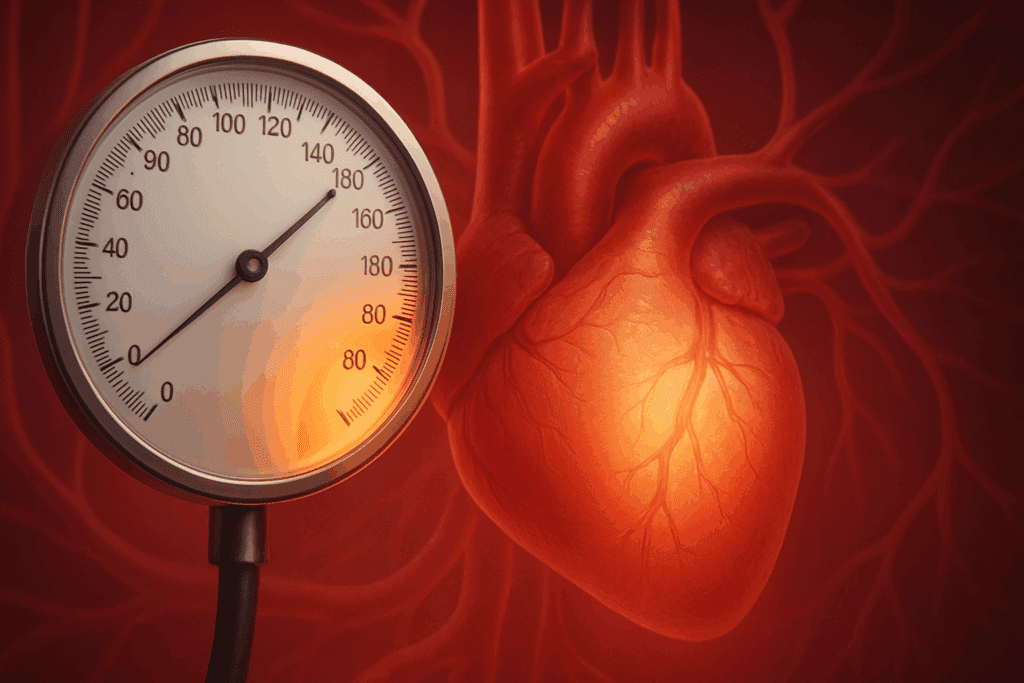
High blood pressure, or hypertension, is one of the most common and consequential health issues affecting people worldwide. While much public attention is given to the top number—systolic pressure—the bottom number, known as diastolic pressure, is equally important and often overlooked. Elevated diastolic blood pressure can be a subtle but significant indicator of cardiovascular dysfunction. When patients ask, “Why is my diastolic pressure high?” they are often unaware that this seemingly minor metric can have profound implications for their long-term health.
Understanding what causes high diastolic blood pressure is essential for early diagnosis, appropriate intervention, and effective management. This article delves into the key reasons behind increased diastolic blood pressure, its potential risks, and the clinical significance of having the bottom number of blood pressure high. Drawing from current medical research and clinical guidelines, we will also explore the concept of diastolic hypertension, why diastolic readings rise independently, and what elevated diastolic blood pressure means for your heart and overall health.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Defining Blood Pressure and the Role of Diastolic Values
Blood pressure is measured in millimeters of mercury (mmHg) and presented as two numbers: systolic over diastolic. The systolic value measures the pressure in your arteries when your heart beats, while the diastolic value reflects the pressure when your heart is at rest between beats. In general, a normal blood pressure reading is considered to be around 120/80 mmHg, though optimal values may vary slightly depending on individual risk factors and clinical circumstances.
When the diastolic number is consistently 90 mmHg or higher, this may be classified as diastolic hypertension. In some cases, the systolic value may remain within the normal range, a condition known as isolated diastolic hypertension. This condition is especially relevant in younger adults and may indicate early vascular changes that precede full-blown hypertension. Understanding what causes high diastolic blood pressure involves recognizing how vascular resistance, arterial stiffness, and other physiological changes impact the pressure during the heart’s resting phase.
What Does High Diastolic Blood Pressure Mean?
