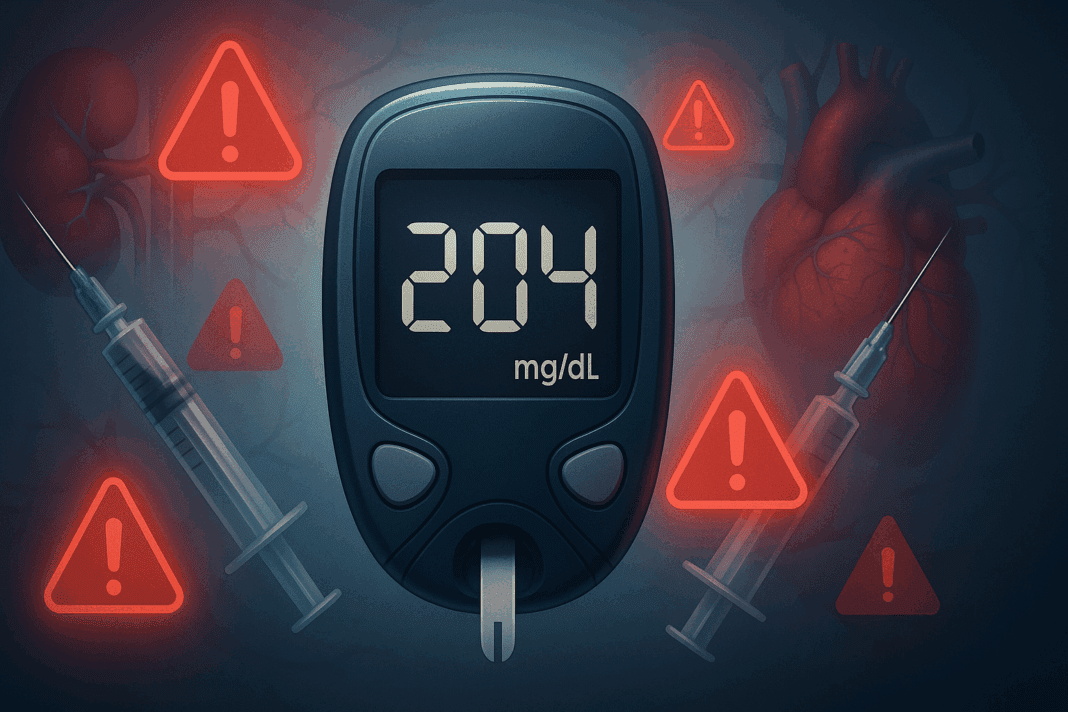
Understanding the Urgency of Blood Sugar Spikes
When blood sugar spikes to 200 mg/dL or higher, it signals more than just a numerical fluctuation; it reflects an urgent metabolic imbalance that demands timely intervention. For individuals managing type 2 diabetes mellitus with hyperglycemia, such elevated glucose levels can arise unexpectedly from dietary choices, stress, illness, or lapses in medication. But for many, the realization begins with a troubling question: My blood sugar is over 200—what should I do? Recognizing this inflection point is critical, as blood sugar level 200 or above is not just a temporary deviation but a marker that immediate action is needed to prevent complications such as dehydration, fatigue, and in severe cases, diabetic ketoacidosis or hyperosmolar hyperglycemic state.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
The body operates within a narrow glucose threshold, typically maintaining blood sugar levels between 70 and 130 mg/dL before meals. When glucose level 200 or higher is recorded, the excess sugar circulating in the bloodstream can lead to cellular damage over time, particularly in the eyes, kidneys, nerves, and blood vessels. High sugar levels in type 2 diabetes not only impair insulin sensitivity but also initiate inflammatory cascades that compound cardiovascular risk. Thus, addressing a 200 sugar level promptly and effectively is not just about comfort—it’s about preventing long-term damage.
Informed responses to blood sugar above 200 begin with understanding the underlying mechanisms and identifying patterns in your personal glucose data. Whether this level represents a one-time post-meal surge or a chronic elevation indicative of poorly controlled diabetes 2 high blood sugar, the actions you take can determine whether the trajectory leads to improvement or further escalation. Knowing how to treat high blood glucose properly and consistently remains a cornerstone of preventing both acute and chronic complications.
