High blood pressure, or hypertension, is one of the most common and insidious health conditions affecting adults around the globe. Often called the “silent killer” due to its lack of obvious symptoms, hypertension can quietly damage the heart, blood vessels, kidneys, and brain over time, often without warning until a severe event like a heart attack or stroke occurs. While much attention is rightly focused on lifestyle choices and preventive strategies, there comes a point for many people when lifestyle changes are not enough—and medication becomes a necessary tool in managing blood pressure. But when, exactly, does this happen? What is the average age to start blood pressure medication, and how does age influence the course of hypertension?
Understanding these questions requires more than a surface-level look at blood pressure trends. The decision to begin pharmacological treatment involves complex interactions between age, genetics, comorbidities, and evolving clinical guidelines. By exploring the data, medical consensus, and individual variation in treatment pathways, we can gain a clearer perspective on what the average age to start blood pressure medication truly reflects—and what it means for people navigating hypertension at different stages of life.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
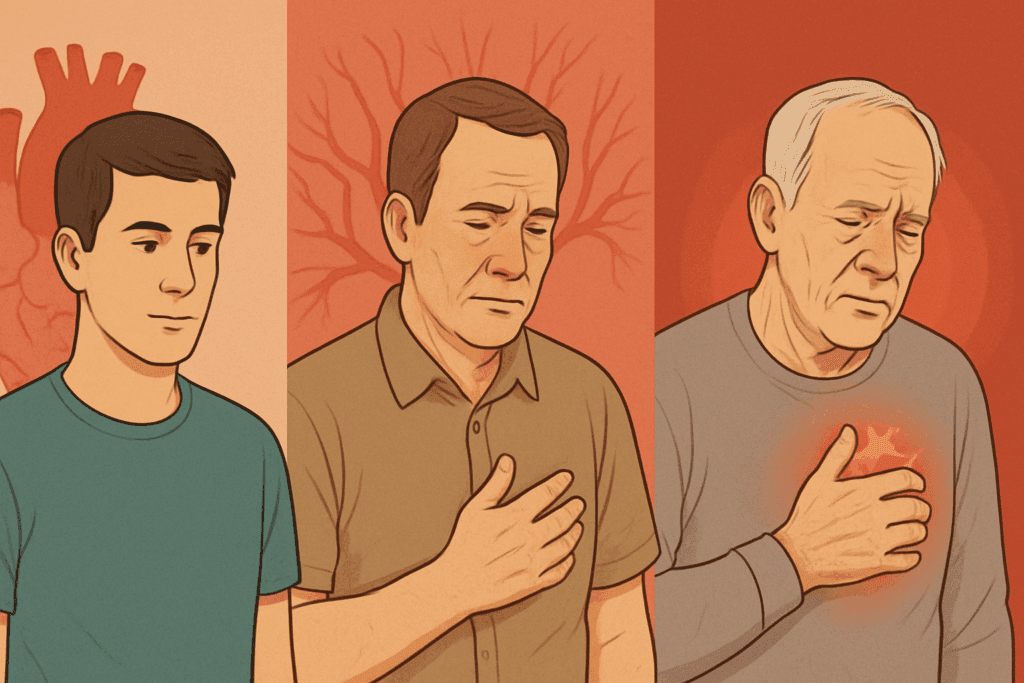
The Progressive Nature of Hypertension and Why Age Matters
Hypertension is a progressive condition, meaning that it tends to worsen over time if left unmanaged. In many people, blood pressure starts to creep up as early as their 30s and continues climbing through the decades. This slow but steady rise is influenced by a variety of factors, including arterial stiffening, declining kidney function, increased body weight, and cumulative lifestyle exposures such as high sodium intake, alcohol consumption, and lack of physical activity. While genetics also play a critical role, age remains one of the most consistent predictors of rising blood pressure.