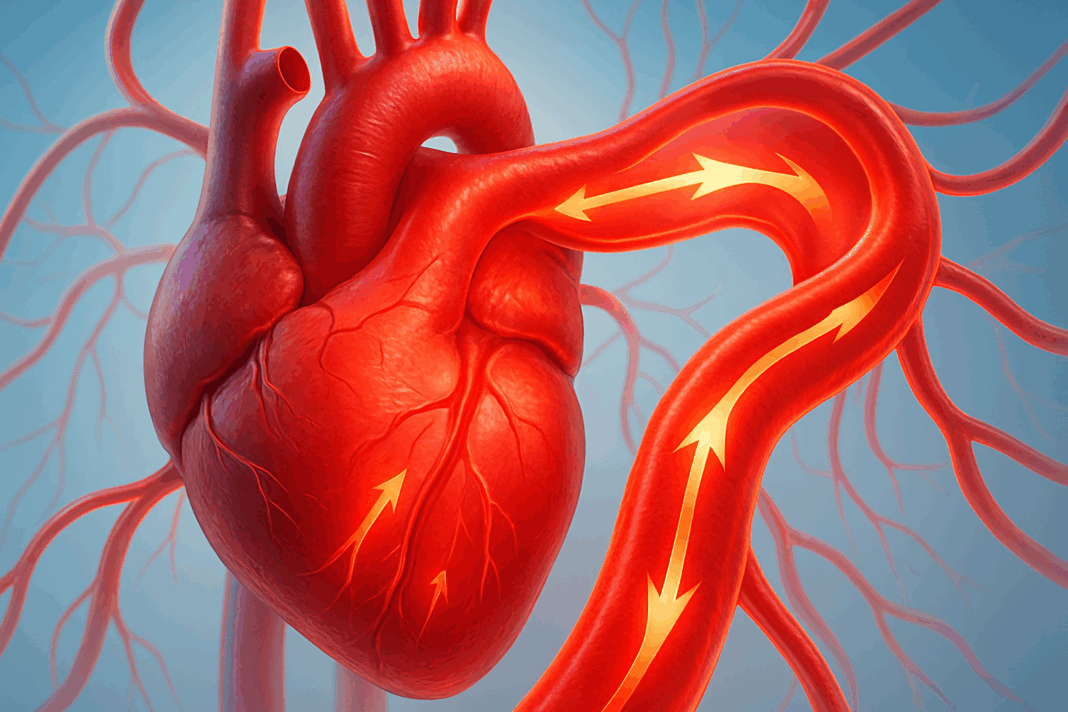
Many individuals assume that if their systolic number is within the normal range, they are in good cardiovascular health. However, this assumption can be misleading. What does high diastolic blood pressure mean in clinical practice? It often suggests that the arteries are not relaxing adequately between heartbeats, which can increase the workload on the heart over time. This can be a precursor to more generalized hypertension, or it may exist independently, posing distinct risks.
High diastolic blood pressure may reflect increased peripheral vascular resistance, early stages of atherosclerosis, or sympathetic nervous system overactivity. In some individuals, especially those under age 50, the bottom blood pressure number being high may indicate a heightened risk for future cardiovascular complications, even if the systolic number appears normal. Therefore, knowing what high diastolic pressure means is crucial for appropriate monitoring and early intervention.
What Causes High Diastolic BP?
There are several physiological and lifestyle-related reasons for increased diastolic blood pressure. One primary cause is chronic vascular resistance—a condition in which the small arteries become constricted, reducing their capacity to dilate properly. This leads to sustained pressure during the heart’s resting phase. Hormonal factors, such as elevated levels of adrenaline and cortisol, can also raise diastolic readings by stimulating vasoconstriction.