What Causes Blood Sugar to Spike to 200 or Higher?
Several physiological and lifestyle-related factors can contribute to a sudden rise in blood sugar levels, leading to hyperglycemia. A common cause is dietary intake rich in carbohydrates, particularly simple sugars and processed foods that rapidly convert to glucose in the bloodstream. A person with type ii diabetes glucose levels may rise substantially after consuming high-glycemic meals without balancing them with fiber, protein, or physical activity. This imbalance leads to increased insulin resistance or insufficient insulin response.
Other contributors include physical inactivity, which diminishes the body’s ability to utilize circulating glucose efficiently. Even short-term stress—emotional or physical—can lead to the release of counter-regulatory hormones like cortisol and adrenaline that raise glucose levels. Additionally, infections, certain medications such as corticosteroids, and hormonal shifts can trigger or exacerbate high blood sugar levels in both type 2 and type 1 diabetes.
Insufficient or missed doses of oral hypoglycemic agents or insulin can also be a direct pathway to blood sugar surges. For patients with type 2 diabetes who usually control their disease through lifestyle modifications or medication, any disruption in routine can tilt the delicate balance of glucose regulation. When that tipping point results in a reading like 200 sugar level, it’s a red flag that these variables may be converging.
Equally important are the hidden triggers—chronic inflammation, sleep disturbances, and hormonal imbalances such as thyroid dysfunction or polycystic ovary syndrome (PCOS)—that silently push glucose levels upward. A comprehensive understanding of what causes high sugar levels in type 2 diabetes allows for targeted strategies to avoid future spikes.
Recognizing the Symptoms of Type 2 Diabetes Hyperglycemia
One of the challenges in managing hyperglycemia is that symptoms can be subtle until blood sugar levels are significantly elevated. When evaluating whether 200 blood sugar is high, it’s essential to correlate it with how the body feels and functions. Classic signs of high sugar levels in type 2 diabetes include increased thirst (polydipsia), frequent urination (polyuria), and unexplained fatigue. These arise as the body attempts to rid itself of excess glucose through urine, leading to dehydration and energy depletion.
Other warning signs may include blurred vision, headaches, and a general feeling of malaise. In cases where type 2 diabetes high sugar symptoms persist over days or weeks, individuals might notice weight loss despite normal or increased appetite, a phenomenon caused by the body’s inability to use glucose effectively. Some patients also experience slow wound healing or recurrent infections, as elevated glucose impairs immune function.
When blood sugar level 200 becomes the norm rather than the exception, these symptoms evolve from episodic discomfort to chronic health threats. It’s vital to distinguish between temporary elevations and persistent high glucose levels requiring sustained treatment. Recognizing symptoms of hyperglycemia in diabetes type 2 is a first line of defense against complications.
For those asking, Is 200 sugar level high? the answer is clinically and functionally affirmative. It reflects an imbalance that, when left unchecked, may escalate to more serious conditions such as neuropathy, nephropathy, and retinopathy. Early recognition empowers patients to seek appropriate high blood sugar level treatment before damage accumulates.

Immediate Actions to Take When Blood Sugar Is Above 200
If your blood sugar is above 200, the first step is to remain calm and begin assessing possible causes. A single high reading, particularly after a large meal, may not warrant emergency intervention, but it does necessitate awareness. Hydration is essential; drinking water can help dilute blood glucose and support renal excretion of excess sugar. Light physical activity, such as walking, can also assist in lowering glucose levels through enhanced insulin sensitivity and muscle uptake of glucose.
Monitor your blood sugar closely to identify whether levels continue to rise or begin to fall. If glucose remains elevated for several hours or is accompanied by symptoms such as nausea, vomiting, confusion, or abdominal pain, seek medical attention. These may signal impending diabetic ketoacidosis or other serious complications that require urgent care. For individuals newly diagnosed or unsure about their status, a blood sugar level 200 reading is a clear prompt to consult a healthcare provider.
Knowing what to take for high blood sugar depends on your treatment plan. For some, this may include rapid-acting insulin or adjusting the dosage of oral medications. Others may need to discuss the initiation or adjustment of pharmacologic therapy. For those managing diabetes 2 high blood sugar through diet and exercise, this may be a time to review strategies with a dietitian or diabetes educator.
