The silent, persistent climb of blood pressure levels despite pharmaceutical intervention is a growing concern for both clinicians and patients. For many individuals who take their prescribed antihypertensive medications diligently, the realization that their blood pressure is still high after taking medication can be both puzzling and alarming. This phenomenon, which falls under the category of resistant or uncontrolled hypertension, warrants an in-depth investigation into its root causes, clinical implications, and evidence-based strategies for effective management.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention

Understanding Uncontrolled Hypertension: When Blood Pressure Won’t Go Down
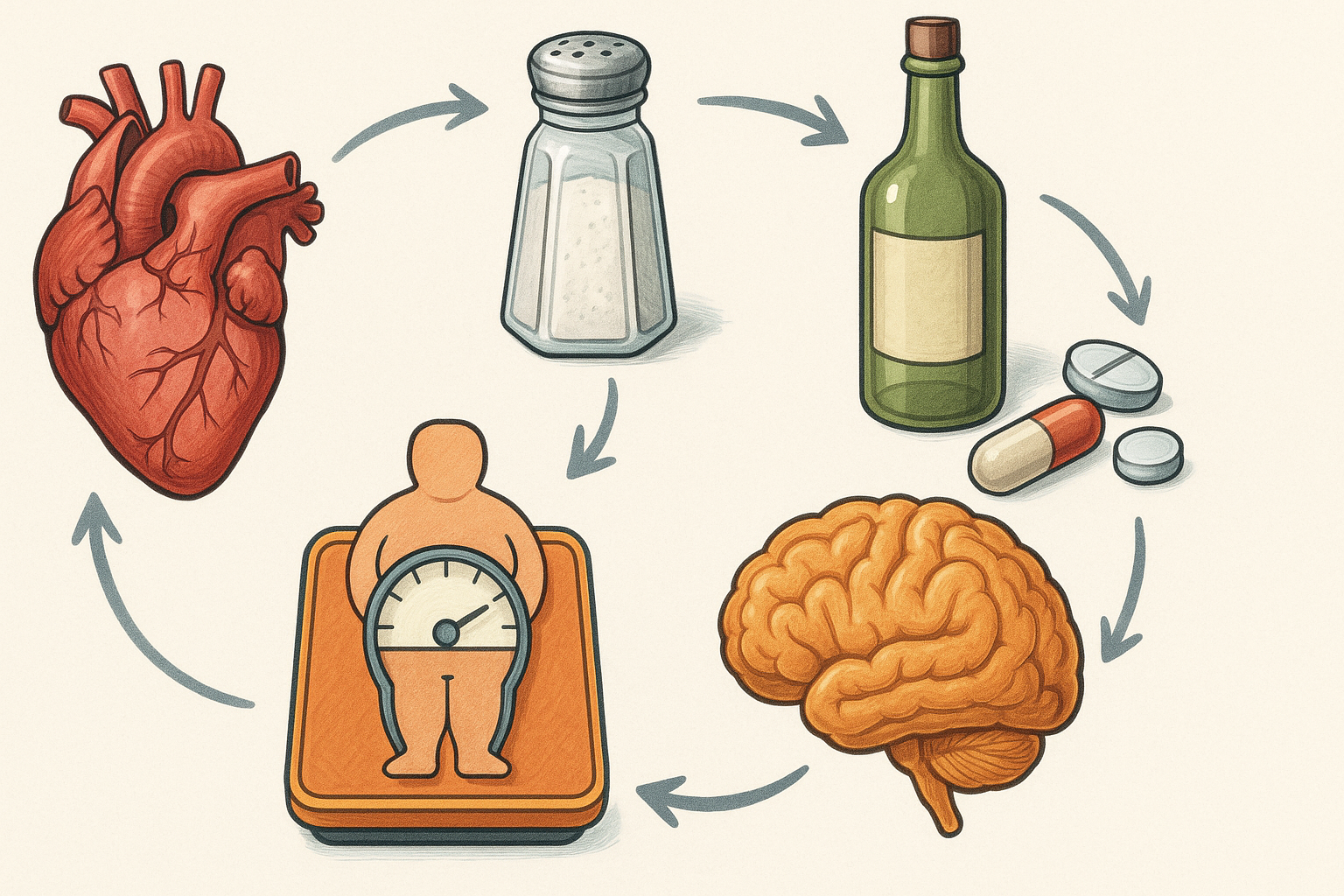
Uncontrolled hypertension, often abbreviated as uncontrolled HTN, refers to high blood pressure that remains above target levels despite adherence to treatment. This condition is typically defined by systolic blood pressure readings of 140 mm Hg or higher, or diastolic readings of 90 mm Hg or higher, even when a person is taking multiple antihypertensive agents. In some cases, patients may be on three or more medications from different classes, yet their blood pressure won’t go down. Understanding the meaning of uncontrolled hypertension is crucial because the implications extend beyond numbers on a monitor; prolonged elevation can damage vital organs, including the heart, kidneys, and brain.