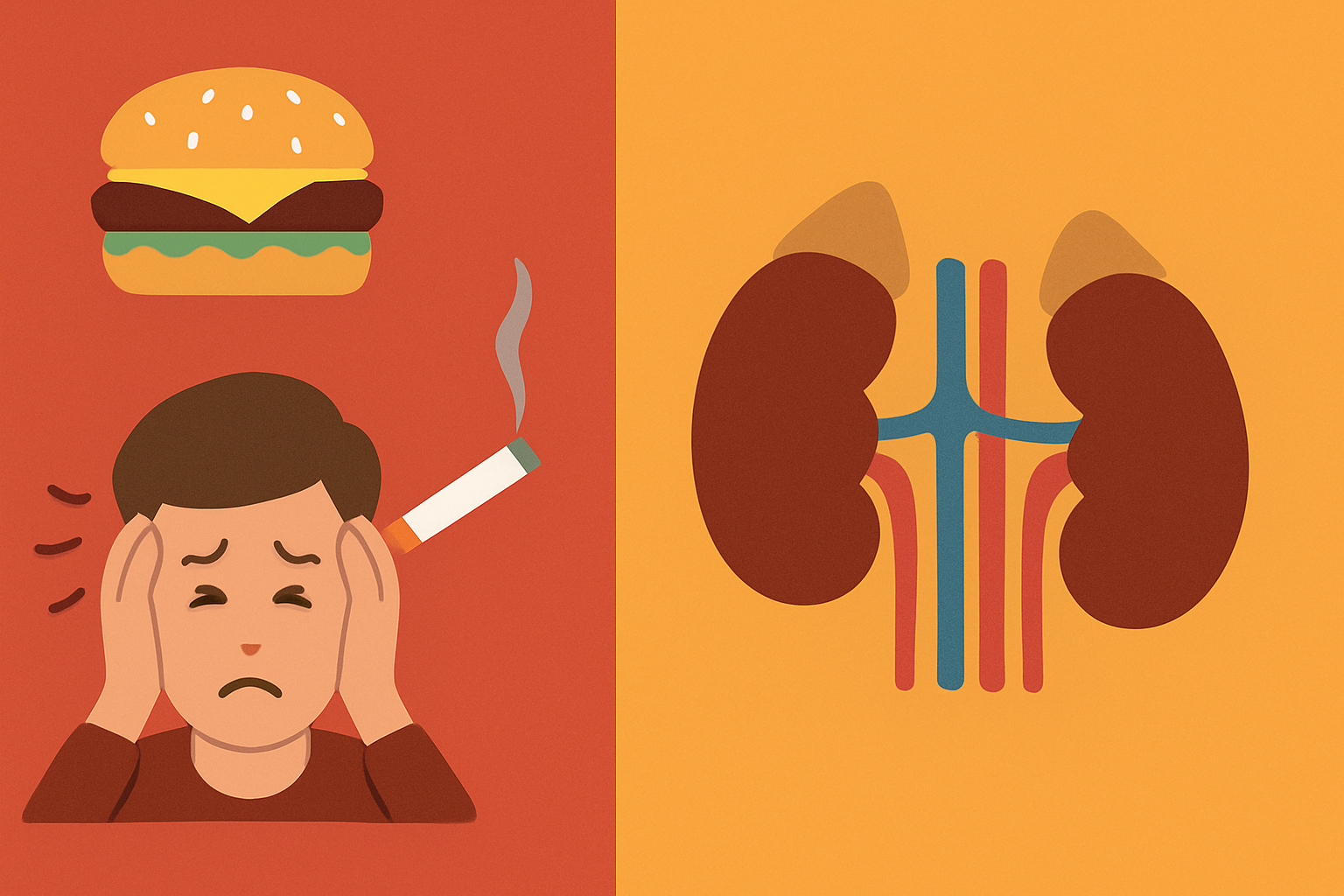
Lifestyle factors, including excessive sodium intake, obesity, smoking, and sedentary behavior, can contribute significantly to elevated diastolic blood pressure. Alcohol consumption, particularly in excess, has been associated with increased diastolic values due to its impact on the autonomic nervous system and fluid balance. Stress and anxiety, too, are frequently overlooked contributors that can influence vascular tone and thus affect the bottom blood pressure number.
Endocrine disorders like hyperthyroidism or adrenal tumors can also be culprits, and so can renal diseases that disrupt the kidney’s ability to regulate blood volume and vascular tone. When evaluating what causes bottom number of blood pressure to be high, healthcare providers often investigate these underlying conditions to determine whether medical treatment or lifestyle modification is most appropriate.
