High blood pressure, or hypertension, has long been referred to as “the silent killer.” This ominous label is not merely rhetorical; it reflects a very real and urgent medical reality. Many individuals live with high blood pressure for years without experiencing any noticeable symptoms, yet this condition quietly inflicts damage on vital organs and substantially raises the risk of life-threatening events such as heart attacks, strokes, and kidney failure. In this article, we explore why hypertension is known as the silent killer, the mechanisms by which it silently compromises health, and the steps individuals can take to detect, manage, and mitigate its long-term consequences. As we dive into the science and clinical implications behind this condition, we also unpack the broader meaning of what is the silent killer medical communities warn about so often, and why early detection and intervention are critical for survival.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Understanding High Blood Pressure and Its Physiological Impact
To understand why high blood pressure is called the silent killer, we must first grasp how blood pressure works and what happens when it remains elevated over time. Blood pressure is the force exerted by circulating blood against the walls of the body’s arteries. It is measured using two numbers: systolic pressure, which occurs when the heart beats, and diastolic pressure, which occurs when the heart is at rest between beats. A normal reading typically falls below 120/80 mmHg.
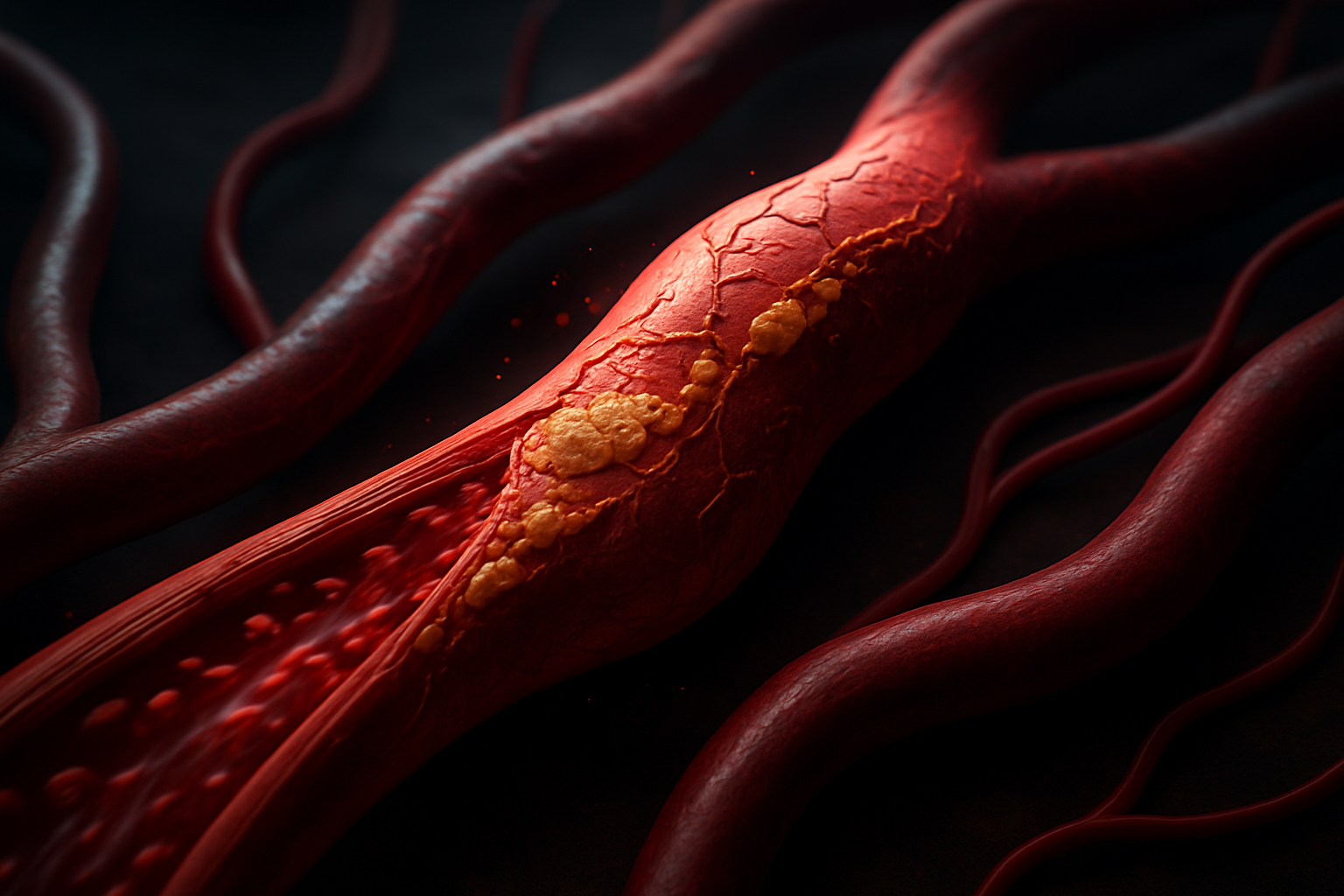
When blood pressure remains consistently high, it increases the strain on the heart and arteries. This extra force can damage the delicate lining of the blood vessels, accelerate the buildup of plaque (atherosclerosis), and reduce the elasticity of arteries over time. The heart, in response to this pressure, must work harder to pump blood, potentially leading to conditions such as left ventricular hypertrophy or even heart failure. It’s in this insidious, gradual wear and tear that hypertension earns its reputation as a silent killer disease. The damage is often already significant by the time any symptoms appear, if they appear at all.