Hypertension abnormally increases the workload on arterial walls and the heart, potentially leading to serious cardiovascular events like stroke and heart failure. When blood pressure not going down becomes a chronic issue, it suggests that either the treatment regimen is insufficient, or there are underlying physiological, behavioral, or secondary medical causes that must be addressed. Accurate diagnosis of uncontrolled hypertension begins with confirming adherence and excluding white coat hypertension or improper measurement techniques.
What Is Resistant Hypertension and How Is It Different?
While all resistant hypertension cases are a form of uncontrolled high blood pressure, not all uncontrolled hypertension qualifies as resistant. The distinction lies in the pharmacological intensity of treatment. Resistant hypertension is defined as blood pressure that remains above goal despite the concurrent use of three antihypertensive medications of different classes, ideally including a diuretic. Alternatively, it also includes patients who require four or more drugs to control their blood pressure, regardless of whether they reach target levels.
Resistant high blood pressure often signals an underlying complexity that goes beyond lifestyle or nonadherence. In many instances, it reflects biological resistance to treatment or an interplay of multiple comorbidities, such as chronic kidney disease, obesity, diabetes, and obstructive sleep apnea. This subset of patients poses a significant therapeutic challenge and calls for a multidimensional approach to resistant hypertension treatment that spans beyond mere prescription changes.
Exploring the Causes: Why Can’t I Get My Blood Pressure Down?
For many patients, the most pressing question is, “Why can’t I get my blood pressure down?” The answers are multifaceted. One of the leading reasons for uncontrolled hypertension is therapeutic inertia, where healthcare providers may delay necessary adjustments to medication regimens. Additionally, some patients exhibit pseudo-resistance, which can result from white coat hypertension, inaccurate blood pressure measurements, or nonadherence to prescribed therapy.
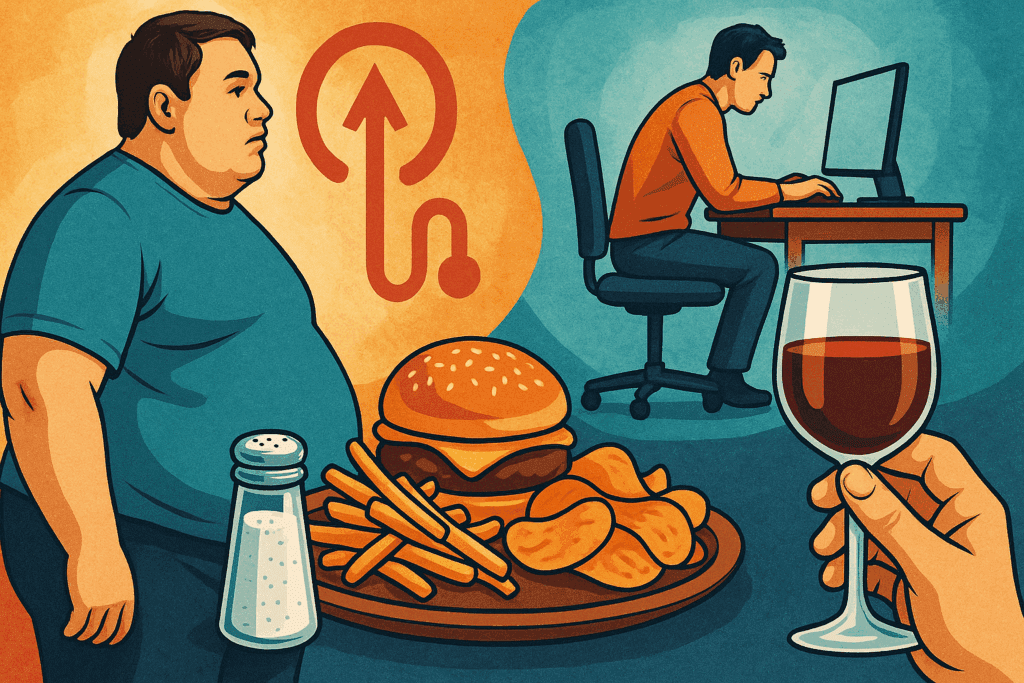
Beyond these initial considerations, secondary hypertension—where another condition drives blood pressure elevation—must be ruled out. Common causes include primary aldosteronism, renal artery stenosis, pheochromocytoma, and thyroid dysfunction. Identifying these causes is vital because treating the root condition often results in significant blood pressure improvement. Moreover, lifestyle factors such as excessive sodium intake, obesity, physical inactivity, and alcohol use can significantly interfere with blood pressure control.

Uncontrollable High Blood Pressure in the Elderly: Unique Challenges
Elderly patients face distinct challenges when it comes to managing high blood pressure, particularly when it becomes uncontrollable. Age-related changes in vascular elasticity, autonomic function, and renal capacity contribute to the difficulty in achieving optimal control. Furthermore, polypharmacy is common in this demographic, raising the risk of drug interactions and adverse effects that complicate treatment adherence.