Dangers of High Diastolic Blood Pressure
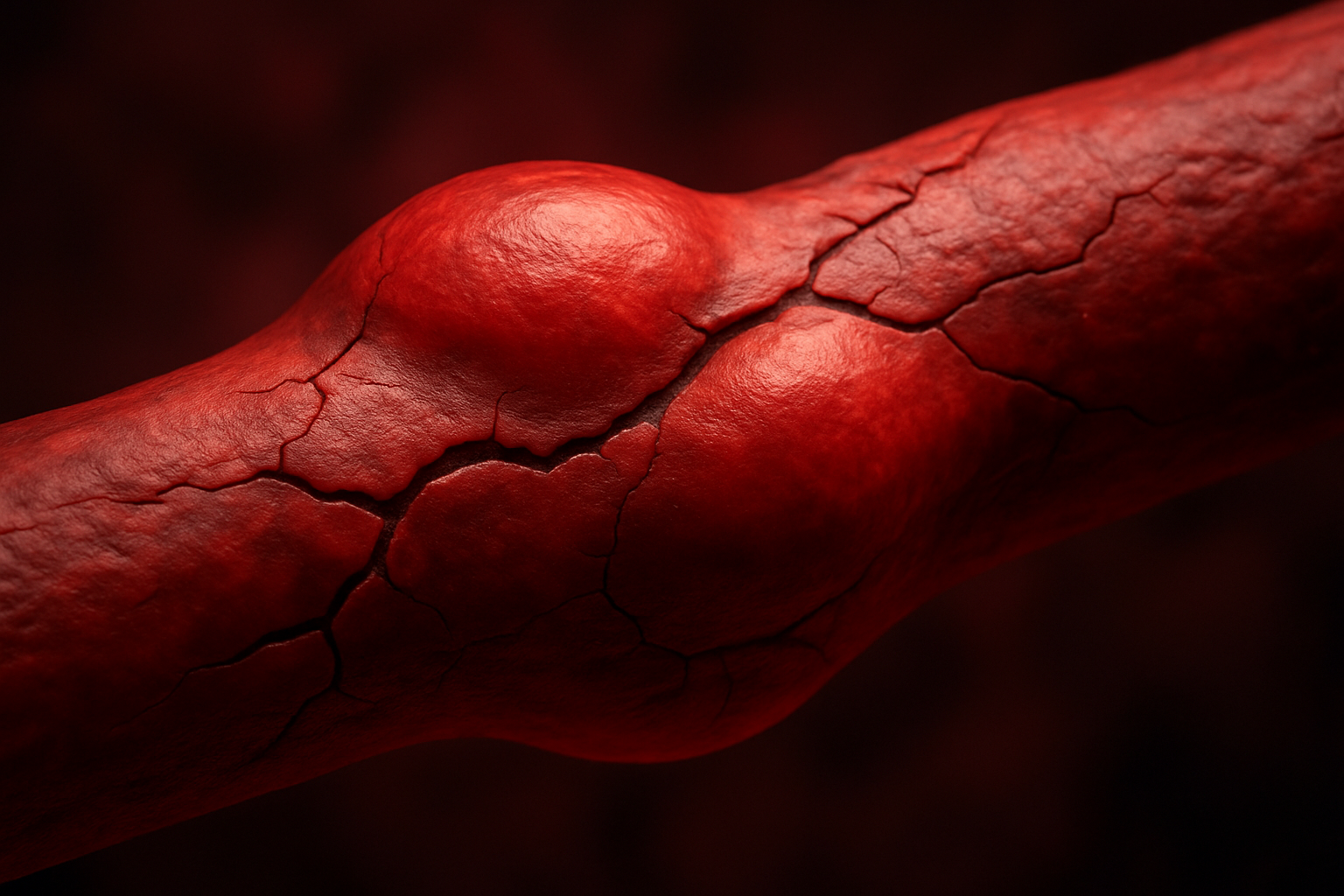
While many people are familiar with the dangers of high systolic blood pressure, the risks associated with high diastolic pressure are less frequently discussed. Yet the dangers of high diastolic blood pressure are real and potentially serious. Elevated diastolic readings can place continuous strain on the arterial walls, increasing the risk of arterial damage, aneurysm formation, and eventual cardiovascular events.