In general, systolic blood pressure—the top number in a blood pressure reading—increases more markedly with age than diastolic pressure. This means that isolated systolic hypertension, a condition where only the systolic number is elevated, becomes more common in older adults. This type of hypertension is particularly dangerous, as it has been closely linked to an increased risk of heart attack and stroke.
Age matters not just because of biological aging, but because it often correlates with the cumulative burden of risk factors. A 60-year-old person who has been overweight for decades, has type 2 diabetes, and smokes is at a higher risk for complications than a 30-year-old with no comorbidities. This cumulative risk often compels physicians to start medication earlier in certain individuals, depending on their overall health status and the rate at which their blood pressure is increasing.
Defining the Average Age to Start Blood Pressure Medication
There is no universally fixed age at which individuals start taking medication for hypertension, but data from large-scale epidemiological studies can provide useful benchmarks. According to the National Health and Nutrition Examination Survey (NHANES) and other population-level studies, the average age to start blood pressure medication in the United States tends to be around 49 to 55 years. However, this average is influenced by many contextual variables, including race, sex, socioeconomic status, and access to healthcare.
For instance, African American individuals tend to develop hypertension at younger ages and often experience more severe forms of the disease, which may lead to earlier initiation of treatment. Women, on the other hand, often see a rise in blood pressure after menopause, shifting the average age of onset and treatment toward the post-menopausal years. In lower-income populations, where preventive care may be lacking, people may not receive treatment until their condition becomes symptomatic or advanced, which can distort average age metrics.
Moreover, the “average age to start blood pressure medication” should be understood not as a recommendation but as a population trend. Many people begin treatment earlier or later based on their individual health profile. The average simply provides a reference point within the context of a large and diverse population, and it should not dictate clinical decisions for any one person.
The Role of Guidelines in Determining Treatment Thresholds
Clinical guidelines for managing hypertension have evolved significantly over the past two decades. Organizations such as the American College of Cardiology (ACC) and the American Heart Association (AHA) have periodically updated their recommendations in response to emerging evidence from clinical trials and observational studies. These updates influence when and how clinicians initiate medication.
One major shift came in 2017, when the ACC and AHA redefined hypertension as a blood pressure reading of 130/80 mmHg or higher, compared to the previous threshold of 140/90 mmHg. This change effectively increased the number of people classified as hypertensive, particularly among those in their 40s and early 50s, thereby potentially lowering the average age to start blood pressure medication. However, the updated guidelines also emphasized a more nuanced approach, encouraging lifestyle modifications as the first line of treatment for many patients in the newly reclassified category.
These evolving thresholds are especially significant when discussing hypertension age trends. People who might have previously been advised to watch and wait are now often encouraged to take earlier action—either through behavioral change or medication—based on their cardiovascular risk profile. This dynamic has made age a more fluid factor in treatment decisions, requiring personalized approaches rather than rigid age-based rules.

Early-Onset Hypertension: A Growing Concern
While hypertension has traditionally been considered a condition of middle age and older adulthood, an increasing number of young adults are being diagnosed with elevated blood pressure. This trend is concerning, not only because of the long-term health risks associated with early-onset hypertension but also because it challenges traditional assumptions about the average age to start blood pressure medication.
Several factors contribute to this shift. Rising rates of obesity, sedentary lifestyles, and high-sodium diets among younger populations are accelerating the onset of cardiovascular risk factors. Additionally, stress—both psychological and socioeconomic—has been identified as a significant contributor to elevated blood pressure in younger demographics. In some cases, these individuals may require pharmacological treatment earlier than expected, especially if lifestyle interventions fail to bring blood pressure under control.
The implications of early-onset hypertension are far-reaching. Studies have shown that people diagnosed with hypertension before the age of 40 have a significantly higher lifetime risk of cardiovascular disease, even if their blood pressure is later well-managed. This underscores the importance of early detection, sustained intervention, and, when necessary, a willingness to initiate medication earlier in life to mitigate long-term risk.