Uncontrollable high blood pressure in the elderly often stems from both physiological resistance and increased sensitivity to medication side effects. As a result, healthcare providers must balance the urgency of reducing cardiovascular risk with the need to avoid hypotension-related complications, such as dizziness, falls, and cognitive impairment. A nuanced, individualized approach is essential, and often involves starting with lower doses, using long-acting agents, and ensuring frequent monitoring.

Persistent High Blood Pressure: When Initial Interventions Aren’t Enough
Persistent high blood pressure, despite initial interventions, often indicates a need for comprehensive reevaluation. At this stage, patients typically have tried standard medications and may have made basic lifestyle changes, such as reducing salt intake or increasing physical activity. However, these measures may not suffice if deeper issues are not addressed.
A thorough clinical reassessment should include ambulatory blood pressure monitoring to rule out white coat hypertension and identify any masked hypertension that may not be evident during office visits. Laboratory investigations can help detect underlying metabolic or endocrine abnormalities. A medication review is also vital to identify drugs that may elevate blood pressure, including NSAIDs, corticosteroids, and certain antidepressants. Addressing persistent high blood pressure often requires a layered strategy, incorporating dietary interventions like the DASH diet, supervised physical activity, stress management techniques, and sometimes, referral to a hypertension specialist.
Elevated Blood Pressure Without Hypertension: A Diagnostic Gray Area
Some individuals may present with elevated blood pressure readings without meeting the clinical criteria for hypertension. This diagnostic gray area can be challenging for both patients and clinicians. These individuals may not yet have sustained elevated readings across multiple visits or may show only intermittent spikes due to stress, pain, or physical exertion.
Elevated blood pressure without hypertension should still be taken seriously, especially if the readings are consistently approaching hypertensive levels. It serves as a warning sign for future cardiovascular risk and should prompt proactive lifestyle modifications. Moreover, in some cases, early intervention in this stage can prevent progression to full-blown resistant high blood pressure. Clinicians must remain vigilant in monitoring and guiding patients through this borderline phase, ensuring that preventive strategies are not overlooked.
Reasons for Uncontrolled Hypertension: Lifestyle, Medication, and More
There are numerous reasons for uncontrolled hypertension, ranging from medication issues to lifestyle choices and unrecognized secondary causes. One of the most common culprits is suboptimal adherence, whether due to forgetfulness, cost of medication, or side effects. Many patients discontinue or skip doses without informing their providers, leading to ineffective treatment.