Why Is High Blood Pressure Known as the Silent Killer?
Hypertension’s reputation as the silent killer stems from its subtle, often symptomless progression. Unlike infections that present with fever or pain, or injuries that signal distress, high blood pressure may quietly persist without triggering any noticeable discomfort. This allows the disease to go undetected for years, quietly causing harm in the background. By the time a person experiences symptoms such as headaches, blurred vision, or chest pain, the damage to the cardiovascular system and other organs may already be considerable.
The absence of symptoms doesn’t equate to the absence of harm. On the contrary, this is precisely why is high blood pressure known as the silent killer in medical literature and among healthcare professionals. Hypertension is frequently only diagnosed during routine checkups or after an acute event like a stroke or myocardial infarction. Without regular monitoring, individuals may remain unaware that they are living with a condition that is steadily raising their risk of morbidity and mortality.
The Mechanisms of Hidden Harm: How Hypertension Silently Affects the Body
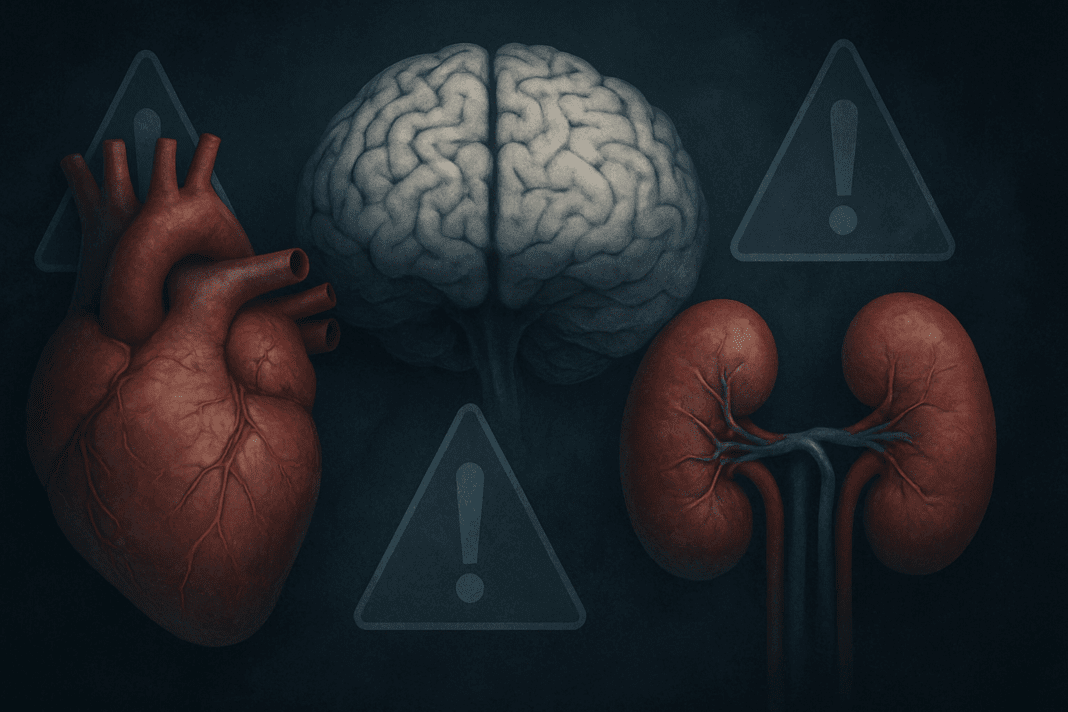
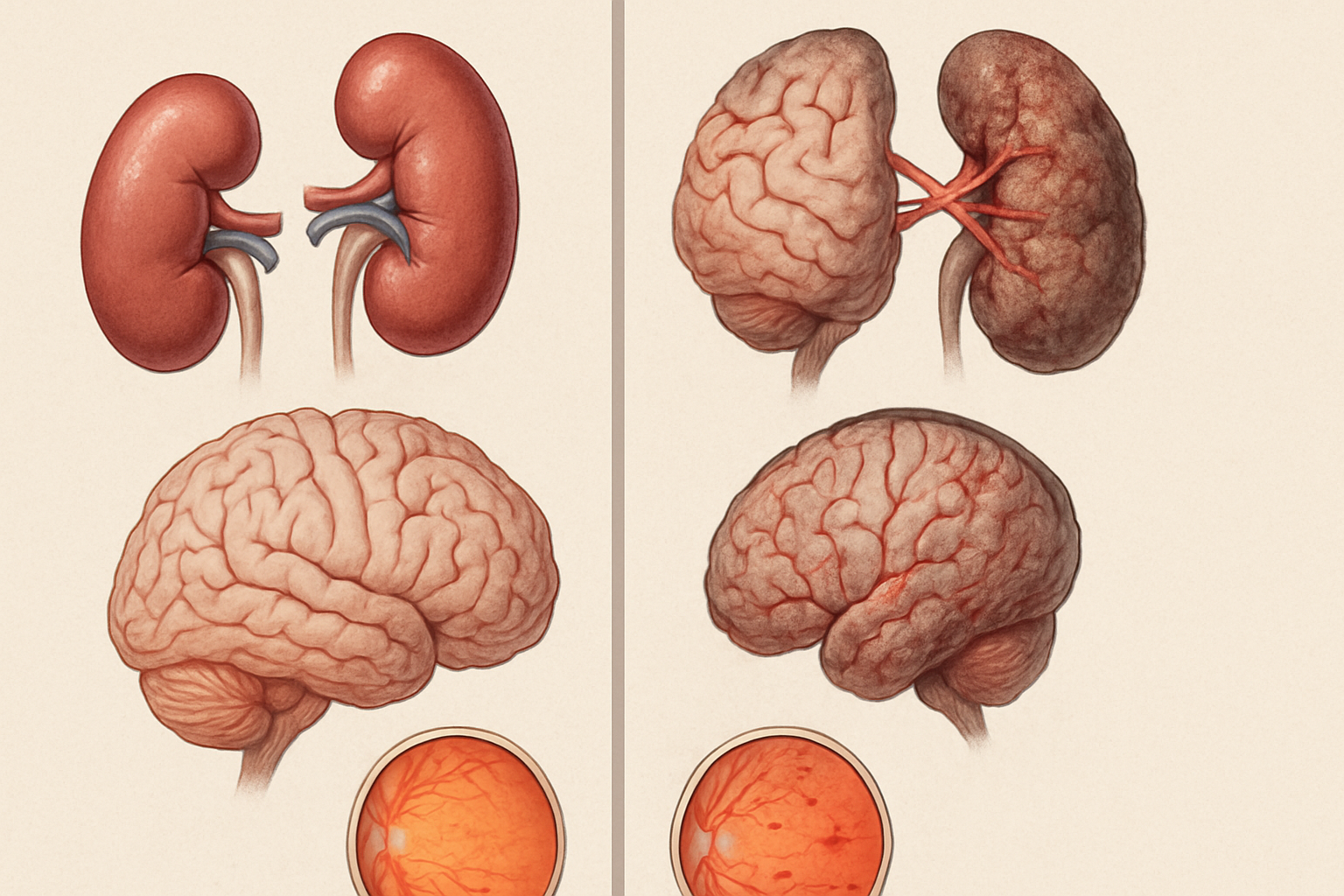
Beyond the cardiovascular system, high blood pressure exerts a destructive influence on multiple organ systems. Chronic hypertension can damage the kidneys, impairing their ability to filter waste and regulate fluid balance, which may ultimately lead to kidney failure. It can affect the brain by weakening blood vessels, increasing the risk of both ischemic and hemorrhagic strokes, and contributing to cognitive decline and dementia over time.
