Blood pressure, a vital indicator of cardiovascular health, is regulated by a complex interplay of physiological mechanisms that ensure adequate perfusion of organs and tissues. It is neither static nor arbitrary; rather, it responds dynamically to both internal and external stimuli to maintain homeostasis. Understanding what regulates blood pressure is essential not only for medical professionals but also for the broader population, given the high prevalence of hypertension and related conditions. Whether responding to exercise, stress, medication, or dietary intake, the body employs finely tuned systems to ensure that blood pressure remains within an optimal range.
At the center of this regulation are the autonomic nervous system, the kidneys, hormonal responses, and vascular integrity. Each of these components contributes uniquely and synergistically to what controls blood pressure. Additionally, lifestyle factors such as diet, physical activity, and sleep profoundly influence the long-term trajectory of cardiovascular health. The regulation of blood pressure is not merely a physiological curiosity—it is a cornerstone of preventing stroke, heart attack, kidney failure, and other potentially life-threatening outcomes. This article explores the intricate mechanisms and modifiable influences that govern blood pressure control, with a focus on scientific accuracy and practical relevance.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention

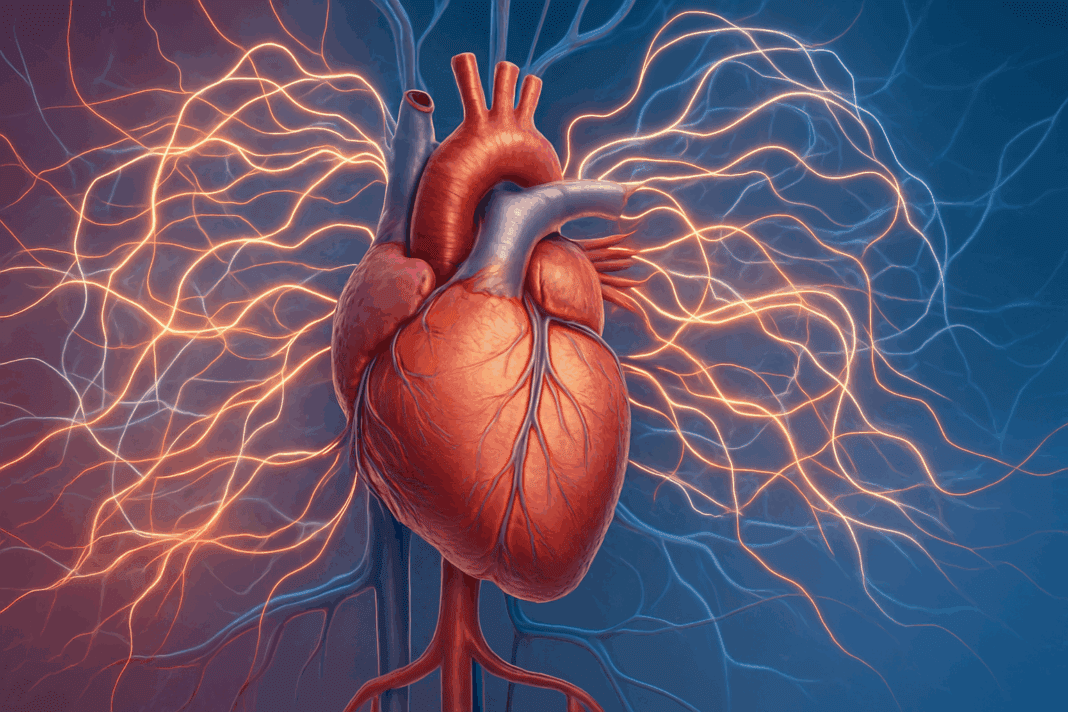
The Autonomic Nervous System: The First Line of Blood Pressure Regulation
The autonomic nervous system (ANS), comprising the sympathetic and parasympathetic branches, is one of the most immediate and responsive regulators of blood pressure. When a person stands up, experiences emotional stress, or engages in physical activity, the ANS rapidly adjusts cardiovascular output to meet the body’s demands. The sympathetic nervous system (SNS) increases heart rate and constricts blood vessels, effectively raising blood pressure to ensure sufficient blood flow to vital organs. In contrast, the parasympathetic system works to calm the body, slowing heart rate and promoting vasodilation when the stressor has passed.