Dietary habits play a substantial role as well. High sodium consumption, often hidden in processed and restaurant foods, directly contributes to resistant hypertension. Obesity and lack of physical activity further compound the problem. Stress, sleep disorders, and certain medications can all exacerbate blood pressure control issues. Addressing these factors requires open communication between patients and healthcare providers, as well as consistent follow-up and education. Sustainable change is more likely when patients understand how seemingly minor daily habits influence their condition.

Resistant Hypertension Treatment: Comprehensive and Individualized Strategies
When managing resistant hypertension, treatment must go beyond conventional approaches. A tailored plan is essential, taking into account patient-specific factors such as comorbidities, age, and genetic predispositions. For patients with blood pressure still high after taking medication, a strategic reevaluation of the current regimen is the first step. This may include optimizing doses, switching to more effective drug combinations, or adding a fourth-line agent such as spironolactone, which has shown efficacy in numerous clinical trials.
Lifestyle interventions should not be underestimated in this population. Adherence to the DASH diet, regular aerobic exercise, weight reduction, and alcohol moderation have all been shown to enhance medication effectiveness. For patients with obstructive sleep apnea, continuous positive airway pressure (CPAP) therapy may significantly reduce blood pressure levels. In some cases, interventional procedures such as renal denervation or baroreceptor activation therapy may be considered, although these are generally reserved for those who do not respond to maximal medical therapy.
Hypertension Abnormally Increases the Risk of Cardiovascular Events
Unchecked high blood pressure is one of the leading modifiable risk factors for cardiovascular morbidity and mortality worldwide. Hypertension abnormally increases the mechanical stress on blood vessels, promoting endothelial dysfunction, arterial stiffening, and accelerated atherosclerosis. These pathophysiological changes set the stage for myocardial infarction, stroke, peripheral artery disease, and chronic kidney disease.
When blood pressure not going down becomes a long-term pattern, the cumulative damage to the cardiovascular system becomes more severe. Left ventricular hypertrophy, a common consequence of sustained high pressure, increases the risk of arrhythmias and sudden cardiac death. Similarly, microvascular damage in the kidneys leads to proteinuria and gradual decline in renal function. Recognizing these downstream effects underscores the urgency of achieving and maintaining optimal blood pressure control, especially in those with resistant hypertension.
Addressing Psychological and Behavioral Barriers in Hypertension Management
Beyond physiology and pharmacology, behavioral and psychological factors can significantly influence blood pressure control. Depression, anxiety, and chronic stress not only elevate sympathetic nervous system activity but also interfere with a patient’s ability to adhere to treatment recommendations. Cognitive behavioral therapy, mindfulness-based stress reduction, and other psychological interventions can play a supportive role in the management of resistant high blood pressure.
Effective communication between providers and patients is also critical. Patients who feel heard and involved in their treatment decisions are more likely to adhere to medication regimens and lifestyle changes. Educational efforts should be personalized, addressing specific concerns such as “why can’t I get my blood pressure down” with evidence-based guidance and empathy. Behavioral coaching and mobile health technologies offer additional support in helping patients stay on track.
The Role of Genetics and Pharmacogenomics in Resistant High Blood Pressure
Emerging research suggests that genetic factors may play a role in resistant hypertension. Variations in genes involved in the renin-angiotensin-aldosterone system, sodium transport, and vascular tone may influence an individual’s response to antihypertensive medications. While pharmacogenomic testing is not yet standard practice in managing high blood pressure, it holds promise for the future of personalized medicine.
Understanding an individual’s genetic profile could potentially guide medication selection and dosing, improving treatment outcomes and minimizing side effects. Ongoing clinical trials are investigating the feasibility and cost-effectiveness of incorporating genetic screening into hypertension management. For patients with blood pressure that won’t go down despite exhaustive conventional treatments, this avenue may eventually offer new hope.
How to Approach Follow-Up and Long-Term Monitoring
Managing resistant and persistent high blood pressure requires ongoing follow-up and monitoring. Regular blood pressure checks, either in-office or through home monitoring, allow for timely detection of trends and adjustments in treatment. For patients with complex medical histories or multiple comorbidities, specialist referral to a hypertension clinic may be warranted.