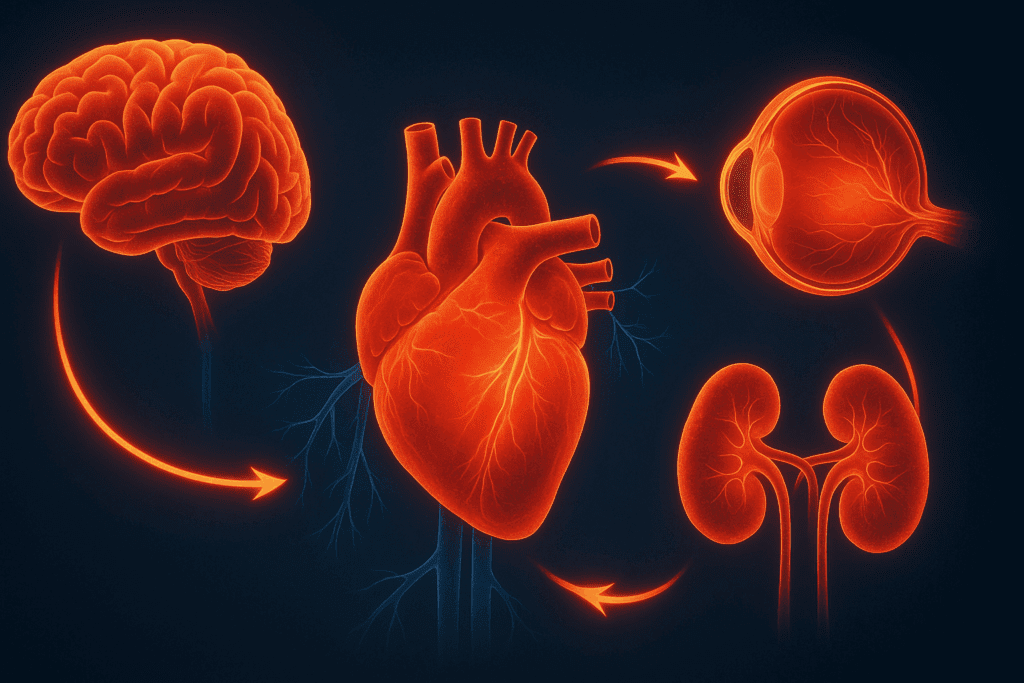
Sustained diastolic hypertension may impair coronary artery perfusion, particularly during diastole, which is the only time the heart muscle itself receives blood. This can lead to myocardial ischemia and increase the risk of heart attacks, especially in individuals who already have underlying coronary artery disease. Over time, the heart may respond to this increased workload by undergoing hypertrophy—thickening of the heart muscle—which can progress to heart failure if left unchecked.
Additionally, the microvascular systems in organs like the kidneys, brain, and eyes are highly sensitive to pressure changes. Elevated diastolic blood pressure can exacerbate chronic kidney disease, contribute to cognitive decline, and increase the risk of hypertensive retinopathy. These outcomes underscore why it is so important to understand the dangers associated with raised diastolic pressure and to take timely steps to mitigate them.
Isolated Diastolic Hypertension: A Unique Clinical Picture
In some individuals, especially those under 50 years of age, diastolic hypertension can occur without a corresponding increase in systolic pressure. This condition, known as isolated diastolic hypertension, presents a unique clinical challenge. The mechanisms underlying this phenomenon are not yet fully understood, but several theories point to increased sympathetic activity, early arterial stiffness, or hormonal imbalances.
One of the challenges in managing isolated diastolic BP is that it often goes unnoticed in routine screenings. Physicians may focus primarily on the systolic value, inadvertently overlooking the bottom number when it falls just above the threshold. However, when the blood pressure bottom number is high, even in isolation, it can serve as an early warning sign of vascular dysfunction. Studies have suggested that individuals with isolated diastolic hypertension may be at increased risk for developing full-spectrum hypertension in the future, particularly if lifestyle risk factors are not addressed.