Personalized Medicine and the Future of Hypertension Management
In an era increasingly defined by personalized medicine, the approach to managing hypertension is shifting away from one-size-fits-all strategies. Genetic testing, advanced risk calculators, and wearable blood pressure monitors are allowing for more tailored treatment plans that consider not just age, but the totality of a person’s health profile. This personalized approach may ultimately refine how we define the optimal hypertension age for intervention.
Pharmacogenetics, the study of how genes affect a person’s response to drugs, is a burgeoning field that holds promise for hypertension management. Some individuals may metabolize certain medications faster or slower than others, affecting both efficacy and risk of side effects. By leveraging this knowledge, physicians can choose the most appropriate medication earlier in the treatment process, potentially improving outcomes and reducing the trial-and-error phase often associated with blood pressure management.
As technology advances, the average age to start blood pressure medication may become less relevant than the context in which treatment is initiated. Tools that assess arterial stiffness, cardiac output, and other markers of cardiovascular health could soon become standard parts of routine checkups, offering clinicians a more comprehensive understanding of an individual’s risk—and helping determine the precise moment when medication should be introduced.
Navigating Medication Decisions: When Lifestyle Isn’t Enough
Lifestyle modifications are universally recommended as the first-line treatment for mild to moderate hypertension. These include dietary changes such as reducing sodium and increasing potassium intake, engaging in regular physical activity, maintaining a healthy weight, limiting alcohol consumption, and managing stress. For many people, these changes can significantly lower blood pressure and delay or even eliminate the need for medication.
However, lifestyle interventions are not always sufficient, particularly in cases of stage 2 hypertension or when other risk factors—such as diabetes, chronic kidney disease, or a history of cardiovascular events—are present. In such instances, the decision to start medication is not simply a matter of age but a reflection of the overall clinical picture.
The average age to start blood pressure medication may suggest a general timeline, but real-world decisions are made on a case-by-case basis. For someone in their 30s with a family history of heart disease and consistently high readings, waiting until the average age may not be advisable. Conversely, an otherwise healthy 60-year-old with borderline readings might delay medication through aggressive lifestyle management. Understanding this nuance is crucial for patients and providers alike.
Rethinking Age-Based Stereotypes in Hypertension Care
There is a persistent stereotype that associates hypertension solely with aging, reinforcing the idea that high blood pressure is inevitable after a certain age. While it is true that the risk increases with age, this perception can be misleading and even dangerous. It may cause both patients and providers to overlook early signs of hypertension in younger individuals, thereby delaying necessary intervention.
Conversely, some older adults are placed on blood pressure medications without a comprehensive evaluation of their broader health status, which can lead to overtreatment and side effects such as dizziness, electrolyte imbalances, and kidney dysfunction. In very elderly patients, aggressive blood pressure lowering has sometimes been associated with an increased risk of falls and cognitive decline. These findings support a more individualized approach that weighs the risks and benefits of treatment within the context of a person’s age, overall health, and personal preferences.
The focus, therefore, should not be on hitting a specific hypertension age or average treatment milestone but on achieving optimal cardiovascular health throughout the lifespan. This may mean reevaluating the role of medication at different ages, taking into account how priorities and risk factors evolve over time.

The Psychosocial Impacts of Starting Blood Pressure Medication
Starting any long-term medication can be a psychologically significant event, and blood pressure medication is no exception. For many, the decision marks a turning point in how they perceive their health. Younger individuals, in particular, may feel that starting medication signifies premature aging or the onset of chronic illness, which can impact mental health and treatment adherence.
It is essential for healthcare providers to recognize these emotional dynamics and offer support, education, and reassurance throughout the treatment journey. Framing the use of medication not as a failure, but as a proactive step toward long-term wellness, can shift the narrative and encourage better engagement with treatment plans. Clear communication about the reasons for initiating medication—especially when lifestyle efforts have plateaued—is critical in fostering trust and adherence.
Understanding that the average age to start blood pressure medication does not dictate personal readiness can empower patients to focus on their individual needs rather than societal benchmarks. Ultimately, the goal is not to avoid medication at all costs, but to use it wisely, effectively, and in the right context.