Long-term management should also include periodic reassessment of lifestyle habits, medication tolerability, and organ function. Laboratory tests to monitor electrolytes, renal function, and glucose levels can help prevent complications from both hypertension and its treatments. Ultimately, effective follow-up hinges on a collaborative, multidisciplinary approach that places the patient at the center of care.
Frequently Asked Questions: Understanding Persistent and Resistant High Blood Pressure
What lifestyle changes are most effective when blood pressure is still high after taking medication?
When facing blood pressure still high after taking medication, many patients wonder if lifestyle changes can make a measurable impact. Research shows that consistent aerobic exercise, such as brisk walking or swimming for 30 minutes most days, significantly complements pharmacologic interventions. Beyond physical activity, reducing sodium intake to under 1,500 mg per day and incorporating potassium-rich foods can help regulate vascular tension. Stress reduction is another critical element—practices like biofeedback, progressive muscle relaxation, and guided meditation have demonstrated notable effects on lowering persistent high blood pressure. Ultimately, these behavioral modifications are essential, especially in resistant hypertension treatment plans, where medication alone may fall short.
Is it possible for elevated blood pressure without hypertension to still pose long-term risks?
Yes, even elevated blood pressure without hypertension can contribute to long-term cardiovascular damage. This condition, often termed prehypertension or borderline hypertension, is associated with early vascular changes, including endothelial dysfunction and arterial stiffening. Though a formal hypertension diagnosis may not be warranted initially, this pattern of intermittently high readings increases the risk of progression to full-blown resistant high blood pressure. Early intervention with dietary and lifestyle changes can delay or even prevent the need for medication. Therefore, monitoring and addressing elevated readings proactively can reduce the eventual burden of uncontrolled HTN.
How does mental health affect persistent high blood pressure and treatment outcomes?
Mental health plays a surprisingly strong role in the persistence of elevated blood pressure. Chronic stress, anxiety disorders, and untreated depression stimulate the sympathetic nervous system and trigger inflammatory responses that can undermine otherwise effective treatment. Patients who report that their blood pressure won’t go down often experience psychological barriers that interfere with lifestyle consistency and medication adherence. Integrating mental health support, whether through therapy, support groups, or behavioral coaching, into resistant hypertension treatment plans can help resolve cases where physiological strategies alone have failed. Addressing these components creates a more holistic model of care that supports long-term success.
What is the difference between white coat hypertension and uncontrolled HTN, and why does it matter?
White coat hypertension refers to elevated blood pressure readings that occur only in clinical settings, while readings at home remain normal. In contrast, uncontrolled HTN denotes blood pressure that remains elevated both at home and in medical environments, indicating a genuine failure of regulation. Distinguishing between these two is critical because treatment approaches differ significantly. Relying on office measurements alone could lead to overtreatment of benign cases or undertreatment of true resistant hypertension. Ambulatory or home monitoring provides a more accurate picture, helping to identify whether blood pressure not going down reflects real physiological resistance or merely situational stress.
Why is resistant high blood pressure more common in patients with kidney disease?
Resistant high blood pressure is disproportionately prevalent among individuals with chronic kidney disease due to the complex interplay between the kidneys and blood pressure regulation. Damaged kidneys have a diminished ability to filter sodium and water, which increases fluid volume and raises blood pressure. Moreover, impaired kidney function disrupts the renin-angiotensin-aldosterone system, a hormonal cascade responsible for maintaining vascular tone and fluid balance. This disruption often leads to a feedback loop where hypertension abnormally increases the workload on the kidneys, further worsening function. Effective management in these patients requires careful titration of medications, dietary restrictions, and sometimes dialysis to address fluid overload.
What are emerging technologies that help manage resistant hypertension?