Baroreceptors, specialized stretch-sensitive cells located in the carotid sinuses and aortic arch, serve as real-time sensors for blood pressure changes. These receptors transmit information to the brainstem, which modulates autonomic outflow accordingly. If blood pressure drops, the brain increases sympathetic activity to raise it; if it rises excessively, parasympathetic responses help bring it back down. This feedback loop operates continuously and is remarkably effective in moment-to-moment regulation.
Disruption in autonomic regulation can contribute to disorders such as orthostatic hypotension, where blood pressure falls abnormally upon standing, or in more chronic conditions like autonomic neuropathy in diabetes. Understanding what regulates blood pressure through neural pathways reveals just how sensitive the cardiovascular system is to neurophysiological input. This also underscores the importance of neurological health in maintaining cardiovascular stability.
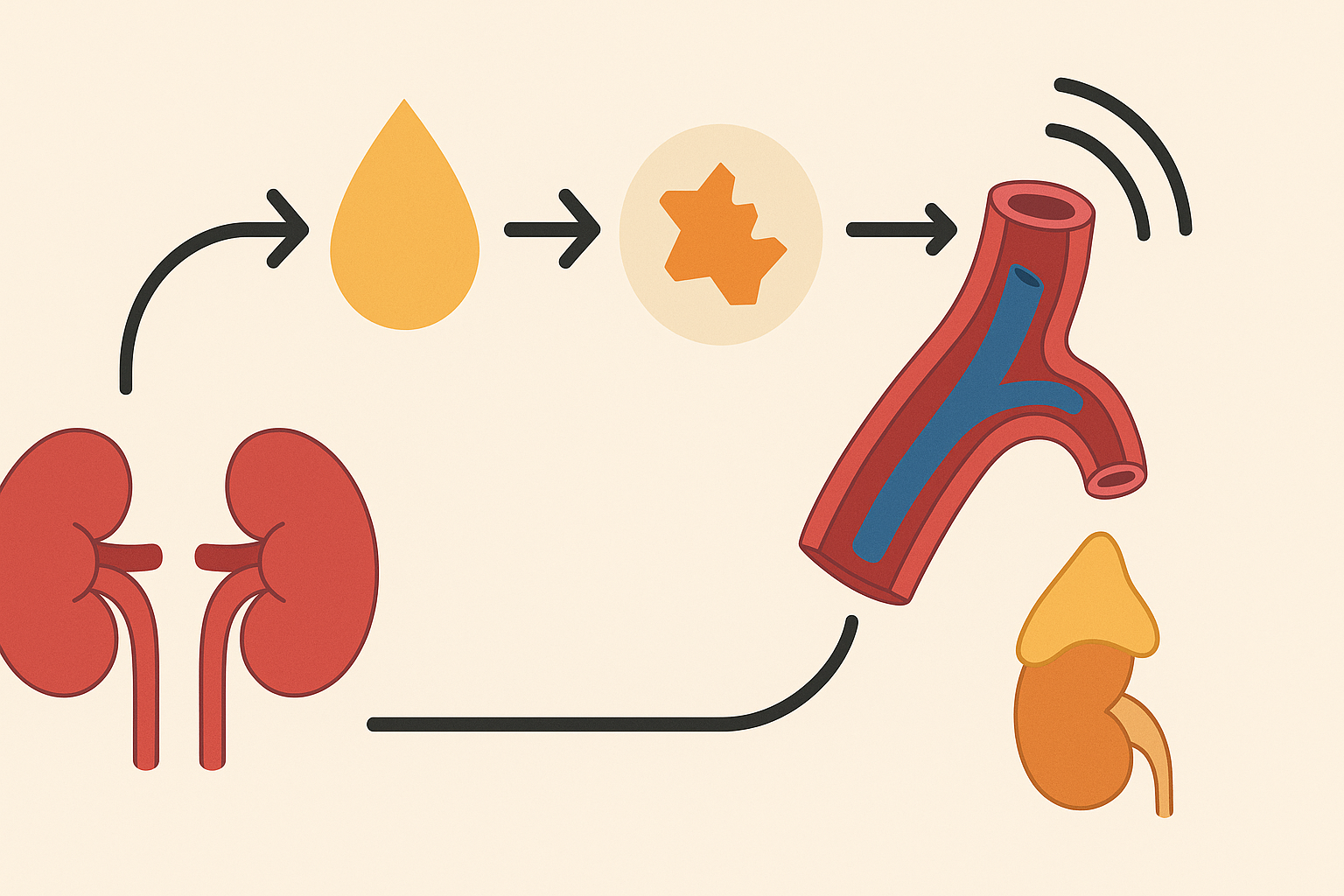
Hormonal Control: The Renin-Angiotensin-Aldosterone System (RAAS)
One of the most significant hormonal regulators of blood pressure is the renin-angiotensin-aldosterone system (RAAS). When blood volume or sodium levels decrease—or when the kidneys detect a drop in perfusion pressure—they release the enzyme renin. Renin catalyzes the conversion of angiotensinogen to angiotensin I, which is then transformed by angiotensin-converting enzyme (ACE) into angiotensin II. This potent peptide has multiple effects: it causes vasoconstriction, stimulates thirst, promotes the release of antidiuretic hormone (ADH), and triggers aldosterone secretion from the adrenal glands.