Patients who are told their diastolic BP is elevated may question what this means in the context of their overall health. What does high diastolic BP indicate in such cases? It may point to an imbalance in autonomic regulation or a pre-hypertensive state that warrants close monitoring and proactive intervention.
Which Blood Pressure Number Is More Important?
The question of which blood pressure number is more important—systolic or diastolic—has long been debated among clinicians. While both numbers carry clinical significance, recent research has highlighted that the relative importance of each can vary depending on age, comorbidities, and individual cardiovascular risk profiles. In older adults, systolic hypertension has been more closely associated with stroke, heart attack, and cognitive decline. In contrast, for younger individuals, a high diastolic reading may be more predictive of long-term risk.
That said, dismissing an elevated diastolic blood pressure reading as clinically irrelevant would be a mistake. High diastolic pressure, particularly when sustained over time, can be a harbinger of future cardiovascular disease. Recognizing why diastolic is high in a specific patient is key to providing targeted treatment and prevention strategies. This is especially important for individuals with other risk factors, such as diabetes, smoking, or a family history of hypertension or heart disease.

Reasons for High Diastolic Pressure: Exploring Contributing Factors
The reasons for high diastolic pressure are diverse and multifactorial. Genetics play a significant role, as a family history of hypertension can predispose individuals to elevated diastolic readings. Environmental factors, including dietary habits, physical activity levels, and sleep quality, also contribute. For instance, insufficient potassium and magnesium intake can impair vascular relaxation, contributing to increased peripheral resistance and higher diastolic values.
Medications, both prescription and over-the-counter, can also influence diastolic readings. Nonsteroidal anti-inflammatory drugs (NSAIDs), decongestants, and some antidepressants have been linked to elevated diastolic blood pressure. Hormonal contraceptives and certain weight-loss supplements may similarly affect vascular tone. Understanding the interplay of these factors is essential when evaluating what causes bottom number of BP to be high in a given patient.
In some cases, high diastolic blood pressure may be secondary to sleep disorders such as obstructive sleep apnea (OSA), which leads to intermittent hypoxia and sympathetic nervous system activation. Chronic inflammation, poor glycemic control in diabetics, and exposure to environmental toxins like lead or mercury are other potential contributing factors. Each of these elements must be considered carefully when assessing the broader picture of elevated diastolic blood pressure causes.
What Does It Mean When Diastolic Is High?
When patients encounter a high diastolic number on their blood pressure readings, they often wonder what it means in practical terms. What does it mean when diastolic is high? In essence, it means that the blood vessels are experiencing elevated pressure even when the heart is at rest. This persistent pressure can erode the integrity of the vascular walls, compromise organ perfusion, and lead to long-term damage if left unaddressed.
Clinically, an elevated diastolic BP may also serve as a biomarker for systemic inflammation, endothelial dysfunction, or hormonal imbalance. It may reflect early signs of cardiovascular remodeling, particularly in individuals with comorbid conditions such as obesity or insulin resistance. By the time symptoms appear—such as fatigue, headaches, or palpitations—the underlying pathology may already be advanced. This highlights the importance of regular monitoring and timely interpretation of diastolic readings.
Why Is My Bottom BP Number High?
Many people discover during routine checkups that their diastolic blood pressure is higher than normal and naturally wonder, “Why is my bottom BP number high?” The answer to this question can vary significantly depending on the individual. For some, it may be a temporary response to stress, poor sleep, or caffeine intake. For others, it may signal the beginning of a chronic condition requiring ongoing management.
Accurate diagnosis involves more than just one isolated reading. Physicians typically recommend ambulatory blood pressure monitoring or home-based readings taken over a period of days to assess whether elevated values persist. Laboratory tests, imaging studies, and lifestyle assessments can help determine the underlying reasons for high diastolic BP. Often, a combination of factors—including genetics, diet, physical activity, and mental health—come together to produce sustained elevations in diastolic pressure.