The eyes are another vulnerable target. Hypertension can damage the blood vessels in the retina, a condition known as hypertensive retinopathy, which can cause vision problems or even blindness. These examples underscore why hypertension is called the silent killer—it launches a stealthy, multi-systemic assault that may not be evident until irreversible damage has been done.
The Public Health Burden of the Silent Killer
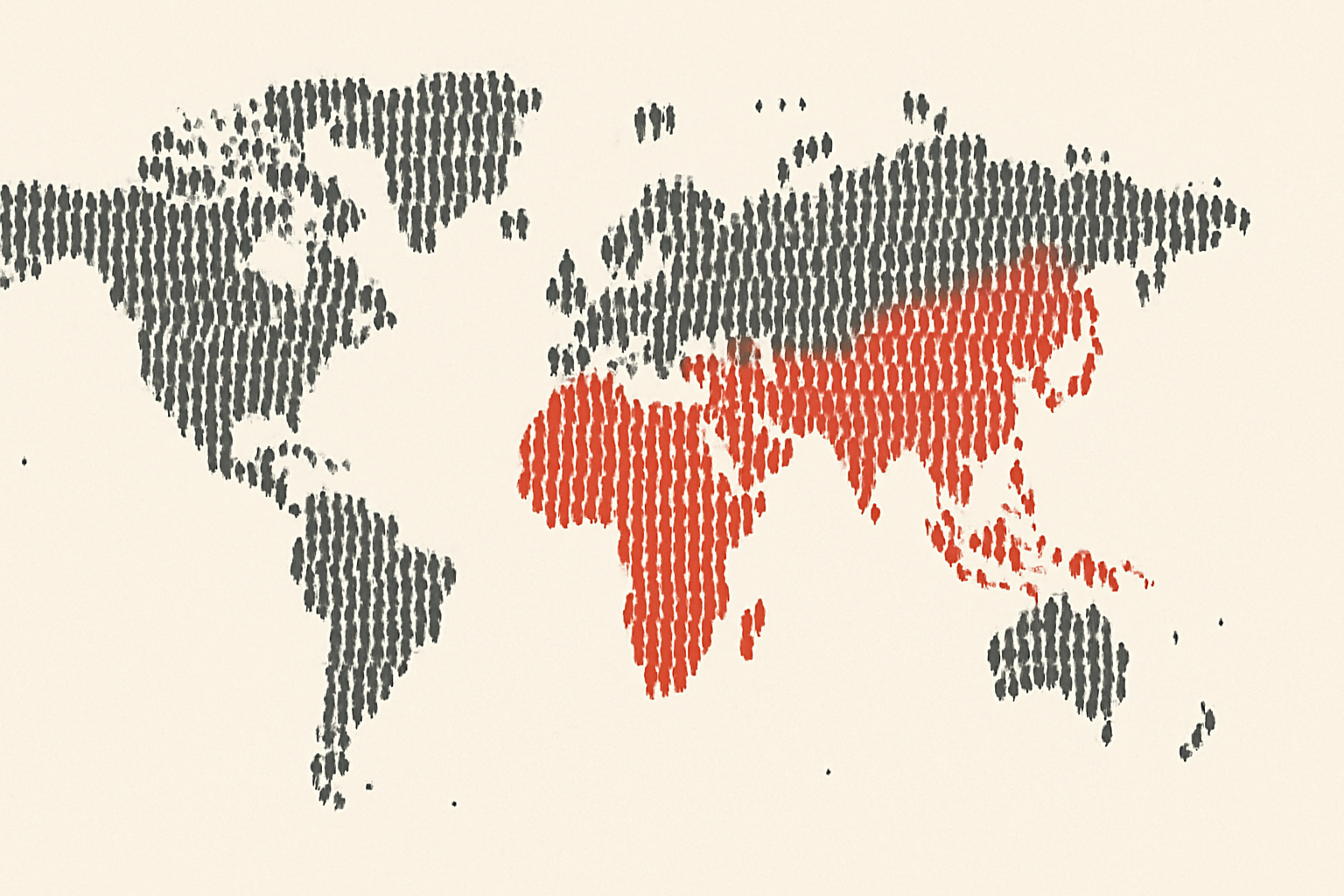
The implications of labeling hypertension as the silent killer extend beyond individual cases. From a public health perspective, hypertension is one of the leading risk factors for premature death worldwide. The World Health Organization (WHO) estimates that over 1.28 billion adults globally have high blood pressure, and a significant proportion of them are unaware of their condition. This widespread lack of awareness is part of what makes high blood pressure the silent killer in so many societies.