Immediate steps taken after discovering a sugar over 200 level can prevent a single event from becoming a pattern. It also reinforces the principle that glucose control is not a static achievement but a dynamic balance responsive to behavior, environment, and physiology.

Evidence-Based Treatment Options for High Blood Sugar
Treating high blood sugar involves a multifaceted approach tailored to the individual’s clinical profile, lifestyle, and preferences. Pharmacological interventions remain a mainstay for many, especially those with type 2 diabetes mellitus with hyperglycemia. Metformin is often the first-line oral agent due to its efficacy in reducing hepatic glucose production and improving insulin sensitivity. Other oral and injectable medications, such as GLP-1 receptor agonists, SGLT2 inhibitors, and DPP-4 inhibitors, offer additional options with benefits extending beyond glycemic control to weight loss and cardiovascular protection.
In cases where blood sugar level 200 is persistent despite oral therapy, insulin may be introduced either temporarily or as part of a long-term strategy. Basal-bolus regimens allow for precise control of fasting and postprandial glucose, reducing fluctuations that lead to complications. For those managing high blood sugar type 1 or late-stage type 2 diabetes, insulin remains essential.
Non-pharmacologic treatments are equally important. Medical nutrition therapy (MNT) provides individualized dietary plans that emphasize low-glycemic index foods, adequate fiber intake, and controlled carbohydrate consumption. Incorporating physical activity not only assists with glucose uptake but also improves lipid profiles, blood pressure, and overall metabolic health. These strategies are core components of any high glucose levels treatment protocol.
Behavioral interventions, including structured diabetes self-management education and support (DSMES), empower patients to make informed decisions and maintain long-term glycemic control. Evidence shows that patients who actively engage in such programs experience fewer hospitalizations and complications. Therefore, effective high blood sugar treatment goes beyond medication—it requires a commitment to comprehensive lifestyle integration.
How to Prevent Blood Sugar Spikes in Type 2 Diabetes
Prevention is a powerful tool in diabetes care, and the goal is to minimize the frequency and severity of hyperglycemic episodes. Understanding what is the normal sugar level for type 2 diabetes helps set realistic targets. Generally, pre-meal glucose should be between 80 and 130 mg/dL, and post-meal levels should not exceed 180 mg/dL. Keeping blood sugar within this range involves proactive monitoring and consistent self-care.
Diet plays a central role in prevention. Meals rich in complex carbohydrates, paired with protein and healthy fats, slow glucose absorption and reduce postprandial spikes. Portion control, meal timing, and awareness of carbohydrate counting further refine glucose management. These habits become second nature for patients with type 2 diabetes who usually control their disease successfully.
Exercise enhances insulin sensitivity and glucose uptake, reducing fasting and postprandial blood sugar. A combination of aerobic and resistance training yields optimal results. Sleep, often overlooked, is another critical factor; insufficient or poor-quality sleep is associated with impaired glucose tolerance and increased insulin resistance.
Stress management is essential for both emotional well-being and glucose control. Mindfulness practices, cognitive-behavioral therapy, and even regular social engagement can buffer the physiological effects of chronic stress. Addressing these risk factors for hyperglycemia holistically ensures better long-term outcomes.

New Research on Managing and Reversing Type 2 Hyperglycemia
Recent medical research is reshaping how we understand and manage type 2 hyperglycemia. Studies now show that early intensive interventions, even within the first year of diagnosis, can induce long-term remission of type 2 diabetes in some individuals. The DiRECT trial demonstrated that sustained weight loss of 10-15 kg through dietary intervention led to normalized blood sugar in nearly half of participants, highlighting the potential for disease reversal.
Pharmacological innovations continue to emerge. Dual and triple agonist drugs that target multiple hormonal pathways simultaneously have shown promise in improving glucose levels, reducing appetite, and supporting cardiovascular health. Precision medicine is also advancing the personalization of high blood sugar level treatment, considering genetic, metabolic, and lifestyle factors to optimize therapeutic outcomes.
Continuous glucose monitoring (CGM) has revolutionized real-time tracking of glucose trends, allowing for dynamic feedback and improved self-management. This technology empowers individuals to identify patterns, refine insulin dosages, and understand the impact of specific foods or activities on their glucose control. It also assists clinicians in designing more precise treatment for high glucose.