Aldosterone encourages the kidneys to retain sodium and water, increasing blood volume and, consequently, blood pressure. This system operates over a longer timeframe than the autonomic nervous system but is equally crucial in maintaining homeostasis. Overactivation of RAAS, however, is implicated in the development of chronic hypertension and organ damage, which is why ACE inhibitors and angiotensin receptor blockers (ARBs) are commonly prescribed in hypertensive patients.
Understanding what controls blood pressure through hormonal pathways offers critical insight into the pharmacological management of hypertension. RAAS is not only a target for intervention but also a key to understanding how fluid balance, electrolyte regulation, and vascular tone interact. It exemplifies how a single regulatory axis can influence multiple physiological domains.
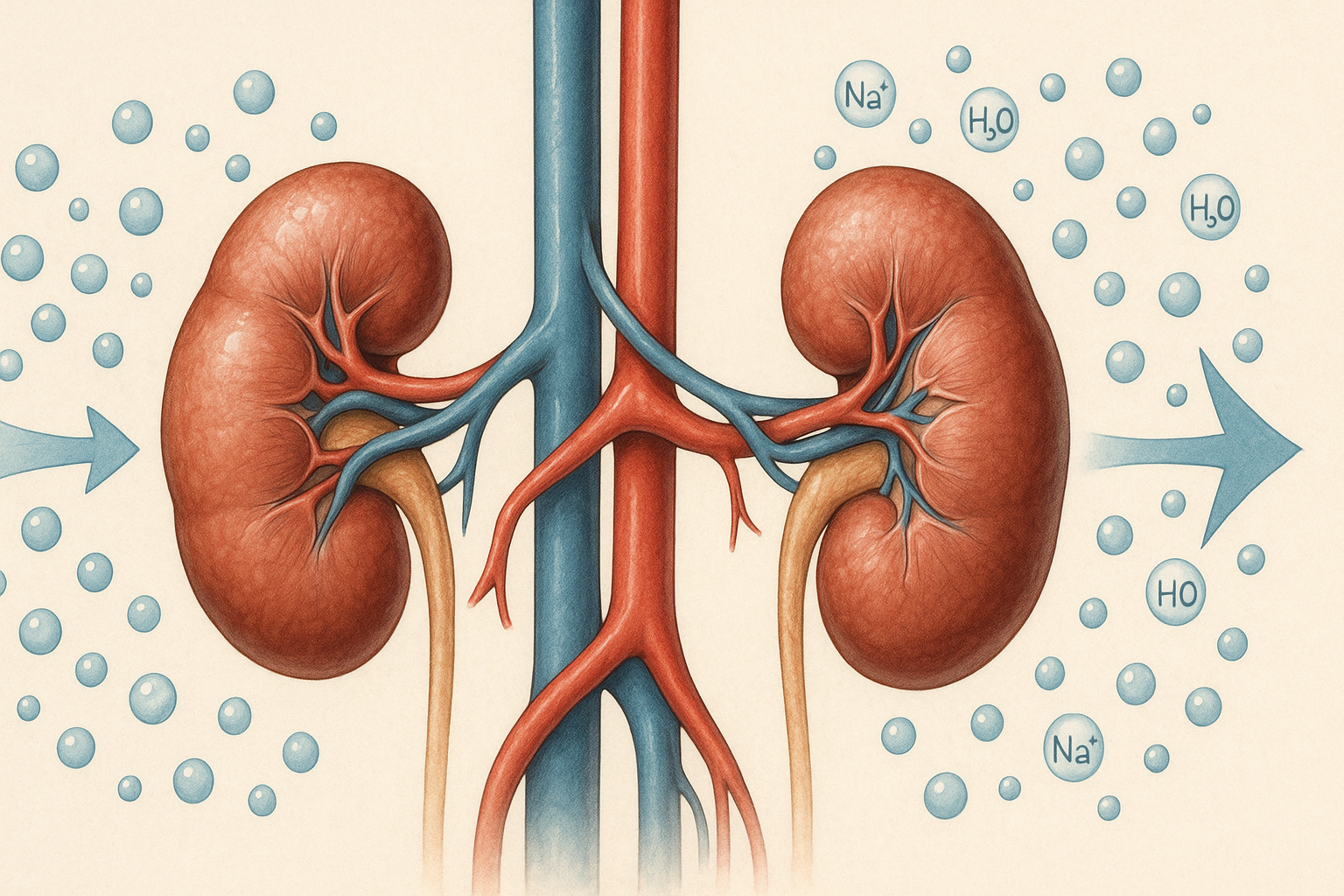
The Role of the Kidneys in Long-Term Blood Pressure Regulation
The kidneys play an indispensable role in long-term blood pressure control through the regulation of extracellular fluid volume and sodium balance. They serve as both sensors and effectors in the complex matrix of cardiovascular regulation. By adjusting the excretion or reabsorption of sodium and water, the kidneys can influence blood volume and, by extension, blood pressure.