In low- and middle-income countries, the burden is even more pronounced due to limited access to preventive care, diagnostic services, and essential medications. Even in more developed healthcare systems, socioeconomic disparities can lead to unequal detection and treatment of this silent killer disease. The need for widespread public education, early screening programs, and accessible treatment options has never been more urgent.
Why Is Hypertension Known as the Silent Killer Among Clinicians?
Clinicians often describe hypertension as the silent killer because of the frequency with which it leads to severe complications in patients who had no prior warning signs. Primary care physicians, cardiologists, nephrologists, and neurologists alike encounter patients who present with heart attacks, strokes, kidney dysfunction, or cognitive impairment, only to discover that unrecognized and untreated hypertension was a key contributing factor.
This clinical reality reinforces the need for routine blood pressure monitoring as a core element of preventive medicine. Many professional guidelines recommend that adults, especially those over the age of 40 or with risk factors such as obesity, diabetes, or a family history of heart disease, have their blood pressure checked at least once a year. Understanding why is hypertension known as the silent killer can galvanize both clinicians and patients to take blood pressure seriously, even in the absence of outward symptoms.
Risk Factors That Worsen the Silent Threat
Several modifiable and non-modifiable risk factors can elevate an individual’s chances of developing high blood pressure. Age, genetics, and family history are beyond one’s control, but lifestyle factors play a critical role. Diets high in sodium and saturated fats, physical inactivity, smoking, excessive alcohol consumption, and chronic stress all contribute to hypertension. Obesity and metabolic disorders such as type 2 diabetes are also closely linked to high blood pressure.
Addressing these risk factors through targeted interventions can help individuals avoid becoming victims of the silent killer. For instance, adopting a DASH (Dietary Approaches to Stop Hypertension) diet, engaging in regular aerobic exercise, limiting alcohol intake, and managing stress through mindfulness or therapy can all significantly lower blood pressure. These proactive measures are not only effective but essential for preventing the hidden dangers of hypertension.
The Role of Regular Monitoring and Early Detection
Given the asymptomatic nature of hypertension, regular monitoring is one of the most important tools in combating the blood pressure silent killer. Home blood pressure monitors are now widely available, affordable, and easy to use, allowing individuals to keep track of their cardiovascular health from the comfort of their homes. For those with risk factors or borderline readings, ambulatory blood pressure monitoring—where readings are taken over 24 hours during regular activities—can provide a more accurate picture than a single measurement taken in a clinical setting.
Public health campaigns emphasizing the importance of knowing one’s numbers have proven effective in increasing awareness and early diagnosis. In many cases, lifestyle changes initiated at the first signs of elevated blood pressure can prevent the condition from progressing to more severe stages. This approach is vital in reducing the toll taken by the high blood pressure silent killer on both individual health and healthcare systems.
Treatment Options and Advances in Hypertension Management
While lifestyle changes are foundational, many individuals with high blood pressure also require pharmacologic treatment. A wide range of antihypertensive medications are available today, including diuretics, ACE inhibitors, angiotensin receptor blockers, calcium channel blockers, and beta-blockers. The selection of medications is personalized, taking into account the patient’s age, comorbidities, and specific cardiovascular risk profile.
Recent advancements in precision medicine have led to more tailored approaches, such as using genetic data to inform drug choices or combining medications in fixed-dose formulations to improve adherence. These innovations, along with mobile health technologies and digital monitoring platforms, are reshaping the landscape of hypertension care. As treatment becomes more patient-centered and proactive, we inch closer to neutralizing the effects of what is the silent killer medical communities continue to battle on a global scale.
