pregnancy.
Women with a history of gestational hypertension or other risk factors may require additional support. In some cases, low-dose aspirin is prescribed starting in the second trimester to reduce the risk of preeclampsia. Collaborating with healthcare providers to develop a personalized care plan is the most effective way to achieve and maintain normal blood pressure in pregnancy.

How to Lower Blood Pressure During Pregnancy Safely
When elevated blood pressure is identified, the primary goal is to lower it safely without compromising the health of the mother or the developing fetus. Non-pharmacologic interventions are often the first line of defense. These include dietary adjustments, stress management, and increased physical activity, provided these are cleared by a healthcare provider. Women often ask how to reduce blood pressure while pregnant without medication, and these lifestyle changes provide a safe and effective starting point.
In cases where lifestyle changes are insufficient, blood pressure pills and pregnancy must be considered together with great caution. Not all antihypertensive medications are safe for use during pregnancy. Drugs such as ACE inhibitors and angiotensin receptor blockers (ARBs) are contraindicated due to potential harm to the fetus. Safer alternatives include labetalol, methyldopa, and nifedipine, which are commonly prescribed under close medical supervision.
Understanding how to lower blood pressure during pregnancy also means understanding the importance of individualized treatment. What works for one woman may not be suitable for another, especially when underlying conditions are present. A woman with chronic hypertension in pregnancy will require different management than someone with late-onset gestational hypertension. Therefore, continuous monitoring and adjustments are crucial.
Women should be advised to avoid over-the-counter herbal supplements or home remedies that claim to lower blood pressure, as these can be unpredictable or harmful during pregnancy. Instead, a collaborative approach with a qualified healthcare team ensures that blood pressure is controlled in a manner that prioritizes both maternal and fetal health.
Using Blood Pressure Charts and Monitoring Trends
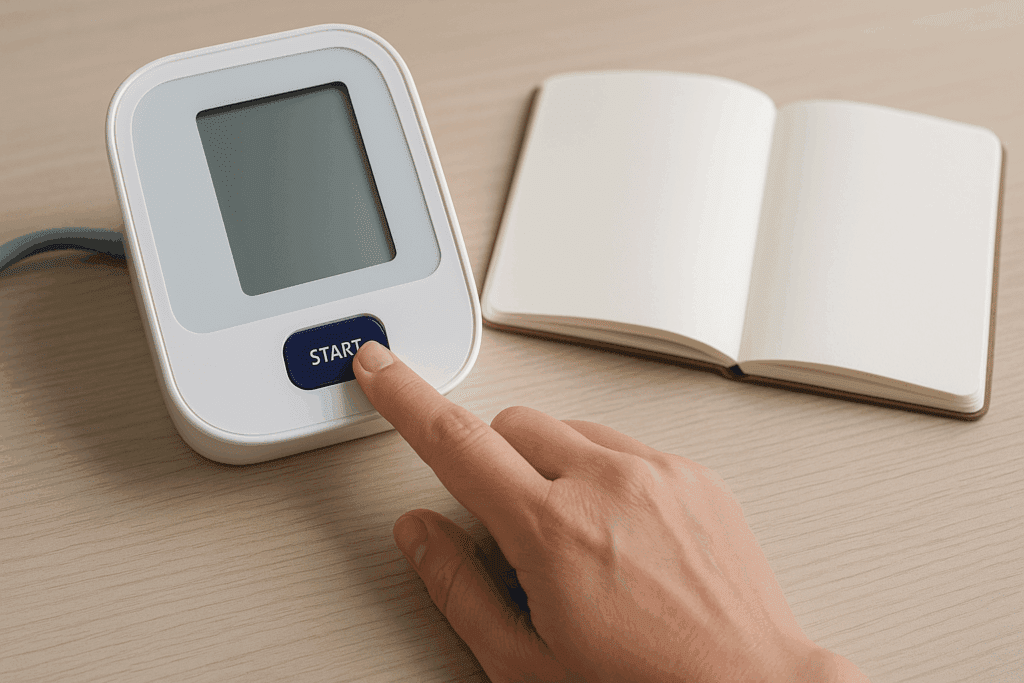
A blood pressure chart for pregnancy is an invaluable resource for tracking cardiovascular health throughout the gestational period. These charts help women identify trends in their readings, differentiate between normal fluctuations and dangerous spikes, and understand where their values fall within the recommended range. The normal blood pressure range during pregnancy chart typically includes color-coded zones that highlight safe, borderline, and high readings.
Using a home blood pressure monitor can further enhance awareness and early detection. When readings consistently fall outside the normal blood pressure range during pregnancy chart, this signals the need for clinical evaluation. It is especially helpful in identifying subtle upward trends that may not immediately trigger symptoms but could evolve into gestational hypertension or preeclampsia if left unchecked.