When the kidneys retain sodium, water follows, expanding blood volume and increasing pressure within the vascular system. Conversely, increased sodium excretion can lower blood volume and reduce blood pressure. This mechanism is tightly regulated by both neural and hormonal signals, including RAAS and natriuretic peptides, which promote sodium excretion when blood pressure is elevated.
Chronic kidney disease is frequently associated with hypertension, not only because of fluid overload but also due to impaired RAAS feedback and increased systemic vascular resistance. The kidney’s function in blood pressure control is so central that any loss of nephron mass or efficiency can have a cascading effect on cardiovascular health. This interdependence emphasizes the importance of kidney function assessments in managing hypertension and highlights the kidneys as a cornerstone of what regulates blood pressure over the long term.
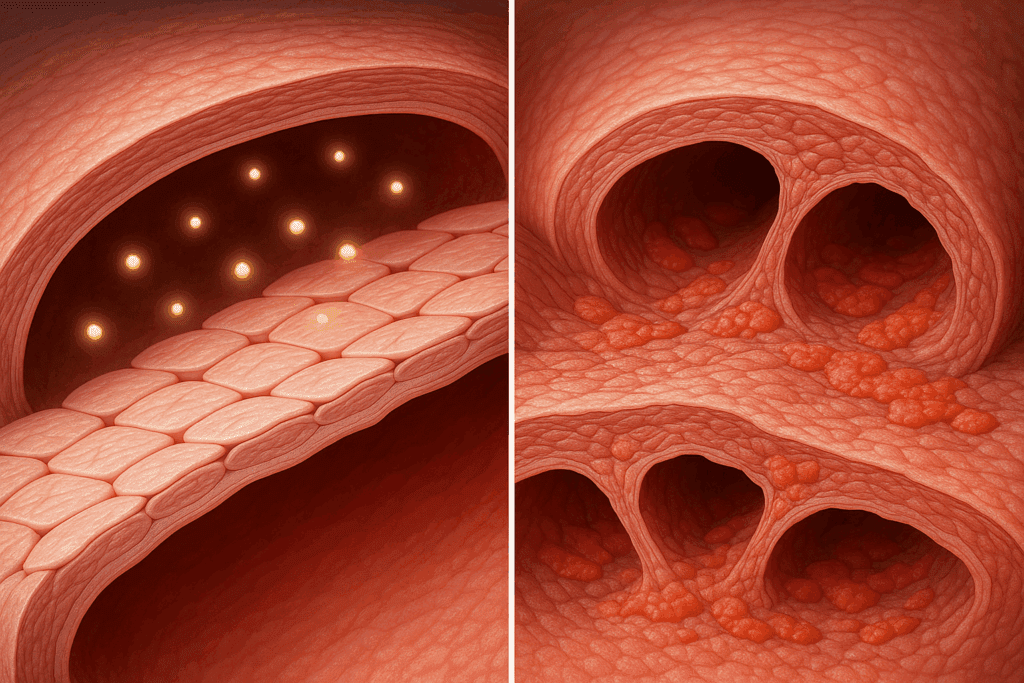
Vascular Resistance and Endothelial Function
Blood pressure is fundamentally a product of cardiac output and systemic vascular resistance, and the latter is largely determined by the diameter and tone of blood vessels. The endothelium, the inner lining of blood vessels, plays a critical role in modulating vascular tone through the release of vasoactive substances such as nitric oxide, endothelin, and prostacyclin.