Frequently Asked Questions: Hypertension and Blood Pressure Medication
1. Can starting blood pressure medication before the average age be beneficial for long-term health?
Yes, initiating treatment before the average age to start blood pressure medication—typically around the late 40s to early 50s—can be highly beneficial for those at elevated risk. Early intervention is especially critical in individuals with a family history of cardiovascular disease, chronic kidney issues, or metabolic syndrome. While age is a common consideration, it should never be the sole factor in deciding when to begin treatment. Targeting hypertension age trends through proactive monitoring in younger populations may prevent vascular damage and reduce the likelihood of complications like stroke or heart failure later in life. The decision to start earlier is best made in consultation with a physician using tools that assess lifetime cardiovascular risk.
2. Are there psychological effects associated with starting blood pressure medication at a younger-than-average age?
Absolutely. Many younger individuals feel a sense of stigma or failure when they begin medication earlier than the perceived average age to start blood pressure medication. This emotional response can influence adherence, self-esteem, and how people view their long-term health trajectory. However, reframing medication as a proactive step rather than a sign of deterioration helps mitigate these effects. Some patients benefit from counseling or group support, particularly when they must reconcile their hypertension age with personal or cultural expectations around youth and vitality. Physicians can support patients emotionally by explaining how early treatment can empower them to preserve health and avoid complications.
3. How does sleep quality affect the decision to start blood pressure medication regardless of age?
Poor sleep has been strongly linked to elevated blood pressure levels, regardless of one’s hypertension age. Sleep apnea, insomnia, and fragmented rest can lead to persistent nocturnal hypertension, a condition that often goes undetected with standard daytime monitoring. If lifestyle efforts to improve sleep do not yield better blood pressure readings, medication might be initiated even before reaching the average age to start blood pressure medication. This highlights the importance of 24-hour monitoring and the growing use of wearable technology to evaluate nighttime blood pressure patterns. Addressing sleep disturbances may delay the need for medication or inform the type and timing of pharmacologic therapy.
4. Can certain professions influence the age at which someone starts blood pressure medication?
Yes, occupational stress and environmental exposures can accelerate the timeline for developing hypertension, potentially lowering the average age to start blood pressure medication among certain workers. For instance, individuals in high-stakes careers like emergency responders, airline pilots, and financial traders often experience chronic stress, irregular schedules, and poor sleep—all risk factors for hypertension. In such populations, the hypertension age curve may shift earlier, and employers are increasingly including cardiovascular screenings in routine health assessments. Preventive strategies in workplace health programs, such as guided meditation or ergonomic improvements, are emerging to address these unique risks and delay the need for medication.
5. Is there a difference in medication response based on the age treatment is initiated?
The effectiveness and side effect profile of antihypertensive medications can vary significantly depending on the age of initiation. People who begin therapy closer to the average age to start blood pressure medication often tolerate a wider range of drugs compared to older adults, who may experience more side effects due to changes in metabolism and organ function. Younger patients may respond well to lower doses and more targeted therapy, especially if caught early in the course of the disease. Conversely, older adults may require multiple medications due to stiffened arteries and coexisting conditions. Tailoring medication regimens based on hypertension age and biological age rather than calendar age is becoming increasingly relevant in clinical decision-making.
6. How might future technologies alter the average age to start blood pressure medication?
Emerging technologies are poised to reshape the hypertension landscape by enabling earlier detection and more personalized interventions. With the advent of continuous blood pressure monitoring, AI-driven risk modeling, and at-home diagnostic tools, physicians may identify and address blood pressure anomalies before they manifest in standard clinic readings. This could result in a gradual decrease in the average age to start blood pressure medication, especially among tech-savvy individuals who track their health proactively. Moreover, advances in pharmacogenomics could match patients with medications most suited to their genetic makeup, minimizing trial-and-error periods and optimizing early intervention strategies across all hypertension age groups.