For example, a pregnant woman whose normal blood pressure has gradually increased from 110/70 to 135/85 over several weeks may still be within the technical limits of normal, but the upward trend suggests a need for vigilance. Recognizing these patterns early can lead to interventions that prevent escalation. Blood pressure monitoring empowers women to become active participants in their healthcare journey, fostering a sense of control during a time when so many changes are beyond their control.
Additionally, maintaining a blood pressure diary, where readings are recorded along with notes about physical activity, stress levels, and dietary choices, can provide valuable insights for both patients and providers. This holistic approach to monitoring supports timely and personalized medical decision-making.
Frequently Asked Questions: High Blood Pressure in Pregnancy
1. How do genetics influence what is considered high blood pressure in pregnancy?
Genetics can significantly impact a woman’s susceptibility to high blood pressure during pregnancy. If a close family member experienced gestational hypertension or pregnancy induced hypertension, a woman may have a heightened risk of developing the same conditions. While lifestyle and environmental factors are also important, inherited traits related to vascular function, kidney performance, and hormonal regulation can contribute to elevated readings. This means that even a pregnant woman with a healthy lifestyle might fall outside the normal blood pressure range during pregnancy chart if she carries certain genetic predispositions. Recognizing this risk early can help guide personalized prevention strategies and facilitate timely monitoring using a reliable blood pressure chart for pregnancy.
2. Can travel or altitude changes impact normal blood pressure in pregnancy?
Yes, environmental changes such as long-distance travel or shifts in altitude can affect blood pressure, especially for pregnant women. High altitudes, in particular, can lead to vasoconstriction, which may temporarily elevate blood pressure in individuals who are already prone to cardiovascular changes. A normal bp in pregnant woman at sea level may appear elevated when measured at altitude, potentially leading to confusion about what is considered high blood pressure in pregnancy. Women with chronic hypertension in pregnancy should consult their physician before planning trips to locations with significant altitude variations. Monitoring changes with a portable device and referencing a blood pressure chart for pregnancy can help differentiate between temporary spikes and sustained elevation.
3. What are the emotional and psychological effects of gestational hypertension?
Experiencing gestational hypertension can lead to increased anxiety, uncertainty, and emotional fatigue, especially when it disrupts a previously uncomplicated pregnancy. Women often worry about how to lower blood pressure during pregnancy without harming their baby, which can lead to stress-induced hypertension, further complicating the situation. The psychological toll may also affect sleep quality and relationships, contributing to a cycle of stress that challenges efforts to maintain normal blood pressure in pregnancy. Access to mental health resources, peer support groups, and prenatal counseling can offer essential emotional relief. Addressing the mental health aspect of high blood pressure pregnancy care is just as important as managing physical symptoms.
4. How do sleep patterns and quality affect high blood pressure during pregnancy?
Poor sleep can directly affect blood pressure regulation due to its impact on the nervous system and hormonal balance. Pregnant women who experience frequent awakenings, sleep apnea, or insomnia are more likely to develop high blood pressure during pregnancy. The disruption in circadian rhythms can elevate cortisol levels, interfering with vascular relaxation and contributing to pregnancy induced hypertension. Developing a healthy sleep routine, including regular sleep-wake times and minimizing screen exposure before bed, may support the goal of maintaining a pregnant woman normal blood pressure. Sleep-focused interventions, including positional therapy or breathing support devices for sleep apnea, may also reduce the risk of gestational hypertension and preeclampsia.
5. Are there any non-invasive tools for tracking normal blood pressure during pregnancy at home?
Yes, modern home blood pressure monitors designed for pregnancy provide accurate, easy-to-use tracking that empowers women to stay informed about their cardiovascular health. These monitors often integrate with smartphone apps that generate trend analyses and alert users when values approach what is considered high blood pressure for pregnant woman. Some models even allow data sharing with healthcare providers, enabling real-time assessment of changes associated with gestational hypertension and preeclampsia. By consistently checking readings and comparing them to a normal blood pressure range during pregnancy chart, women can detect subtle changes early. This proactive approach enhances the safety and well-being of both mother and child, especially for those managing chronic hypertension in pregnancy.
6. What are the long-term cardiovascular risks for women who experience high blood pressure pregnancy complications?
Women who develop high blood pressure during pregnancy, including gestational hypertension and preeclampsia, face an increased risk of future cardiovascular disease. Studies show a heightened incidence of heart attack, stroke, and chronic hypertension later in life among these individuals. Even when blood pressure normalizes postpartum, the vascular changes initiated during pregnancy may persist, making regular monitoring essential. The experience also serves as a valuable early indicator of a woman’s lifelong cardiovascular risk profile, suggesting the need for long-term lifestyle changes. Understanding what causes high blood pressure in pregnancy helps contextualize these long-term risks and encourages preventive care well beyond childbirth.