Technology is advancing rapidly in the field of hypertension management, especially for resistant cases. Wearable blood pressure monitors that track 24-hour patterns allow clinicians to tailor treatment based on real-time data rather than sporadic office readings. Additionally, AI-driven apps can remind patients to take their medications, log lifestyle behaviors, and alert providers to early signs of worsening control. Devices like baroreceptor stimulators, which modulate nervous system responses, show promise in trials for individuals whose blood pressure won’t go down despite aggressive treatment. These technologies empower patients and providers alike, offering precision-based approaches to conditions like persistent high blood pressure and uncontrolled HTN.
How does age influence the reasons for uncontrolled hypertension?
Age adds complexity to blood pressure regulation for several reasons. In older adults, arteries become less elastic, reducing their ability to buffer pressure surges. Additionally, age-related changes in kidney function and autonomic regulation affect the body’s ability to maintain homeostasis. This explains why uncontrollable high blood pressure in the elderly is especially challenging to treat. Polypharmacy, common in this population, further complicates treatment by increasing the risk of drug interactions that can blunt medication efficacy. As a result, the reasons for uncontrolled hypertension in older adults are often multifactorial, requiring a nuanced, low-risk strategy that balances efficacy with safety.
Why do some patients experience blood pressure not going down even after following medical advice?
Even when patients meticulously follow medical advice, some still report blood pressure not going down. This phenomenon may arise due to undiagnosed secondary causes such as primary aldosteronism, pheochromocytoma, or Cushing’s syndrome. In other cases, subtle issues like inconsistent medication absorption due to gastrointestinal disorders can interfere with treatment efficacy. Genetic variability in drug metabolism also plays a role, where certain individuals may not respond to standard doses. Recognizing these hidden barriers can transform resistant hypertension treatment outcomes by guiding specialists toward personalized solutions that go beyond surface-level adherence.
What role does sleep play in resistant hypertension and its treatment?
Sleep disorders, particularly obstructive sleep apnea (OSA), are frequently overlooked contributors to resistant hypertension. Repeated nocturnal hypoxia from OSA activates stress hormones that elevate nighttime and daytime blood pressure. Patients with resistant high blood pressure often show improvement when sleep apnea is diagnosed and managed with therapies like CPAP. Beyond OSA, poor sleep hygiene and chronic insomnia can also worsen sympathetic activation. Incorporating sleep assessments into hypertension evaluations adds a crucial layer to understanding why some patients present with persistent high blood pressure despite adequate treatment.
Can social and environmental factors contribute to what is the cause of uncontrolled high blood pressure?
Yes, social determinants of health significantly impact what is the cause of uncontrolled high blood pressure for many individuals. Living in areas with limited access to healthy food, safe exercise spaces, or quality healthcare services creates barriers to effective management. Financial instability can lead to medication nonadherence, while environmental stressors like noise pollution and community violence exacerbate stress-related blood pressure spikes. These factors are especially relevant in underserved communities where resistant hypertension is more prevalent. Addressing them requires systemic change alongside individual care, as clinical solutions alone may not fully resolve persistent high blood pressure rooted in structural inequality.
Bringing It All Together: Overcoming Resistant Hypertension with Insight and Action
Resistant hypertension and persistent high blood pressure present some of the most formidable challenges in modern cardiovascular care. Yet these conditions are far from insurmountable. For patients facing the disheartening reality of blood pressure still high after taking medication, the path forward begins with knowledge, clarity, and a commitment to tailored, evidence-based care. Understanding what is the cause of uncontrolled high blood pressure, whether rooted in physiology, lifestyle, or external factors, empowers both patients and providers to take informed action.
Effective resistant hypertension treatment requires a multifaceted approach. This includes optimizing drug therapy, addressing behavioral barriers, investigating secondary causes, and leveraging lifestyle interventions. It also demands regular monitoring and, when necessary, the integration of emerging technologies and specialist expertise. By recognizing the many reasons for uncontrolled hypertension and implementing comprehensive strategies, we can reduce the burden of cardiovascular disease and improve quality of life for those most at risk.
In an era where hypertension abnormally increases the risk of life-altering complications, no case of blood pressure not going down should be accepted as inevitable. With the right tools, insights, and collaboration, even the most resistant high blood pressure can be brought under control—restoring health, hope, and longevity.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Understanding Resistant Hypertension: Causes, Symptoms, and Risk Factors