Nitric oxide is a potent vasodilator that promotes blood vessel relaxation and reduces resistance, thereby lowering blood pressure. Conversely, endothelin is a vasoconstrictor that increases resistance and raises blood pressure. The balance between these substances is influenced by a range of factors, including oxidative stress, inflammation, insulin sensitivity, and mechanical forces such as shear stress.
In conditions like atherosclerosis, endothelial dysfunction results in impaired nitric oxide production and a pro-inflammatory, pro-constrictive state. This leads to increased vascular resistance and sustained elevation in blood pressure. The health of the vascular endothelium is thus pivotal to what controls blood pressure, and interventions aimed at restoring endothelial function—through lifestyle changes, antioxidant therapy, or medications—are vital for long-term cardiovascular health.
The Impact of Lifestyle and Behavioral Factors
While the physiological systems that regulate blood pressure are robust, they are also significantly influenced by lifestyle and behavioral choices. Dietary habits, physical activity, stress levels, sleep quality, and substance use all contribute to blood pressure variability and chronic trends. Among dietary factors, excessive sodium intake is particularly notorious for raising blood pressure, whereas potassium, magnesium, and calcium have protective effects. The DASH (Dietary Approaches to Stop Hypertension) diet, which emphasizes fruits, vegetables, whole grains, and lean proteins, has been shown to significantly lower blood pressure in both hypertensive and normotensive individuals.
Physical activity enhances cardiovascular efficiency, reduces sympathetic overactivity, and improves endothelial function. Even moderate exercise, such as brisk walking for 30 minutes most days of the week, can yield measurable improvements in blood pressure. Chronic stress, on the other hand, can lead to sustained activation of the sympathetic nervous system and elevated cortisol levels, contributing to hypertension over time.
Sleep deprivation and poor sleep quality have also emerged as independent risk factors for hypertension, partly through disruptions in autonomic and hormonal regulation. Substance use—including excessive alcohol, tobacco, and certain stimulants—can have a direct pressor effect and undermine the body’s ability to maintain balanced blood pressure control. Understanding what regulates blood pressure, therefore, must include a holistic appreciation of behavioral influences and their interactions with physiological systems.
Genetic and Epigenetic Influences on Blood Pressure Regulation
Genetics play a foundational role in determining an individual’s baseline blood pressure and susceptibility to hypertension. Numerous genes have been implicated in blood pressure regulation, including those involved in sodium handling, vascular tone, and sympathetic activity. For example, polymorphisms in the angiotensinogen gene or the beta-adrenergic receptor gene can predispose individuals to higher blood pressure under environmental stressors.
Epigenetic mechanisms, which involve changes in gene expression without alterations in DNA sequence, also contribute to the regulation of blood pressure. These include DNA methylation, histone modification, and microRNA activity, which can be influenced by factors such as diet, stress, and early-life exposures. Epigenetic changes may help explain why some individuals develop hypertension despite similar environmental exposures, and why certain interventions are more effective for some people than others.
The burgeoning field of personalized medicine seeks to leverage this genetic and epigenetic knowledge to tailor interventions for optimal blood pressure control. Understanding what controls blood pressure at the genetic level not only deepens our appreciation of its complexity but also opens new avenues for prevention and treatment that are individualized and precise.

Environmental and Circadian Influences on Blood Pressure
Blood pressure is not static throughout the day—it follows a circadian rhythm, typically dipping during sleep and rising upon awakening. Disruptions to this pattern, such as in shift workers or those with sleep apnea, are associated with increased cardiovascular risk. The central circadian clock, located in the hypothalamus, interacts with peripheral clocks in the heart, kidneys, and vasculature to coordinate these fluctuations.
Environmental factors such as temperature, altitude, and air pollution also influence blood pressure regulation. Cold temperatures can cause vasoconstriction and elevate blood pressure, while high altitudes may trigger adaptive mechanisms involving increased erythropoietin and sympathetic activity. Air pollution, particularly fine particulate matter (PM2.5), has been linked to endothelial dysfunction and increased blood pressure through inflammatory pathways.