The Connection Between Mental Health and Hypertension
An often-overlooked aspect of hypertension is its complex relationship with mental health. Chronic stress, anxiety, and depression can contribute to elevated blood pressure through hormonal and behavioral mechanisms. Stress hormones like cortisol and adrenaline increase heart rate and constrict blood vessels, raising blood pressure. Over time, these physiological responses can become chronic and harmful.
Conversely, living with a diagnosis of hypertension can also affect mental well-being. Patients may experience anxiety about their health, especially when faced with lifestyle restrictions or side effects from medication. Addressing this bidirectional relationship is essential for holistic management. Cognitive-behavioral therapy, stress-reduction techniques, and psychosocial support can complement medical treatments, providing a more comprehensive approach to defeating the silent killer disease.
Hypertension in Special Populations
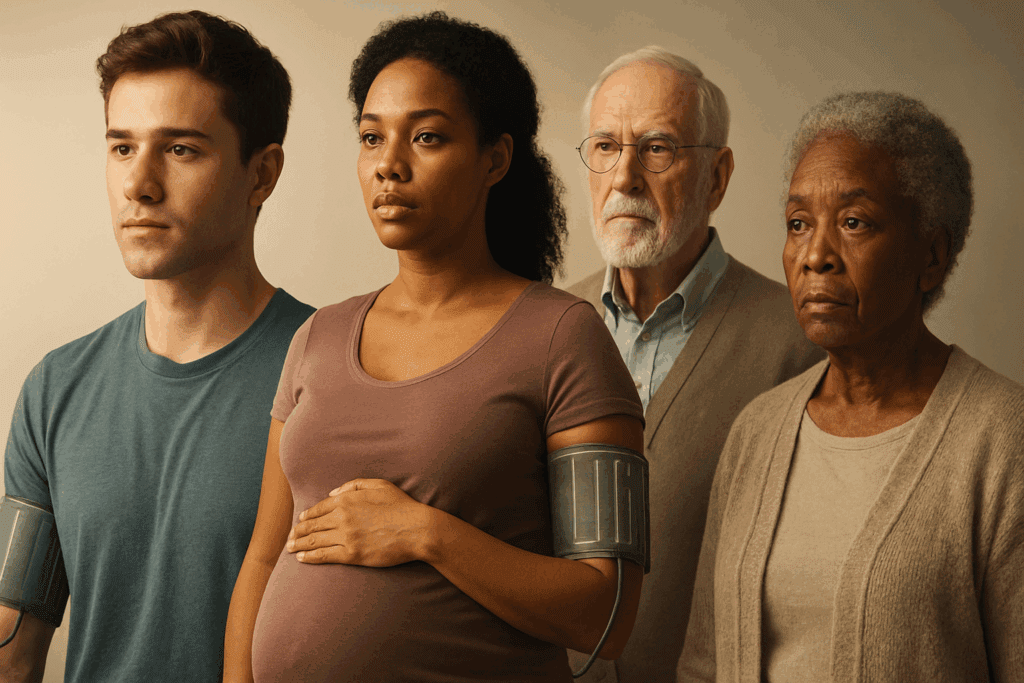
Certain populations are at heightened risk for developing complications from high blood pressure. Older adults, for example, are more susceptible due to age-related vascular changes and coexisting chronic conditions. Pregnant women can develop a specific type of high blood pressure known as preeclampsia, which poses risks to both mother and fetus.
Racial and ethnic disparities also play a role. African American individuals, in particular, tend to develop hypertension at earlier ages and experience more severe complications. Understanding these demographic differences is key to designing effective prevention and intervention strategies. Targeted education, culturally competent care, and community-based initiatives are essential in curbing the disproportionate impact of the blood pressure silent killer on vulnerable groups.
Reframing the Narrative: Empowering Patients Through Education
To dismantle the lethal potential of hypertension, we must move beyond the language of fear and towards a model of empowerment. Educating patients about what is the silent killer medical professionals caution against means giving them the knowledge and tools they need to take control of their health. This includes understanding how lifestyle choices affect blood pressure, recognizing early warning signs, and knowing when to seek medical advice.