Stem cell therapy, gut microbiome modulation, and digital health platforms are among the emerging areas of exploration. These breakthroughs suggest a future where treatment extends beyond symptom control to fundamental shifts in metabolic function. For patients with persistent readings such as a glucose level 200, these innovations offer hope for deeper, more lasting solutions.
Frequently Asked Questions About Blood Sugar Spikes and Type 2 Diabetes Hyperglycemia
1. What makes blood sugar levels rise suddenly even when I follow a diabetes-friendly diet?
It may be surprising, but even when someone is diligently managing type 2 diabetes mellitus with hyperglycemia, sudden spikes can occur due to several overlooked variables. One common factor is the glycemic load of foods, not just the glycemic index. Even healthy carbs, when consumed in large quantities or without protein or fat, can cause a glucose surge. Sleep deprivation and stress are also significant contributors to sudden high sugar levels in type 2 diabetes, as both can increase cortisol, which elevates blood glucose. Moreover, hidden sugars in sauces, condiments, or processed foods can cause blood sugar level 200 or higher, even when meals appear balanced. Managing these nuances is key in treating high blood sugar effectively.
2. If my blood sugar is over 200, what should I do before taking medication?
When you’re thinking, “my blood sugar is over 200 what should I do,” the impulse may be to reach for medication immediately. However, it’s worth taking a pause to assess contributing factors. First, rehydrate—water helps flush out excess glucose. Then consider light movement such as walking, which can lower blood sugar naturally. Also review your recent meals, stress levels, or missed medications to understand why you reached a 200 sugar level. High blood sugar treatment should be contextual and personalized—if the high persists despite these steps, medication may indeed be necessary, but understanding the root cause is just as critical for long-term control.
3. Are there psychological factors that affect high blood sugar levels in people with type 2 diabetes?
Absolutely. Emotional stress plays a significant but often underestimated role in high blood sugar type 1 and type 2 alike. Chronic stress activates the hypothalamic-pituitary-adrenal (HPA) axis, elevating cortisol and adrenaline, which counteract insulin and raise glucose levels. People dealing with anxiety, grief, or depression may see unexplained increases in glucose level 200 or more, even when their diet and medication remain unchanged. Effective high glucose levels treatment must incorporate mental health strategies such as mindfulness, therapy, or stress-reduction practices to complement pharmacological interventions. A comprehensive approach to treating high blood sugar should always consider both physiological and psychological dimensions.
4. How do changing hormones affect blood sugar management in type 2 hyperglycemia?
Hormonal fluctuations can significantly impact type ii diabetes glucose levels, particularly in women. Menstrual cycles, menopause, or conditions like PCOS (polycystic ovary syndrome) can alter insulin sensitivity, sometimes making blood sugar above 200 more difficult to avoid during specific times of the month. Similarly, thyroid imbalances may disrupt glucose metabolism. For men, shifts in testosterone can also affect insulin function and weight distribution. These hormonal factors add complexity to high blood sugar level treatment, requiring patients and providers to adapt strategies over time and tailor treatment for high glucose according to hormonal life stages.
5. Can physical fitness offset occasional spikes like a blood sugar level 200?
Yes, to a degree. Regular exercise improves insulin sensitivity and facilitates glucose uptake by muscles, often preventing moderate spikes from escalating into chronic hyperglycemia. Even if you hit a 200 sugar level post-meal, being physically active can help bring levels down more efficiently. Over time, consistent activity reduces baseline glucose and improves cardiovascular resilience—a critical benefit for patients with type 2 diabetes who usually control their disease through lifestyle. However, exercise is not a standalone cure. For those with persistent diabetes 2 high blood sugar, fitness must be combined with proper diet, medication, and stress control to be truly effective.
6. Is 200 blood sugar high if I just finished eating, or is that normal?
This is a common question: Is 200 blood sugar high after eating, or can it be considered a typical postprandial rise? Generally, blood glucose should stay below 180 mg/dL two hours after meals, according to American Diabetes Association guidelines. A blood sugar level 200 or more after eating may signal impaired insulin response or excessive carbohydrate intake. For people with type 2 diabetes hyperglycemia, consistent post-meal spikes increase the risk of vascular complications. While one-time readings may not warrant alarm, repeated elevations call for reassessment of meal timing, portion size, and possibly medication adjustments as part of long-term high blood sugar treatment.