Recognizing the role of environmental and circadian influences is essential for a comprehensive understanding of what regulates blood pressure. These factors may be less amenable to individual control but are important considerations for public health strategies aimed at reducing the global burden of hypertension.
Medications and Medical Conditions That Affect Blood Pressure Regulation
Several medications can directly or indirectly impact blood pressure regulation. Antihypertensive agents such as ACE inhibitors, calcium channel blockers, beta-blockers, and diuretics are designed to modulate the physiological systems involved in blood pressure control. However, other drugs—including corticosteroids, NSAIDs, and certain antidepressants—may raise blood pressure as a side effect.
Medical conditions such as diabetes, thyroid disorders, adrenal tumors (e.g., pheochromocytoma), and sleep apnea can disrupt the normal mechanisms that control blood pressure. In secondary hypertension, identifying and addressing the underlying cause is crucial for effective management. Regular monitoring and a comprehensive medical evaluation are often needed to distinguish between essential and secondary forms of hypertension.
Understanding what regulates blood pressure in the context of comorbid conditions and pharmacological influences enhances clinical decision-making and promotes better outcomes. It also reinforces the importance of personalized treatment plans that consider the full spectrum of contributing factors.
Frequently Asked Questions: What Regulates and Controls Blood Pressure
1. How does emotional well-being influence what regulates blood pressure?
Emotional health has a powerful and often underappreciated impact on what regulates blood pressure. Chronic anxiety, unresolved trauma, and high-stress lifestyles stimulate prolonged sympathetic nervous system activation, which can contribute to elevated blood pressure over time. This stress-induced state affects hormonal regulation, particularly increasing cortisol and adrenaline levels, which disrupt vascular tone and renal function. Practices like mindfulness, cognitive behavioral therapy, and emotional regulation exercises have been shown to help recalibrate the neurohormonal circuits that control blood pressure. Understanding these emotional triggers offers a deeper insight into how our mental state interconnects with physiological systems responsible for blood pressure regulation.
2. Can gut health play a role in what controls blood pressure?
Emerging research suggests that the gut microbiome plays a more significant role in what controls blood pressure than previously thought. Specific strains of gut bacteria influence inflammation, nitric oxide production, and metabolic pathways that directly affect vascular tone and systemic resistance. Dysbiosis, or microbial imbalance, can increase endotoxins that impair endothelial function and elevate blood pressure. Probiotic supplementation, fiber-rich diets, and fermented foods may support healthier blood pressure through microbial modulation. While not traditionally considered a core mechanism, gut health now represents a novel frontier in the broader conversation about what regulates blood pressure.
3. How do socioeconomic factors affect what regulates blood pressure in different populations?
Socioeconomic status can heavily influence both direct and indirect factors related to what regulates blood pressure. Individuals from lower-income backgrounds often face higher levels of chronic stress, limited access to nutritious food, and reduced opportunities for physical activity. Environmental stressors, such as noise pollution and unsafe living conditions, can further impair the autonomic and hormonal systems that control blood pressure. Disparities in healthcare access may delay diagnosis and proper management, exacerbating long-term cardiovascular risk. These social determinants of health reveal that what controls blood pressure extends well beyond biology and into structural and societal domains.
4. What role does hydration play in what controls blood pressure, especially in older adults?
Proper hydration is crucial in determining what controls blood pressure, especially among the elderly, whose thirst response and renal concentrating abilities may be diminished. Dehydration can reduce plasma volume and trigger compensatory mechanisms such as increased heart rate and vasoconstriction, which raise blood pressure. Conversely, overhydration in individuals with compromised kidney function may result in fluid overload and hypertensive episodes. Maintaining optimal hydration helps balance electrolytes and supports kidney function, both of which are central to what regulates blood pressure. Encouraging regular fluid intake, particularly water and low-sodium broths, becomes a simple yet effective strategy in older adults.
5. Are there technological innovations that can improve how we monitor what controls blood pressure in real time?
Yes, modern technology is revolutionizing how we observe and influence what controls blood pressure in real time. Wearable devices equipped with photoplethysmography (PPG), AI-driven analytics, and even non-invasive cuffless monitors are making continuous blood pressure tracking more accessible. These tools can detect subtle fluctuations linked to stress, activity, or medication adherence, offering immediate feedback for both patients and clinicians. By enabling personalized insights, these innovations allow a more responsive and precise understanding of what regulates blood pressure on a moment-to-moment basis. Such advancements not only empower self-care but also enhance early detection of trends that may require intervention.