Understanding why diastolic BP is elevated is critical not only for diagnosis but also for crafting an effective treatment plan. This may include lifestyle interventions such as dietary modifications, increased physical activity, weight loss, and stress reduction techniques, as well as pharmacological treatment when necessary.
Frequently Asked Questions (FAQ): High Diastolic Blood Pressure
1. Can high diastolic blood pressure affect younger adults differently than older individuals?
Yes, high diastolic blood pressure often presents unique concerns in younger adults compared to older individuals. In younger patients, an elevated diastolic reading may be an early warning sign of future vascular disease rather than an indication of existing arterial stiffness, which is more common in older adults. Since younger people typically have more elastic arteries, an increased diastolic BP can signal heightened sympathetic nervous system activity, chronic stress exposure, or early metabolic imbalances. Recognizing what causes high diastolic blood pressure in younger adults can help prevent its progression to full hypertension. Proactive lifestyle adjustments and early screening are essential in this age group to mitigate long-term cardiovascular risks.
2. Why might my diastolic pressure remain high even if I’m following a healthy lifestyle?
It can be frustrating when elevated diastolic blood pressure persists despite good health habits. In such cases, hidden or genetic factors may be at play. Hormonal imbalances, undiagnosed kidney disease, or subtle sleep disorders like sleep apnea can all contribute to increased diastolic BP. Additionally, some individuals have a genetic predisposition to higher vascular tone or a stronger vasoconstrictive response, which makes managing hypertension diastolic high more complex. Understanding what is the reason for high diastolic blood pressure in such cases may require specialized diagnostic testing beyond standard check-ups.
3. Are there environmental or occupational factors that can raise the diastolic number?
Absolutely. Environmental stressors and workplace conditions can significantly affect cardiovascular health, including raising the blood pressure bottom number. Prolonged exposure to noise pollution, shift work, high-stress occupations, or exposure to industrial chemicals can lead to a chronically activated stress response. This persistent stimulation of the sympathetic nervous system may lead to diastolic hypertension over time. When evaluating what causes bottom number of blood pressure to be high, these contextual factors are often overlooked, yet they play a pivotal role in long-term health outcomes. Identifying and mitigating these influences can be crucial in controlling diastolic BP.
4. How does poor sleep quality contribute to diastolic BP elevation?
Sleep quality is a lesser-discussed but critical factor in blood pressure regulation. Inadequate or fragmented sleep can disrupt the body’s ability to recover from daily stressors, leading to elevated diastolic blood pressure. Conditions like insomnia or obstructive sleep apnea may keep the sympathetic nervous system active during the night, leading to increased vascular resistance. This sustained physiological arousal can result in raised diastolic pressure by morning. When exploring elevated diastolic blood pressure causes, a sleep study may be warranted, especially if lifestyle changes have not led to improvements.
5. Is it possible to experience symptoms specifically from high diastolic pressure?
While high diastolic pressure is often asymptomatic, some individuals may notice subtle signs when their bottom BP is high. These might include early morning headaches, persistent fatigue, shortness of breath with exertion, or even mild chest discomfort. These symptoms are usually vague and can be easily attributed to other conditions, which is why diastolic BP elevated levels may go undetected for years. However, they can be an indication that the vascular system is under strain. Recognizing what does high diastolic blood pressure mean in the presence of symptoms requires a nuanced approach and careful clinical evaluation.
6. How does mental health impact diastolic blood pressure over time?
Chronic mental health challenges, such as anxiety and depression, are increasingly recognized as contributing factors to sustained high diastolic blood pressure. These conditions can lead to a dysregulated hypothalamic-pituitary-adrenal (HPA) axis, resulting in long-term elevations in cortisol and adrenaline. These hormones increase vascular tone and contribute to what causes high diastolic pressure even in individuals who appear physically healthy. Moreover, emotional distress can lead to unhealthy coping mechanisms such as overeating, alcohol use, or physical inactivity, all of which worsen the condition. Understanding what high diastolic pressure means in the context of mental health can enhance treatment plans.