Patient-centered care models that emphasize shared decision-making, personalized goal-setting, and ongoing support have been shown to improve adherence to treatment and outcomes. When individuals are equipped with accurate information and a supportive healthcare team, they are better positioned to overcome the silent threats posed by uncontrolled blood pressure.
Frequently Asked Questions: Understanding High Blood Pressure as the Silent Killer
1. Can emotional and psychological stress trigger the silent killer effect of high blood pressure?
Yes, psychological stress can play a powerful but underestimated role in the development and worsening of high blood pressure, further cementing its reputation as the silent killer. Chronic emotional strain can lead to prolonged elevations in cortisol and adrenaline, hormones that constrict blood vessels and raise heart rate, increasing blood pressure over time. Unlike acute stress, which resolves quickly, chronic stress can lead to vascular inflammation and endothelial dysfunction, which are precursors to cardiovascular events. This explains why high blood pressure is known as the silent killer, as individuals may internalize stress without noticing the physiological consequences. Prolonged mental strain without visible symptoms exemplifies what is the silent killer medical professionals warn about in modern high-stress lifestyles.
2. How do wearable technologies contribute to early detection of the silent killer disease?
Wearable technologies have evolved into critical tools in identifying and managing what is widely considered the silent killer medical threat—hypertension. Devices like smartwatches and fitness trackers with blood pressure monitoring capabilities allow for continuous observation of cardiovascular data, enabling users to detect trends rather than relying on one-off clinic readings. This form of passive surveillance can reveal masked hypertension or white coat syndrome, helping to address hidden patterns. These technologies are reshaping the narrative around why is high blood pressure called the silent killer by enabling earlier interventions before clinical symptoms arise. In many ways, wearables represent a proactive response to the blood pressure silent killer that once depended solely on sporadic clinical testing.
3. How does hypertension’s impact differ in men and women?
Hypertension affects men and women differently, not just in prevalence but also in how the disease progresses and presents. While men are more likely to develop high blood pressure earlier in life, women—especially postmenopausal—face increased cardiovascular risks due to hormonal changes and less protective estrogen levels. These sex-based differences have prompted researchers to revisit why is hypertension known as the silent killer in both populations. For women, symptoms may be more subtle or atypical, and they are often underdiagnosed or misdiagnosed, contributing to the silent killer effect. Recognizing these differences is vital in addressing what is the silent killer medical literature often underrepresents in female populations.
4. Are younger adults at risk of developing the silent killer disease?
Contrary to the outdated belief that hypertension is exclusive to older adults, recent data reveal a rising prevalence among people in their 20s and 30s. Sedentary lifestyles, poor dietary choices, increased stress, and high sodium intake are contributing to early-onset hypertension. Because these individuals typically feel healthy and show no symptoms, their condition often remains undiagnosed—emphasizing why is hypertension called the silent killer even in youthful demographics. Early exposure to high blood pressure can accelerate vascular damage and increase lifetime cardiovascular risk, making early education and screening essential. As the face of the silent killer disease changes, so too must our approach to awareness and prevention.
5. How does social isolation influence the risk of hypertension as a silent killer?
Social isolation and loneliness are emerging as significant but underrecognized risk factors for high blood pressure and cardiovascular disease. Individuals lacking strong social support are more likely to experience chronic stress, poor sleep, and unhealthy lifestyle habits—all of which elevate the risk of developing hypertension. This aligns with why is high blood pressure known as the silent killer, as the psychological and behavioral effects of isolation often occur without outward symptoms. Medical researchers are increasingly viewing social well-being as a critical factor in the battle against the silent killer. Addressing loneliness and community disconnection may become an essential strategy in preventing the high blood pressure silent killer from progressing unnoticed.
6. Are there genetic markers that predispose individuals to the blood pressure silent killer?
Genetic research has identified several polymorphisms associated with salt sensitivity, vascular stiffness, and hormonal regulation that predispose individuals to hypertension. Those with a family history of the condition may carry gene variants that influence the renin-angiotensin-aldosterone system (RAAS), leading to higher baseline blood pressure levels. Understanding these inherited risks sheds new light on why is hypertension known as the silent killer—it can begin its course silently from birth. Genetic testing may help stratify risk earlier, allowing for targeted prevention strategies even before clinical hypertension manifests. This molecular insight provides a deeper layer to what is the silent killer medical professionals now approach with a more personalized lens.