7. Can dietary choices during pregnancy help reduce the need for blood pressure pills and pregnancy-related medications?
In many cases, adopting a nutrient-rich, low-sodium diet can minimize or even eliminate the need for medications, particularly in mild or borderline cases of gestational hypertension. Incorporating foods high in potassium, magnesium, and fiber supports vascular health and contributes to a normal blood pressure of pregnant lady. While some women may still require pharmacological support due to chronic hypertension in pregnancy, dietary improvements can complement medical treatment and potentially reduce dosage requirements. Registered dietitians who specialize in prenatal care can design meal plans tailored to support a pregnant woman normal blood pressure. This food-as-medicine approach represents a powerful tool in the discussion of how to lower blood pressure during pregnancy naturally.
8. What emerging research is being done on gestational hypertension vs preeclampsia?
Recent studies are exploring the use of biomarkers and advanced imaging to distinguish gestational htn vs preeclampsia more accurately and earlier in pregnancy. Researchers are identifying molecular signals, such as placental growth factor (PlGF) levels, that differ between gestational hypertension and preeclampsia, allowing for earlier intervention. This differentiation is critical for predicting outcomes and customizing treatment strategies to either stabilize blood pressure or address systemic organ involvement. As our understanding of what causes high blood pressure in pregnancy expands, so does the potential to develop targeted therapies that reduce the incidence of both conditions. Future technologies may even integrate AI to analyze patterns in blood pressure chart pregnancy data for real-time decision-making.
9. How can support networks help in managing high blood pressure during pregnancy?
Strong support systems—including family, friends, doulas, and prenatal coaches—play a vital role in helping women navigate the emotional and logistical complexities of high blood pressure pregnancy. A reliable network can reduce feelings of isolation, provide accountability for lifestyle changes, and assist with stress management, all of which contribute to maintaining normal blood pressure in pregnancy. Support can be particularly helpful when making dietary adjustments, scheduling medical appointments, or managing anxiety related to gestational hypertension and preeclampsia. Online forums and telehealth consultations also offer platforms for sharing experiences and receiving expert guidance. These networks become even more essential for women balancing chronic hypertension in pregnancy with other life responsibilities.
10. Is it possible to have fluctuating blood pressure during pregnancy without a formal diagnosis of hypertension?
Yes, blood pressure can vary throughout the day due to posture, hydration, stress, and physical activity, even in women without a formal diagnosis of pregnancy induced hypertension. These fluctuations are usually benign but can mimic early signs of gestational hypertension if not understood properly. Women should be educated on interpreting the average blood pressure for a pregnant woman in the context of timing and environmental conditions. Using a consistent routine for measuring and logging values can help distinguish normal variability from concerning trends. Importantly, having elevated readings does not automatically mean a woman has gestational hypertension or preeclampsia—careful clinical evaluation is required to make that determination.
Conclusion: Prioritizing Cardiovascular Health for a Safer Pregnancy
Understanding what is considered high blood pressure in pregnancy is essential not only for identifying risks but also for taking proactive steps to ensure a healthy pregnancy. With terms like gestational hypertension, preeclampsia, and chronic hypertension in pregnancy frequently entering conversations between patients and providers, clear knowledge of their meanings and implications becomes indispensable.
Whether it’s recognizing the signs of high blood pressure during pregnancy, interpreting a blood pressure chart for pregnancy, or exploring how to lower blood pressure during pregnancy safely, informed decisions are rooted in education and active participation. A pregnant woman’s normal blood pressure may vary slightly depending on individual circumstances, but sustained elevations always warrant attention. Learning how to prevent high blood pressure during pregnancy through lifestyle choices, stress management, and medical care can significantly reduce complications.
From the average blood pressure for a pregnant woman to the nuanced differences between gestational hypertension vs preeclampsia, the insights gained through consistent monitoring and communication with healthcare providers empower women to take charge of their health. The journey of pregnancy is one of growth and adaptation, and with the right support, women can navigate the complexities of blood pressure management with confidence.
Ultimately, maintaining normal blood pressure in pregnancy is not just about numbers on a chart—it’s about fostering a safe and nurturing environment for both mother and baby. Through evidence-based strategies, personalized care, and a commitment to informed choices, expectant mothers can significantly enhance their cardiovascular well-being and ensure the best possible outcomes for their growing families.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
High blood pressure and pregnancy: Know the facts