7. How do social determinants of health influence when someone begins blood pressure treatment?
Access to healthcare, education level, and socioeconomic status all play a significant role in determining the actual versus ideal hypertension age for treatment. Individuals in underserved communities may not receive a diagnosis until symptoms become severe, pushing the average age to start blood pressure medication higher than necessary. Conversely, those with better healthcare access often receive earlier diagnoses through routine screenings. The disparity also extends to trust in medical systems, with some populations delaying care due to historical or cultural concerns. Addressing these inequities is essential in refining treatment timelines and ensuring that hypertension management aligns with need rather than circumstance.
8. Can hormone fluctuations, such as during menopause, influence the need to start medication at a specific age?
Yes, hormonal shifts during menopause significantly impact blood pressure, often leading to a rise in systolic pressure. This natural transition can result in many women reaching the hypertension age threshold and starting treatment shortly after menopause, regardless of prior health status. The loss of estrogen’s protective vascular effects is a primary factor. Women may also experience weight gain, metabolic changes, and increased salt sensitivity during this phase, further elevating their risk. Clinicians should proactively monitor women in their late 40s and 50s for signs of rising blood pressure and consider medication when these factors combine to exceed safe thresholds—even if this precedes the statistically average age to start blood pressure medication.
9. What lifestyle changes can most effectively delay the need for blood pressure medication, especially before reaching the average treatment age?
Adopting a heart-healthy lifestyle early in life can significantly delay the hypertension age at which medication becomes necessary. The DASH (Dietary Approaches to Stop Hypertension) diet, rich in vegetables, fruits, whole grains, and lean proteins, has shown particular promise in lowering blood pressure naturally. Regular aerobic exercise, stress reduction techniques such as yoga or mindfulness, and limiting alcohol and sodium intake are equally important. While genetics and family history still play a role, sustained lifestyle interventions can help individuals remain medication-free well past the average age to start blood pressure medication. Importantly, these strategies should be tailored to each individual’s preferences and circumstances for long-term adherence.
10. Is it ever advisable to discontinue blood pressure medication after long-term use if blood pressure normalizes?
In select cases, patients may be able to taper off blood pressure medication under medical supervision, particularly if lifestyle changes have been dramatic and sustained. However, this is more likely in those who started treatment early—possibly below the average age to start blood pressure medication—due to modifiable risk factors rather than irreversible conditions. If blood pressure remains stable for an extended period and the original causes have been mitigated, such as significant weight loss or improved sleep, a gradual reduction in dosage may be considered. It is critical to monitor closely during this time, as hypertension often recurs silently. The key takeaway is that the hypertension age at which medication begins does not necessarily dictate lifelong use, especially when paired with consistent health improvements.
Conclusion: What the Average Age to Start Blood Pressure Medication Reveals—and Why It’s Only Part of the Story
The average age to start blood pressure medication provides a helpful reference point for understanding population trends in hypertension care, but it should never substitute for personalized clinical judgment. Age, while influential, is only one piece of a multifactorial puzzle that includes genetics, comorbidities, lifestyle, access to healthcare, and emerging medical technologies. As the understanding of cardiovascular risk continues to evolve, so too will the strategies for managing it.
The notion of a definitive “hypertension age” oversimplifies a complex, lifelong health issue. People are being diagnosed and treated at increasingly diverse ages, driven by changes in clinical guidelines, improved diagnostic tools, and shifting lifestyle patterns. The focus must remain on individualized, evidence-based care that considers each patient’s unique profile rather than relying on averages or assumptions.
In the end, starting blood pressure medication is not a failure or a concession to aging. It is a strategic decision aimed at reducing long-term health risks and preserving quality of life. By reframing the conversation around blood pressure treatment to emphasize personalization, prevention, and patient empowerment, we can better support individuals at every stage of life as they navigate the challenges and choices of hypertension care.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Hypertension: What You Need to Know as You Age