7. What role do hydration and electrolytes play in treating high blood sugar?
Hydration is often overlooked in the context of high blood sugar level treatment. When blood sugar rises, the kidneys work harder to excrete excess glucose, pulling water and electrolytes like potassium, sodium, and magnesium with it. This can lead to dehydration, fatigue, and muscle cramps. Rehydrating with water—not sugary sports drinks—is essential, but maintaining electrolyte balance is also key. Especially when dealing with a glucose level 200 or higher, ensuring adequate magnesium intake may support insulin sensitivity, making hydration a critical yet simple strategy in treating high blood sugar effectively.
8. Can wearable technology help prevent sugar over 200 episodes in type 2 diabetes?
Yes, wearable technology has transformed how we approach type 2 hyperglycemia management. Continuous glucose monitors (CGMs) provide real-time insights that allow patients to catch and address blood sugar fluctuations before they reach problematic thresholds like a 200 sugar level. This proactive approach helps in high glucose levels treatment by identifying food patterns, sleep disruptions, or emotional triggers that contribute to spikes. Some advanced devices even offer predictive alerts, empowering users to intervene before blood sugar rises above 200. Wearables are especially valuable for patients with type 2 diabetes mellitus with hyperglycemia who are experimenting with different treatment regimens or experiencing erratic patterns.
9. What is the normal sugar level for type 2 diabetes, and how flexible are those numbers in real life?
The standard clinical targets suggest fasting blood sugar should be between 80 and 130 mg/dL, with post-meal readings under 180 mg/dL. But in reality, managing type 2 diabetes high sugar symptoms involves more nuance. Age, comorbidities, medication risks, and individual goals all influence what constitutes “normal” for a given patient. For older adults or those with other health concerns, slightly higher targets might be appropriate to avoid hypoglycemia. In contrast, younger individuals newly diagnosed with diabetes 2 high blood sugar may aim for tighter control to reverse early damage. Context matters when defining what is the normal sugar level for type 2 diabetes in practice.
10. How does long-term exposure to blood sugar above 200 affect diabetes management over time?
Persistent exposure to a blood sugar level 200 or more accelerates the risk of complications such as retinopathy, neuropathy, and cardiovascular disease. But beyond physical effects, it also contributes to psychological burnout—a lesser-known yet impactful aspect of type 2 diabetes management. Patients often feel frustration or defeat when repeated efforts fail to prevent a sugar over 200 reading. This can erode motivation, reduce adherence, and hinder long-term success in treating high blood sugar. Innovative models of care, such as behavioral coaching and patient support communities, are helping reframe this narrative. Sustainable high blood sugar level treatment requires not just biomedical solutions but emotional and community-based support systems as well.
Final thoughts on High Blood Sugar: Understanding, Treating, and Preventing Glucose Spikes Above 200
When it comes to managing blood sugar levels that exceed 200, knowledge and action go hand in hand. A single elevated reading—whether termed 200 sugar level, sugar over 200, or blood sugar above 200—is not just a number but a signal that the body’s glucose regulation is under strain. Recognizing this signal and responding with the right combination of hydration, activity, dietary adjustments, and medication can prevent escalation and support long-term stability.
For individuals living with type 2 diabetes hyperglycemia, consistent monitoring, and proactive lifestyle changes are the foundation of success. While asking Is blood sugar level of 200 high? may seem like a simple question, it opens the door to complex considerations about insulin function, hormonal balance, and metabolic resilience. The key lies not in fear, but in informed action rooted in evidence-based strategies.
As research evolves, so does the potential for more effective high blood sugar treatment and prevention. The integration of cutting-edge pharmacology, wearable technology, and personalized care plans marks a new era in diabetes management. Whether addressing acute symptoms or navigating chronic challenges, the path forward for high sugar levels in type 2 diabetes is paved with science, support, and self-empowerment.
Further Reading:
Hyperglycemia (High Blood Sugar): Symptoms & Treatment
Type 2 Diabetes: What It Is, Causes, Symptoms & Treatment
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.