6. How does climate or seasonal change impact what regulates blood pressure?
Seasonal and climatic variations play a surprisingly significant role in what controls blood pressure. In colder environments, vasoconstriction is more pronounced as the body attempts to conserve heat, often leading to temporary increases in blood pressure. During warmer months, vasodilation can lead to lower readings, though dehydration in hot climates may counteract this effect. Additionally, seasonal affective disorder (SAD) and altered physical activity levels can indirectly affect the neuroendocrine systems that regulate blood pressure. Recognizing these patterns can help patients and clinicians anticipate and adapt blood pressure management strategies accordingly throughout the year.
7. Can certain breathing techniques influence what controls blood pressure naturally?
Targeted breathing exercises are a promising non-pharmacological tool for influencing what controls blood pressure. Techniques such as slow diaphragmatic breathing, alternate-nostril breathing, and guided biofeedback have been shown to reduce sympathetic arousal and enhance vagal tone. This shift in autonomic balance supports vasodilation and lowers cardiac output, contributing to more stable blood pressure readings. Regular practice has even been associated with improved baroreceptor sensitivity, an essential element of real-time regulation. These techniques represent a low-cost, accessible intervention for individuals seeking to better understand and manage what regulates blood pressure.
8. How does long-term exposure to noise pollution affect what regulates blood pressure?
Long-term noise exposure—particularly in urban environments—can exert a stealthy yet profound impact on what controls blood pressure. Chronic noise acts as a persistent stressor, activating the hypothalamic-pituitary-adrenal (HPA) axis and increasing sympathetic tone. Over time, this can lead to vascular remodeling, increased arterial stiffness, and heightened systemic resistance. Sleep disturbances from nocturnal noise further degrade autonomic recovery, compounding the effects. Policies aimed at reducing environmental noise, alongside soundproofing strategies in personal spaces, can contribute to healthier blood pressure regulation in affected populations.
9. What is the relationship between circadian rhythm disruption and blood pressure regulation?
Disruption of the circadian rhythm profoundly alters what regulates blood pressure. Normally, blood pressure follows a diurnal pattern—dipping during sleep and peaking in the early morning. Shift work, frequent travel across time zones, and sleep disorders like insomnia or apnea can flatten or reverse this pattern. Such alterations disturb hormonal secretion patterns, including melatonin and cortisol, which modulate vascular tone and fluid balance. Interventions such as light therapy, consistent sleep routines, and chronotherapy (timing medications according to circadian rhythms) are emerging tools to help restore natural blood pressure control mechanisms.
10. How might future research evolve our understanding of what controls blood pressure?
Future research is likely to expand our understanding of what regulates blood pressure by integrating systems biology, precision medicine, and digital health technologies. Scientists are investigating gene-environment interactions, metabolomics, and the role of neural networks that extend beyond the classical autonomic and hormonal models. Moreover, advances in machine learning could help predict individual responses to different interventions, whether pharmacologic or lifestyle-based. Artificial intelligence may also reveal hidden patterns in large datasets, helping to uncover new physiological pathways that control blood pressure. This evolving landscape underscores that while our current knowledge is robust, we are only beginning to unravel the full complexity of what controls blood pressure in a personalized, predictive manner.
Conclusion: Why Understanding What Regulates Blood Pressure Is Vital for Lifelong Cardiovascular Health
Blood pressure regulation is a multifaceted, dynamic process involving neural, hormonal, renal, vascular, genetic, behavioral, and environmental components. Each plays an integral role in what controls blood pressure on both a moment-to-moment and long-term basis. The body’s ability to maintain stable blood pressure is a testament to the intricate coordination of these systems, yet it is also vulnerable to disruption from disease, lifestyle, and environmental stressors.
Gaining a deep understanding of what regulates blood pressure is not just of academic interest—it has profound implications for clinical practice, public health, and individual wellness. From the rapid responses of the autonomic nervous system to the long-term influences of renal function and genetic predisposition, every aspect of regulation offers opportunities for intervention and optimization.
As the burden of cardiovascular disease continues to rise globally, empowering individuals and healthcare providers with accurate, actionable knowledge about blood pressure control is more important than ever. Prevention and treatment strategies must be grounded in science, tailored to individual needs, and responsive to emerging insights into how our bodies maintain this vital sign. By appreciating the complex interplay of systems that regulate blood pressure, we are better equipped to promote cardiovascular resilience, longevity, and overall health.