7. Can untreated sleep disorders contribute to the effects of the silent killer?
Absolutely. Obstructive sleep apnea (OSA) is a prime example of a sleep disorder that significantly increases the risk of hypertension by disrupting normal breathing and causing repeated oxygen deprivation during sleep. These episodes trigger sympathetic nervous system activation, raising nighttime and daytime blood pressure. Because many individuals with OSA are unaware of their condition, this contributes to why is high blood pressure called the silent killer. Treating sleep apnea with CPAP therapy has been shown to reduce blood pressure and lower cardiovascular risks, making sleep health an important target in combating the silent killer disease. Integrating sleep assessments into routine screenings can help unmask this hidden contributor to the blood pressure silent killer.
8. How do environmental and socioeconomic factors shape the prevalence of the silent killer?
Access to healthy food, safe environments for exercise, affordable healthcare, and education all play pivotal roles in managing or preventing hypertension. Individuals in lower socioeconomic brackets are disproportionately exposed to chronic stress, environmental pollutants, and dietary challenges, all of which compound the risk of developing undiagnosed high blood pressure. This makes the high blood pressure silent killer particularly insidious in marginalized communities where preventive care is often underutilized or unavailable. Understanding why is hypertension called the silent killer requires examining these social determinants of health, which shape who gets diagnosed, treated, and ultimately who survives. Structural interventions must address these disparities if the silent killer disease is to be effectively countered.
9. How might future innovations help defeat the silent killer?
Future approaches to hypertension management may include AI-driven diagnostics, personalized medication algorithms, and digital therapeutics that use behavioral nudges to encourage lifestyle change. These technologies aim to detect early blood pressure trends and offer tailored interventions long before symptoms arise. Advancements in microbiome science also hint at potential probiotic therapies that could influence blood pressure regulation through gut health. As we redefine what is the silent killer medical response should be, these forward-looking tools represent hope for shifting from reactive care to predictive, preventive medicine. Empowering individuals with such innovations could transform how the blood pressure silent killer is managed in both clinical and community settings.
10. Why is global awareness essential in addressing the silent killer disease?
Despite being highly treatable, hypertension remains the leading preventable cause of death worldwide. However, global awareness about why is high blood pressure called the silent killer is still lacking, especially in low-resource regions. Many individuals are never screened or treated due to cultural, economic, or systemic barriers. International collaborations that provide funding, education, and infrastructure are critical to combating what is the silent killer medical challenge across populations. A globally unified response that respects cultural contexts while promoting universal access to care is vital for dismantling the silent killer disease on a worldwide scale.
Final Thoughts: Confronting the Silent Killer With Awareness and Action
In the face of a disease that operates in silence, awareness becomes our most powerful weapon. The reason why is high blood pressure called the silent killer is not just a medical mystery, but a public health challenge that demands collective attention. Through a combination of education, routine screening, lifestyle change, and advanced medical care, we can interrupt hypertension’s quiet devastation.
Let this understanding be a call to action—for individuals to monitor their blood pressure regularly, for clinicians to maintain vigilance even in asymptomatic patients, and for communities to prioritize cardiovascular health. High blood pressure may be silent, but with knowledge and proactive care, we can ensure that it is no longer deadly. By addressing why is hypertension called the silent killer with informed, compassionate responses, we take a crucial step in saving lives and building a healthier future for all.
hypertension management strategies, cardiovascular health tips, heart disease prevention, managing blood pressure naturally, early signs of cardiovascular risk, lifestyle changes for heart health, silent symptoms of chronic illness, kidney damage from hypertension, vascular health awareness, stroke prevention techniques, holistic heart health, lifestyle risk factors for heart disease, high sodium diet effects, chronic disease without symptoms, public health and hypertension, community health screenings, stress and cardiovascular risk, wearable health tech, personalized heart care, undiagnosed medical conditions
Further Reading:
Why High Blood Pressure Is Known as the Silent Killer
High Blood Pressure: Why It’s Called the ‘Silent Killer’
Hypertension Is Known as the Silent Killer, and Here’s What You Need to Know