7. What is the significance of isolated diastolic hypertension in long-term cardiovascular risk?
Isolated diastolic BP elevation, where only the bottom number is high, has been debated in clinical circles but is gaining attention due to its implications. Although initially considered less concerning than systolic elevation, research shows that isolated diastolic hypertension can increase the risk of heart failure and chronic kidney disease if left untreated. The condition often indicates subtle changes in vascular elasticity and autonomic nervous system regulation. Understanding what does high diastolic BP indicate in isolation helps clinicians identify early intervention opportunities. Tailored treatment approaches are often necessary to prevent progression to combined hypertension.
8. Can high diastolic blood pressure affect organ function even if systolic pressure is normal?
Yes, high diastolic blood pressure can impair organ function independently of systolic values. The kidneys, brain, and eyes are particularly vulnerable to the effects of sustained vascular pressure. Elevated diastolic pressure can reduce perfusion efficiency, contributing to cognitive issues, vision disturbances, or worsening kidney filtration. This illustrates why it is not only systolic but also diastolic pressure that matters when assessing overall risk. Knowing which blood pressure number is more important depends on the organ system in question and the patient’s age and comorbidities.
9. How can nutritional strategies help reduce diastolic pressure specifically?
Diet plays a key role in managing increased diastolic BP. Beyond reducing sodium intake, focusing on potassium-rich foods like leafy greens, bananas, and sweet potatoes can help relax blood vessels. Magnesium, found in nuts and whole grains, also contributes to vascular dilation. Some research suggests that foods high in nitrates, such as beets and arugula, may reduce peripheral resistance and thus lower the bottom BP. When considering what causes bottom number of BP to be high, poor micronutrient intake is often an underappreciated factor that nutritional interventions can effectively address.
10. Are there new or emerging treatments for elevated diastolic blood pressure?
Yes, emerging therapies are being explored to address elevated diastolic blood pressure more effectively. These include neuromodulation techniques, such as renal denervation, which aim to reduce sympathetic nervous system overactivity. Personalized medicine approaches, using genetic profiling, are also being developed to tailor treatment for individuals whose diastolic BP elevated levels do not respond to conventional medications. Lifestyle tech, such as wearable blood pressure monitors and AI-driven stress management tools, are helping patients stay engaged in managing their condition. As our understanding of what causes high diastolic BP deepens, the treatment landscape is becoming increasingly sophisticated and individualized.
Conclusion: The Significance of Elevated Diastolic Blood Pressure and What to Do About It
High diastolic blood pressure is more than just a number—it is a vital sign that reveals much about the current and future state of cardiovascular health. Whether it presents as part of full-spectrum hypertension or as isolated diastolic hypertension, an elevated diastolic reading should never be ignored. Understanding what causes high diastolic blood pressure allows patients and healthcare providers to intervene before complications arise.
From increased vascular resistance and hormonal imbalances to lifestyle factors and genetic predispositions, the reasons for high diastolic BP are as complex as they are interconnected. Recognizing what high diastolic pressure means in the context of broader health indicators enables more personalized and effective management. Knowing which blood pressure number is more important depends on individual risk profiles, but the bottom number—the diastolic reading—is undeniably a critical component of cardiovascular assessment.
If you’ve been asking yourself, “Why is my diastolic pressure high?” or “What does high diastolic BP mean for my health?” the time to take action is now. Monitoring your blood pressure regularly, making informed lifestyle choices, and consulting with your healthcare provider can go a long way in mitigating the dangers of high diastolic blood pressure. It is a silent signal that, when heeded, can pave the way for better health outcomes and a longer, healthier life.
cardiovascular health monitoring, arterial stiffness causes, managing vascular resistance, early signs of heart strain, blood pressure tracking tips, lifestyle changes for heart health, cardiovascular risk in young adults, autonomic nervous system imbalance, sleep apnea and hypertension, mental stress and blood pressure, kidney function and blood pressure, effects of chronic stress on heart, hormone imbalance and blood pressure, nutritional strategies for hypertension, genetic factors in hypertension, inflammation and heart disease, peripheral vascular health, role of cortisol in blood pressure, early intervention in heart health, blood pressure management tools
Further Reading:
How do I bring down my diastolic blood pressure?